KTS often presents a challenging scenario due to the rarity of the condition, multiple systems involved and varied manifestations from patient to patient which makes it essential to individualize treatment goals based on the severity, functional demands, and associated complications.
Dr. Sahil Sanghavi, Department of Orthopaedics, Sancheti Institute for Orthopaedics and Rehabilitation, Pune, Maharashtra, India. E-mail: sahil.sanghavi@hotmail.com
Introduction: Klippel–Trenaunay syndrome (KTS) is rare and sporadic disorder. Clinical manifestation of KTS is heterogenous. KTS patients often suffer degenerative joint disease at an early age. Arthroplasty performed in extremities with KTS is challenging due to vascular malformations and increased risk of intraoperative and post-operative complications.
Case Report: We report two patients of KTS with varied musculoskeletal manifestations with one patient treated operatively and one patient managed conservatively, both predominantly affecting the hip joint. We present this report due to rarity of presentation and to discuss varied articular manifestations in two patients with KTS. Both patients fulfilled the criteria and were diagnosed to have KTS. The first patient was a 36 year-old woman who presented with left hip pain since 3 years which was progressively worsening. As this patient did not have any vascular malformations around the hip, a left total hip arthroplasty was planned and successfully executed. The second patient was a 42-year-old gentleman who had polyarticular involvement, mainly affecting the hip and knee. Due to the severe presentation of a subluxated hip, vascular malformations, gross knee laxity, and the patient’s occupational demands; it was decided to opt for conservative management in this patient.
Conclusion: KTS often presents a challenging scenario due to the rarity of the condition, multiple systems involved and varied manifestations from patient to patient which makes it essential to individualize treatment goals based on the severity, functional demands, and associated complications.
Keywords: Adult, hip, knee, Klippel–Trenaunay syndrome, arthroplasty.
Klippel–Trenaunay syndrome (KTS) is rare with a prevalence rate of 1/20,000–40,000 live births [1]. It is a congenital condition affecting bone and soft-tissue structures, which is characterized by a triad of capillary vascular malformations (port wine stain), venous malformations, and soft-tissue and/or bony hypertrophy [2-4]. It mainly affects one limb, commonly the lower limb in 70% of cases [5]. It is not obvious at birth but becomes visible with growth. Diagnosis may not be confirmed until the limb hypertrophy or venous varicosities become more noticeable [6]. There is controversy regarding treatment of orthopedic conditions associated with KTS due to high risk of hemorrhage during surgery and increased incidence of infection, pulmonary embolism (14%), and deep vein thrombosis (16%) [7].
We report two patients of KTS with varied musculoskeletal manifestations with one patient treated operatively and one patient managed conservatively, both predominantly affecting the hip joint.
Patient 1
A 36-year-old lady presented with complaints of left hip pain and difficulty in standing, walking, and climbing stairs. Pain was insidious in onset and gradually progressive. On examination, the patient was noted to have hypertrophy of the left lower limb, diffuse hyperpigmented patches, and varicose veins. Range of movement of the left hip joint was restricted in all planes. Plain radiographs of pelvis with both hips showed involvement of the left hip joint with irregular margins of the articular surface of the femoral head, areas of sclerosis, and a large cystic lesion (Fig. 1). Based on these clinicoradiological findings and as per the criteria, the patient was diagnosed to have KTS and surgery in the form of left total hip arthroplasty (THA) was planned.
Considering the diagnosis of KTS, there was a high suspicion of underlying vascular malformations that could pose a challenge for surgery, and hence, the patient was advised magnetic resonance (MR) imaging of the pelvis with both hips. MR imaging was suggestive of changes of avascular necrosis in the left femoral head (Ficat Arlet Grade 2–3). Joint effusion with synovial thickening was noted. Patchy hypointense signal in right pelvic bone, right proximal femur, and sacrum were noted and were suggestive of red marrow conversion. No vascular malformations were noted.
Physician, anesthetist, and cardiologist opinion was taken preoperatively for fitness and the patient was posted for left THA with ceramic-on-ceramic bearing surface. Adequate blood products were reserved. The patient was given spinal anesthesia, and the surgery was performed through the posterior approach. Intraoperative course was uneventful and estimated blood loss was 350 mL. Pre-operative hemoglobin was 10.9 g/dL and post-operative hemoglobin was 10.2 g/dL. The patient was mobilized on Day 1 and was allowed full weight-bearing walking with walking frame support (Fig. 2). Perioperative course was uneventful. At 1-year follow-up, the patient was asymptomatic and was able to carry out all her activities of daily living.
Patient 2
A 42-year-old gentleman presented with complaints of right hip pain since 1 year, limp while walking and difficulty in carrying out activities of daily living. He was using a cane for ambulation. There was diffuse right lower limb hypertrophy. Patchy areas of hyperpigmentation were present with multiple broad irregular soft-tissue swellings throughout the right lower limb. Active straight leg raise of the right lower limb was not possible. The right hip had flexion up to 60°, abduction of 30°, and exaggerated rotations. Telescopy test was positive. Right knee had hyperextension of about 30°. Lachman and anterior drawer tests were positive. Sensations were intact over all dermatomes. Reflexes were normal.
On plain radiographs of pelvis with both hips, the right hemipelvis appeared dysplastic. There was presence of a pseudo-acetabulum superior to the native acetabulum on the right side. There was subluxation of the femoral head along with complete loss of sphericity and a flat remnant giving the appearance similar to that of a “mortar and pestle” hip seen in tuberculosis. The right femur appeared hypertrophic and broad compared to the other side. Radiographs of the right knee also showed a dysplastic appearance with mild flattening of the femoral condyles. There was also irregularity seen over the posterior cortex of the distal femur. The right proximal tibiofibular joint also appeared to be involved along with diffuse irregularity of the bony contour of the tibia. MR imaging of the right thigh showed a well-defined focal lesion extending from the pelvis up to the knee, predominantly involving posterior and lateral aspects of the thigh with intra-muscular extension. The MR report mentioned this as a likely possibility of plexiform neurofibromatosis with a less likely possibility of a hemangioma. A soft-tissue lesion was noted along the lateral aspect of the hip joint in sub cutaneous soft-tissue which was suspected to be a fibroma. Based on these clinicoradiological findings and as per the criteria, the patient was diagnosed to have KTS. Based on the overall condition of the patient, multiple joint involvement, especially the gross laxity of the ipsilateral knee coupled with the manual labor involved as a part of his occupation, it was decided to manage the patient conservatively. The patient was advised an ischial weight-bearing orthosis with stick support. At follow-up of 1.5 years, the patient was able to manage activities of daily living with minimal pain.
Vascular malformations in KTS lead to secondary musculoskeletal symptoms such as hypertrophy of limb and swelling of limb due to blood stasis. Swollen soft tissues stimulate the periosteum causing compression of blood vessels and lymphatic vessels, leading to altered vascularity in bones. Chronic stimulation causes hyperactivity of periosteal osteoblasts and results in bone hypertrophy [8]. Bone hypertrophy in turn results in limb length discrepancy, secondary pelvic tilt, scoliosis, abnormal gait, joint contractures, and degenerative joint disease [8]. KTS is a commonly painful condition, with degenerative joint disease being one of the many causes of pain [1]. Commonly, it is a monoarticular arthropathy because the pathology is confined to one limb. Diagnosis of KTS is based on the following criteria, that is, characterized by two major features (at least 1 from group “a,” which should always include either a1 or a2, and at least 1 from group “b”) [9].
- Congenital vascular malformations
- Capillary malformations (CMs). This includes port-wine
- Venous malformations (VMs). This includes hypoplasia or aplasia of veins, persistence of fetal veins, varicosities, hypertrophy, tortuosity, and valvular
- Arteriovenous malformations (AVMs). This includes only very small AVMs or arteriovenous fistula.
- Lymphatic malformation (LM). This includes any
Localization: CM can be located anywhere on the body. Although location on the face is rare, AVM, VM, and LM are mainly located on the extremities and adjacent parts of the trunk (pelvis, shoulder), expressed forms of KTS may also be present elsewhere such as bladder, rectum, lower GI tract, penis, uterus, vulva, vagina, liver, kidneys, lung, and spine. AVM, VM, and LM are not located on the face or in the brain.
- Disturbed growth
- Disturbed growth of bone in the length or
- Disturbed growth of soft tissue in the length or girth. The disturbed growth includes:
- Hypertrophy (frequent) of a small body part (isolated finger [macrodactyly]) or larger body part (total limb, half of the total body).
- Hypotrophy (infrequent) of a small or larger body
Localization: The growth disturbance is frequently present at the same site as the vascular malformation(s) and infrequently at another site. Other, non-obligatory and non-essential symptoms that are still in concert with the diagnosis are:
- Limb anomalies: polydactyly, syndactyly, camptodactyly, and clinodactyly.
- Positional limb defects: scoliosis, hip dislocation, talipes, metatarsus
- Autonomous dysfunctioning: skin atrophy, hyperhidrosis (increased sweating).
- Complications: ulceration, cellulitis, thrombophlebitis, thrombosis, emboli, hemorrhages, and
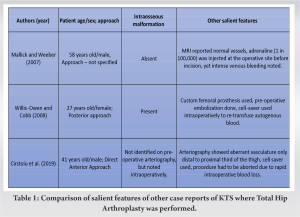
Hip involvement in KTS can be disabling and affect the quality of life of the patient. Surgical management in the form of THA can be challenging due to the presence of vascular malformations that may hinder the surgical approach. We found only three reported cases in English literature with KTS involving the hip joint [5,7,10] (Table 1). All these patients were planned for THA. In the case reported by Cirstoiu et al., pre-operative arteriography was performed to identify arteriovenous (AV) malformations [7]. This patient also had two previous abandoned attempts at THA using the lateral approach, and hence based on arteriography findings an anterior approach was chosen for the subsequent attempt. However, surgery had to be abandoned intraoperatively due to profound bleeding from synovial AV malformations and intraosseous sources that had not been recognized on pre-operative conventional arteriography. To combat the risk of bleeding from malformations, Willis-Owen and Cobb used pre-operative embolization, cell saver intraoperatively, re-transfusion of salvaged autogenous blood, and a CAD-CAM prosthesis to successfully carry out their THA [5]. Similarly, Mallick and Weeber used adrenaline, erythropoietin, and autologous blood transfusion to successfully carry out their staggered bilateral THA in a patient with KTS [10]. Intense venous bleeding despite the use of adrenaline at the incision site was seen. Standard practice says that any form of bony surgery should be avoided in KTS due to high risk of uncontrollable hemorrhage, but extensive pre-operative workup such as CT angiography and MR angiography will be helpful in identifying the location of vascular malformation. This will help surgeons to choose the appropriate approach, that is, anterior/posterior/lateral, so as to avoid the vascular malformation and thereby minimize bleeding. If malformation of superficial vessels is present, superficial branches can be treated with sclerotherapy. This should be done 6 weeks before planning for the replacement surgery [2]. In our patient, even though vascular malformations had not been recognized, we encountered significant bleeding from the soft tissues. A careful surgical dissection along with electrocautery and ligation can limit blood loss, but intraosseous malformations can be difficult to manage intraoperatively.
KTS often presents a challenging scenario due to the rarity of the condition, multiple systems involved and varied manifestations from patient to patient which makes it essential to individualize treatment goals based on the severity, functional demands, and associated complications. KTS patients have similar pathophysiology of arthropathy to hemophiliacs. Although it is associated with many complications and risks with few reports suggesting caution for arthroplasty and preference for conservative management, arthroplasty is an option to treat joint involvement in KTS patients with careful pre-operative planning with regards to AV malformations and weighing the benefit-risk ratio of surgery.
Orthopedic surgeons should be well versed with the diagnostic criteria of KTS, its varied manifestations, and anticipate the surgical challenges of this entity.
References
- 1.Lee A, Driscoll D, Gloviczki P, Clay R, Shaughnessy W, Stans A. Evaluation and management of pain in patients with Klippel-Trenaunay syndrome: A review. Pediatrics 2005;115:744-9. [Google Scholar]
- 2.Labott JR, Wyles CC, Houdek MT, Tollefson MM, Driscoll DJ, Shaughnessy WJ, et al. Total knee arthroplasty is safe and successful in patients with klippel-trénaunay syndrome. J Arthroplasty 2019;34:682-5. [Google Scholar]
- 3.Pavone P, Marino L, Cacciaguerra G, Di Nora A, Parano E, Musumeci G, et al. Klippel-trenaunay syndrome, segmental/focal overgrowth malformations: A review. Children (Basel) 2023;10:1421. [Google Scholar]
- 4.Asghar F, Aqeel R, Farooque U, Haq A, Taimur M. Presentation and management of klippel-trenaunay syndrome: A review of available data. Cureus 2020;12:e8023. [Google Scholar]
- 5.Willis-Owen CA, Cobb JP. Total hip arthroplasty in klippel-trenaunay syndrome. Ann R Coll Surg Engl 2008;90:W6-8. [Google Scholar]
- 6.Hu P, Zhang GY, Wang Y, Cheng Y, Wang LL. Klippel-Trenaunay syndrome in combination with congenital dislocation of the hip. J Chin Med Assoc 2013;76:229-31. [Google Scholar]
- 7.Cirstoiu C, Cretu B, Sandu C, Dorobat B, Neagu A, Serban B. Failed attempt of total hip arthroplasty in a patient with klippel-trenaunay syndrome: A case report. JBJS Case Connect 2019;9:e0103. [Google Scholar]
- 8.Joseph EG, Ernest EP, Dietz MJ. Complicated total knee arthroplasty in a patient with klippel-trenaunay-weber syndrome: A case report. JBJS Case Connect 2017;7:e73. [Google Scholar]
- 9.Oduber CE, Van Der Horst CM, Hennekam RC. Klippel-Trenaunay syndrome: Diagnostic criteria and hypothesis on etiology. Ann Plast Surg 2008;60:217-23. [Google Scholar]
- 10.Mallick A, Weeber AC. An experience of arthroplasty in klippel-trenaunay syndrome. Eur J Orthop Surg Traumatol 2007;17:97-9. [Google Scholar]