Heterotopic ossifications should be considered as a possible cause of vascular compromise in patients after intertrochanteric femur fracture fixation
Dr. Gennadiy Busel, Department of Orthopaedic Surgery, Mercy Hospital, Coon Rapids, Minnesota; NorthStar Trauma Network, Saint Paul, Minnesota. E-mail: genebusel@gmail.com
Introduction: Intertrochanteric (IT) hip fractures are increasing in prevalence due to a rise in the aging population. Cephalomedullary nailing is one of the treatment options and is becoming a treatment of choice worldwide. Complications after a hip fracture have been extensively studied and widely published. Despite numerous publications, we report a unique complication not previously seen in literature.
Case Report: This case demonstrates the rare phenomenon of proximal femur heterotopic ossification (HO) after cephalomedullary nailing of an IT femur fracture causing a femoral artery pseudoaneurysm.
Conclusion: Proximal femoral HO is a rare phenomenon after cephalomedullary nailing that, in this case, presented a serious complication requiring combined surgical intervention from both vascular surgery and orthopedic surgery teams. As far as the authors know, this is the only such incident in the literature.
Keywords: Heterotopic ossification, hip fracture, cephalomedullary nail, femoral artery, pseudoaneurysm.
Hip fractures are common given the increasing aging population with some reports as high as 18% of women and 6% of men [1]. Hip fracture incidence is projected to increase globally to 4.5 million cases annually in 2050 from 1.6 million cases in 1990 [1]. Intertrochanteric (IT) hip fractures represent a large portion of these injuries and lead to high societal, financial, and personal burdens. IT fractures have been extensively studied and demonstrate a high rate of complications resulting from a decrease in mobility. While numerous medical complications are published in the literature, vascular complications are uncommon, mostly as a result of iatrogenic injury, with two case reports of superior gluteal artery injury [2, 3], and a single case report of a deep femoral artery injury [4], but this was from the insertion of a distal interlocking screw. Furthermore, we have not been able to find a case report of a pseudoaneurysm as a result of post-operative heterotopic ossification (HO) after hip fracture fixation. Here, we present a case of a common femoral artery pseudoaneurysm due to HO after cephalomedullary nailing of an IT femur fracture. Pseudoaneurysms are defined as a persistent cavity with communication to an artery through disruption on its wall. The persistent deficit allows for ongoing communication of blood; however, a fibrin shell, also known as the false aneurysmal sac, prevents an expanding hematoma [5, 6]. The common femoral artery is the most common site of pseudoaneurysms with etiologies including iatrogenic injury after endovascular procedures, anastomotic breakdown following arterial reconstructive surgery, infection, and trauma [5]. A variety of treatment options exist depending on pseudoaneurysm characteristics and the patient clinical condition ranging from ultrasound-guided compression, ultrasound-guided thrombin injection, and surgical repair. Few cases of pseudoaneurysm due to HO have been reported in the literature [5], and none as a result of inter-trochanteric hip fracture. HO is an atypical but not uncommon complication following orthopedic surgery. It may result from neurologic injury, local tissue trauma, or post-surgically and generally presents as a painless entity which may possibly limit motion of the involved joint [7]. HO about the hip is a relatively common and known complication following total hip arthroplasty through a posterior approach, with rates of 2–7% [8] and is more common in patients with ankylosing spondylitis or Paget’s disease [9]. In the realm of trauma, HO around the hip is typically seen with the Kocher-Langenbeck approach to the acetabulum due to soft-tissue injury as a result of the traumatic event. Anterior approach to the femoral neck fracture fixation, on the other hand, has been shown to have a much lower rate of HO. When comparing anterior versus posterior approaches for total hip arthroplasty, the anterior approach has a significantly lower rate of clinically significant HO, with 3% in the direct anterior group versus 7.5% in the posterior group [10]. Diagnosis is generally made with plain films, and maturity of the lesion is confirmed with X-ray. Symptomatic HO that limits functional joint movement can be treated with excision after maturation of the lesion. In high-risk patients, attempted prophylaxis with radiation or indomethacin may be considered.
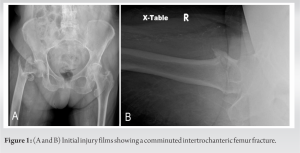
Informed consent was obtained from the patient to use case history, demographics, and photographs for publication of the case report. An 80-year-old female presented to the emergency department after a ground-level fall. After an appropriate workup, she was found to have a right IT femur fracture (Fig. 1a and b).
She then underwent uneventful short cephalomedullary nailing of the fracture the following day on a fracture table. After initial reduction, a bone hook was introduced through a lateral stab incision. The bone hook was placed over the medial calcar in the standard fashion to obtain appropriate alignment before instrumentation (Fig. 2a).
The reduction was held with provisional threaded wires outside of the planned path of the nail (Fig. 2b). Fluoroscopic images were obtained demonstrating appropriate reduction and final instrumentation (Fig. 2c and d). She was discharged and was progressing well with rehab and had returned to her baseline level of function and ambulation without assistive devices by 6 weeks postoperatively (Fig. 3a and b).
The patient was presented to the emergency department after approximately 3 months postoperatively with a 5-day history of severe, intermittent right groin pain. Initially, the pain was 10/10 and cramping in nature which subsequently resolved over several hours. The pain continued to wax and wane over several days. The pain was minimal at rest, but worse with movement, significantly limiting any hip range of motion. On the day of presentation, the patient had multiple episodes of pain that were increasing in frequency, therefore, prompting her visit to the emergency department for evaluation.
Upon presentation to the emergency department nearly 12 weeks after the initial fixation, orthopedic trauma and vascular surgery were consulted. Repeat X-rays were obtained demonstrating a healed IT hip fracture (Fig. 4a and b). The patient was found to have a prominent right femoral pulse as well as ecchymosis and tenderness to palpation in the medial thigh. The thigh was soft. Sensation and motor examination to the right lower extremity were normal. The patient had a monophasic right dorsalis pedis Doppler signal and a multiphasic right posterior tibial artery Doppler signal. Her left lower extremity examination was normal, also with a monophasic right dorsalis pedis Doppler signal and a multiphasic right posterior tibial artery Doppler signal.
Computed tomography angiogram of the right lower extremity demonstrated active extravasation from the right posterolateral common femoral artery with a pseudoaneurysm from exuberant HO arising from her previous fracture site (Fig. 5). The patient was taken to the operating room for planned right external iliac to common femoral artery interposition repair with vascular surgery and removal of HO with the orthopedic trauma team. The procedure began with proximal control of the external iliac artery through a retroperitoneal incision. Then, a longitudinal incision was made over the right groin with dissection carried down to the right common femoral artery and femoral bifurcation. The artery was dissected under the inguinal ligament. There was a clear defect in the posterior aspect of the artery, which given the location underneath the ligament and the posterior aspect of the pseudoaneurysm, was considered best treated with an interposition graft. The conduit was an 8 mm Dacron tunneled between the two incisions. The anastomosis was done in an end-to side functional end-to-end fashion at both ends. 4–0 prolene suture was used on the iliac anastomosis and 5–0 prolene suture on the femoral anastomosis (Fig. 6).
After performing arterial repair, the orthopedic surgery team performed resection of the HO from the base of the lesion at the lesser trochanter, releasing the HO from the surrounding iliopsoas tendon and periosteum. The base was truncated using a ¼” osteotome (Fig. 7). The base was further cleaned using a rongeur to prevent any irritation of the graft. Complete excision was confirmed through intraoperative fluoroscopy (Fig. 8). Incisions were then irrigated and closed in multiple layers. The patient was discharged from the hospital on post-operative day 3 without any complications. She was discharged on a 2-week taper of indomethacin to help prevent the recurrence of the HO as well as aspirin 81 mg daily for deep venous thrombosis prophylaxis.
At most recent clinic follow-up nearly 3 months postoperatively (Fig. 9), the patient has returned to walking without assistive devices, wounds have fully healed, and no recurrence of symptoms have been noted. A duplex ultrasound revealed a patent bypass graft without significant stenosis and normal ABI’s bilaterally.
Femoral pseudoaneurysm not related to trauma or iatrogenic injury is relatively rare. Only a few cases of spontaneous femoral pseudoaneurysm have been reported [2]. To our knowledge, this is the first reported case of a common femoral artery pseudoaneurysm related to HO after cephalomedullary nailing of an IT femur fracture. One prior case report describes a pseudoaneurysm in the deep femoral artery from HO after penetrating trauma to the thigh with stenting of the SFA that developed a deep femoral artery pseudoaneurysm 8 years later [1]. In this patient without penetrating trauma to the region and without significant risk factors for the development of HO, this case presents a curious and thankfully rare phenomenon of vascular compromise following routine hip nailing. It is possible that the introduction of the bone hook, seen in Fig. 2a, caused additional trauma, resulting in HO formation. This technique is commonly utilized to aid in reduction and is introduced over the anterior proximal femur staying directly on bone without previously reported complication. Caution should always be exercised when introducing reduction aids around the proximal femur.
Cephalomeduallary nailing for IT hip fractures is one of the most commonly performed surgeries. These cases are performed not only by orthopedic traumatologists in academic centers but in most community hospitals worldwide by orthopedic surgeons with various specialty backgrounds and training. While heterotopic bone formation can be seen after fracture of the proximal femur, this is the only report of HO causing a pseudoaneurysm requiring surgical intervention in literature. Consideration should be made for this rare complication with patients following up with groin swelling and unusual pain symptoms after hip fracture fixation.
Proximal femoral HO is a rare phenomenon after cephalomedullary nailing that, in this case, presented a serious complication requiring combined surgical intervention from both vascular surgery and orthopedic surgery teams. As far as the authors know, this is the only such incident in the literature.
References
- 1.Veronese N, Maggi S. Epidemiology and social costs of hip fracture. Injury 2018;49:1458-60. [Google Scholar]
- 2.Carroll C, Warren M, Nammour M, Taillac H, Mautner J. Superior gluteal artery bleed after cephalomedullary nail fixation. Ochsner J 2020;20:339-42. [Google Scholar]
- 3.Ward JP, Strauss EJ, Tejwani NC. Injury to the superior gluteal artery during intramedullary fixation of an atypical subtrochanteric stress fracture - A case report. Bull Hosp Jt Dis (2013) 2013;71:297-300. [Google Scholar]
- 4.Yoon HK, Oh HC, Park J, Oyunbat C, Kim T. Rupture of the deep femoral artery during proximal femoral nailing following an intertrochanteric fracture: A case report. Hip Pelvis 2016;28:54-9. [Google Scholar]
- 5.Ge J, Wang T, Zhao J, Lu S, Wang J, Yuan D. Fracture of a covered stent-graft due to heterotopic ossification of residual hematoma after endovascular treatment of superficial femoral artery pseudoaneurysm: A case report. Medicine (Baltimore) 2021;100:e26612. [Google Scholar]
- 6.Silwal P, Karmacharya RM, Vaidya S, Shrestha S, Adhikari MM. Spontaneous common femoral artery pseudoaneurysm: A case report. JNMA J Nepal Med Assoc 2022;60:310-3. [Google Scholar]
- 7.Shehab D, Elgazzar AH, Collier BD. Heterotopic ossification. J Nucl Med 2002;43:346-53. [Google Scholar]
- 8.Riegler HF, Harris CM. Heterotopic bone formation after total hip arthroplasty. Clin Orthop Relat Res 1976;117:209-16. [Google Scholar]
- 9.Kjaersgaard-Andersen P, Ritter MA. Prevention of formation of heterotopic bone after total hip arthroplasty. J Bone Joint Surg Am 1991;73:942-7. [Google Scholar]
- 10.Newman EA, Holst DC, Bracey DN, Russell GB, Lang JE. Incidence of heterotopic ossification in direct anterior vs posterior approach to total hip arthroplasty: A retrospective radiographic review. Int Orthop 2016;40:1967-73. [Google Scholar]