Bipolar hemiarthroplasty is a good modality of treatment in unstable intertrochanteric femur fracture chosen for elderly patients with osteoporosis and comminuted intertrochanteric fracture in which the strength of internal fixation is doubtful with chances of failure and those who need early mobilization to avoid problems with recumbency. Early mobilization is impossible with internal fixation, especially in comminuted fractures.
Dr. Shubham P. Vaidya, Department of Orthopaedics at Mahatma Gandhi Medical College and Research Institute, Sewagram, Wardha, India. E-mail: shubhamvaidya1102@gmail.com
Objective: The objective of this study was to compare the outcomes of primary cemented bipolar hemiarthroplasty with proximal femoral nail (PFN) osteosynthesis as a management modality in unstable fractures of the intertrochanteric femur.
Introduction: Intertrochanteric fractures also referred to as extracapsular fractures occur in the area between the greater and lesser trochanters. Osteosynthesis is a prompt and efficient method for managing stable intertrochanteric fractures. Utilizing osteosynthesis procedures other than intramedullary fixation to address unstable intertrochanteric fractures has been linked to a relatively elevated failure rate. Hemiarthroplasty, a surgical procedure that avoids the problems of an IT fracture resulting from prolonged immobility and allows for early patient mobilization, could potentially resolve the problem. As part of this comparative analysis, we examined the surgical and functional results of PFN osteosynthesis and bipolar hemiarthroplasty in older patients with unstable intertrochanteric fractures.
Materials and Methods: This study included 44 patients, consisting of 24 males and 20 females. The participants were chosen for the study depending on whether or not they met the specified criteria for inclusion and exclusion. The individuals presented with unstable intertrochanteric fractures. The study participants were included in the research after they gave their written informed consent in both English and regional languages. A total of 22 individuals underwent cemented bipolar hemiarthroplasty, whereas the remaining 22 cases underwent PFN osteosynthesis.
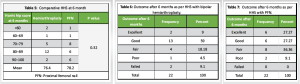
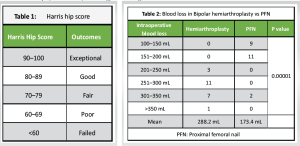
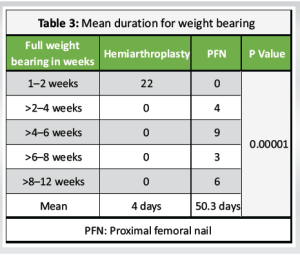
Results: In this study, a group of researchers monitored 44 patients who had unstable intertrochanteric femur fractures over 6 months. The subsequent results were generated by comparing the outcomes of the two groups after 1 month and 6 months: The mean duration of weight-bearing for patients who underwent bipolar hemiarthroplasty was 4 days, whereas, for patients who underwent PFN, it was 50 days. The mean blood loss following bipolar hemiarthroplasty is 288 ml, whereas the mean blood loss associated with PFN is approximately 174 ml. One month after undergoing bipolar hemiarthroplasty, the patient’s Harris hip score was 69 and their PFN score was 59. The bipolar score at the 6-month follow-up was 76, whereas the PFN score was 78. The average duration of bipolar hemiarthroplasty was 84.8 min, whereas PFN had a duration of 67 min. In the group of patients who underwent bipolar hemiarthroplasty, the highest amount of shortening observed was 2.5 cm, whereas in the group of patients who underwent PFN, it was 2 cm.
Conclusion: Our study showed that by performing cemented bipolar hemiarthroplasty in unstable intertrochanteric fractures, we were able to prevent the problems commonly associated with internal fixation. In addition, we could facilitate prompt mobilization in geriatric patients, allowing them to regain their pre-injury level of functioning and enhance their overall quality of life. At the 1-month mark, bipolar hemiarthroplasty yielded superior early functional results compared to PFN. However, by the 6-month mark, both groups exhibited similar scores for functional outcomes. In conclusion, primary cemented bipolar hemiarthroplasty offers a stable, pain-free, and mobile joint with an acceptable rate of complications and improved early recovery.
Keywords: Bipolar hemiarthroplasty, PFN, Harris Hip Score(HHH), Osteoporotic, Unstable Intertrochanteric Fracture, DHS
Intertrochanteric fractures are the primary cause of disability and mortality among the elderly. These fractures make up 45% of all hip fractures and are considered unstable in 35–40% of cases [1]. Older patients with hip fractures who undergo internal fixation have a notable mortality rate ranging from 15 to 20% within the initial 3–6 months. Subsequently, in the subsequent year, that figure increased to 30% [2]. Motor collisions and other types of high-speed trauma and slipping and falling within a residence have the potential to inflict severe injuries [3]. Attaining complete weight bearing in the early stages due to osteoporosis and instability is challenging [4]. Unstable comminuted intertrochanteric fractures are associated with many problems including high rates of non-union, metal failure, and femoral head perforation and challenges in attaining precise alignment [5]. Osteosynthesis using a dynamic hip screw (DHS) or proximal femoral nail (PFN) is an established method for treating stable intertrochanteric fractures [6-8]. At present, there is no established and uniform approach for treating unstable intertrochanteric fractures in the elderly [7, 8]. Prosthetic replacement will enable the patient to ambulate [9]. Multiple studies have shown that the rates of treatment failure such as varus collapse, screw cut out, shortening, and late weight bearing for unstable intertrochanteric fractures treated with older methods of osteosynthesis using DHS or PFN range from 4.5 to 16.5% [10]. The primary objectives of surgery for an unstable intertrochanteric fracture of the femur in older patients with osteoporosis are to facilitate early walking and prevent problems of failure resulting from open reduction and internal fixation [11,12]. Patients who are elderly with osteoporosis, have a comminuted intertrochanteric fracture of the femur, need to start walking early, and to have good survival in the midterm, should consider bipolar hemiarthroplasty as a suitable and successful choice [13]. The participants in this study were older individuals diagnosed with an unstable intertrochanteric fracture. The objective of the study was to assess the functional outcome of primary cemented bipolar hemiarthroplasty in such cases. We conducted a comparative analysis of the surgical and functional results of bipolar arthroplasty and PFN osteosynthesis for the treatment of unstable intertrochanteric fractures in elderly patients in a rural hospital in central India and the efficiency of the prostheses to manage the complications of internal fixation.
The study included 44 individuals with unstable intertrochanteric fractures who met the specified inclusion and exclusion criteria. The study comprised participants who provided written informed permission in both English and regional languages. A total of 22 individuals underwent cemented bipolar hemiarthroplasty, whereas the remaining 22 instances underwent PFN osteosynthesis.
Protocol
Selection of cases
All unstable intertrochanteric fractures (classified according to Evan’s classification) were selected. Segregation of the cases for internal fixation using PFN or bipolar hemiarthroplasty was done based on the willingness of the patient, we explained to the patient about both the procedures, advantages, and disadvantages including the financial scheme (Yojna) available for internal fixation using PFN and the unavailability of any scheme for hemiarthroplasty, and proceed for the respective procedure according to the will of the patient following the inclusion and exclusion criteria.
Inclusion criteria
Elderly individuals aged 60 years and older are restricted to fractures that are not stable (according to Evan’s categorization), and patients who can walk before sustaining an injury.
Exclusion criteria
Open intertrochanteric fractures, individuals suffering from pathological fractures, individuals experiencing a neurovascular injury, presence of infection, or compromised skin conditions at the surgical location. Patients with no neurological diseases.
Operative method
A posterior approach was used. The head is extracted by approaching it through the fracture window followed by sizing of the head. Prosthesis was inserted on trial, the joint was reduced, traction was given to the operative limb to maintain the limb length compared to the non-operative limb, and the level of the prosthesis to be sunk marked on the prosthesis with a marker pen. Stainless steel wire is passed around the proximal femur or sometimes through a drill hole on the femoral shaft for greater trochanteric fixation. For calcar reconstruction bone graft harvested from femoral head and neck part. After cementing is done, a calcar graft is placed, and the prosthesis is sunk to the previously marked level with the version referred from the intercondylar line. After the cement is set, the joint is reduced. Sometimes cement is used to support calcar. Greater trochanter reconstruction is done with the SS wires previously passed. Additional k wires are sometimes used. Lesser trochanter fragment if large is fixed with SS wire. Additional ethibond sutures were used to reinforce GT reconstruction.
PFN was done on the traction table with a standard lateral approach after attaining the reduction of fracture fragments.
Assessment of functional outcomes
Harris hip score (HHS) used.
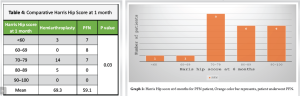
(Table 1, Fig. 1, 2, 3)
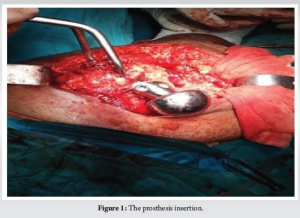
Twenty-two cases with PFN and 22 cases with bipolar hemiarthroplasty (Fig. 1-3) were monitored for 6 months, at 1 month, 3 months, and 6 months and a comparison was conducted.
Bipolar hemiarthroplasty causes approximately 288 ml of blood loss, whereas PFN causes around 174 ml (Table 1-2.)
After bipolar hemiarthroplasty, the patient began weight-bearing within the mean time of 4 days and the patients who underwent PFN started to bear weight at around the mean time of 50 days as shown in Table 3.
In the 1st month after bipolar hemiarthroplasty, the mean HHS was 69, whereas PFN was 59 as shown in Graph 1 and Table 4 . At the 6-month follow-up, the mean score was 76 for bipolar and 78 for PFN as shown in Table 5-7 and Graph 2.

Compared to the PFN, which had a duration of 67 min, the average surgical time for bipolar hemiarthroplasty was 84.8 min, which was greater than the PFN. The bipolar hemiarthroplasty group had a maximum shortening of 2.5 cm, the PFN group had a maximum shortening of 2 cm. One patient who underwent bipolar hemiarthroplasty had the incidence of a medial cortical fracture during surgery, which made up 4.5% of all cases. Two patients (9.1%) had superficial suture site infection. Within 1 month, two patients (9.1%) had dislocations which were due to a fall at home leading to the breakage of SS wires and GT fragments. Overall complication was 13.6% excluding dislocation due to falls at home. Among the patients who undergo PFNs, we encountered several issues such as screw backout in 3 cases (13.6%), reverse Z effect in 2 cases (9%), screw penetration in 1 case (4.5%), superficial infection in 1 case (4.5%), and bedsore in 1 case (4.5%). Overall 36.1% complication.
In elderly patients with osteoporosis, who are at a higher risk and mortality when they are diagnosed with the condition, intertrochanteric fractures are difficult to treat because these fractures can cause major complications with failure rates of 56% [4]. Fixation failure is associated with several hazards, one of which is that it prevents early mobilization, which in turn does not alleviate the morbidity that is associated with fractures [14]. The hemiarthroplasty technique is an alternative way that provides stability and the ability to bear one’s entire weight. In our study, the most common mode of trauma was fall at home, the same as quoted in the study by Siwach et al. [15] and Liang et al. [16]. Evan’s method was applied to divide the fracture pattern into different categories as also by Liang et al. [16], Sancheti et al. [17], Gupta et al. [18], and Bassiony et al. [19]. The greater trochanter was repaired by Bassiony et al. [19] and Kiran Kumar et al. [20] by the utilization of tension band and cerclage wiring techniques. The greater trochanter is a vital component for ensuring the hip joint remains stable, the same principle of fixation was also carried by Liang et al. [16] It is recommended that cement fixing be used to achieve rapid healing and early stability of the implant [20]. Blood lost during a PFN surgery was around 174 ml and the blood lost following a bipolar hemiarthroplasty operation was roughly 288 ml. There was a very small amount of blood that was lost throughout the course of the experiment that was carried out by Pradeep et al. [21], with the average amount being 67.4 ml and the maximum amount being 250 ml. People who had bipolar hemiarthroplasty lost more blood than those who had PFN. Based on our research, the 4th day after surgery was when most people were able to walk. The results from Sancheti et al. [17] said it took 3.2 days and were published in the journal. Puttakemparaju and Beshaj [22] did a study and found that it took 5.4 days. In a study conducted by Agrawal et al., [23] it took an average of 4.7 post-operative days for walking. We encountered several issues among patients who underwent PFNs, including screw backout in three cases (13.6%), reverse Z effect in two cases (9%), screw penetration in one case (4.5%), superficial infection in one case (4.5%), and bedsore in one case (4.5%). Overall, there were 36.1% complications. 68.2% (15) of bipolar hemiarthroplasty cases had no shortening. Only 1 case (4.5%) had a shortening of 2.7 cm which was the maximum. According to the findings of Sancheti et al., the average length reduction for 10 patients (27.02%) was 1.1 cm. As a result of the outcomes of the study that was carried out by Agrawal et al. [23], it was discovered that 16% of the patients had a reduction in length that was <2 cm and 8% had a reduction that was larger than 2 cm. In the 1st month after bipolar hemiarthroplasty, the mean HHS was 69, whereas PFN was 59. At the 6-month follow-up, the score was 76 for bipolar and 78 for PFN. In a study by Sahoo [24], the bipolar arthroplasty group had significantly higher HHS than the PFN group at 3 months, 12 months, and 24 months. Barhoum et al. did a study in which he had mean HHS at 3 months was 73.26 ± 10.5 in bipolar hemiarthroplasty and 68.48 ± 9.28 in the PFN group. There was an increase in HHS at successive follow-up periods leading to comparable outcomes with both modalities of treatment after 1 year [25]. Dr. Venkataraman found [26] that after 1 month, the mean HHS for bipolar hemiarthroplasty was 61.4 + 3.75 and for PFN it was 52.1 + 2.05. After 6 months, the average HHS for the PFN group was 79.65 + 1.5, but for the arthroplasty group, it was 79.95 + 1.82. During the first 1 month, patients who underwent PFN had significantly lower scores than those who underwent hemiarthroplasty (HHS, P = <0.001). The HHS at 6 months for both groups were similar indicating good clinical outcomes in the early post-operative period in terms of rehabilitation. Primary hemiarthroplasty can be a good alternative for therapy as it reduces post-operative complications such as pressure sores, pneumonia, stiffness, and pseudoarthrosis, it enables early mobilization, and provides excellent fixation.
Our study showed that by performing cemented bipolar hemiarthroplasty in unstable intertrochanteric fractures, we were able to prevent the problems commonly associated with internal fixation. In addition, we could facilitate prompt mobilization in geriatric patients, allowing them to regain their pre-injury level of functioning and enhance their overall quality of life. In conclusion, primary cemented bipolar hemiarthroplasty offers a stable, pain-free, and mobile joint with an acceptable rate of complications and improved early recovery.
In selected cases such as unstable intertrochanteric femur fracture, severely comminuted intertrochanteric femur fracture, and osteoporotic intertrochanteric femur fracture bipolar hemiarthroplasty is a better and valid option than internal fixation modality such as PFN as it prevents complications due to failure of internal fixation device in case of early weight-bearing. The patient can be mobilized to start full weight bearing early. However, the bipolar hemiarthroplasty procedure in unstable intertrochanteric femur fracture has a high learning curve.
It needs:
- A meticulous and stable reconstruction of the fracture greater trochanter to maintain the abductor tension
- Reconstruction of femoral calcar
- Getting the proper femoral version
- Attaining acceptable limb length with adequate sinkage of the prosthesis in the canal
- Intraoperative stability.
References
- 1.Gu GS, Wang G, Sun H, Qin DM, Zhang W. Cemented bipolar hemiarthroplasty with a novel cerclage cable technique for unstable intertrochanteric hip fractures in senile patients. Chin J Traumatol 2008;11:13-7. [Google Scholar]
- 2.Moran CG, Wenn RT, Sikand M, Taylor AM. Early mortality after hip fracture: Is delay before surgery important? J Bone Joint Surg Am 2005;87:483-9. [Google Scholar]
- 3.Mulay S, Gouri F, Mahajan U. Treatment of inter-trochantric fracture by PFN or DHS. Int J Healthc Biomed Res 2015;3:209-15. [Google Scholar]
- 4.Haidukewych GJ, Israel TA, Berry DJ. Reverse obliquity fractures of the intertrochanteric region of the femur. J Bone Joint Surg Am 2001;83:643-50. [Google Scholar]
- 5.Kang SY, Lee EW, Kang KS, Song KS, Lee SK, Park YU, et al. Mode of fixation failures of dynamic hip screw with TSP in the treatment of unstable proximal femur fracture: Biomechanical analysis and a report of 3 cases. J Korean Orthop Assoc 2006;41:176-80. [Google Scholar]
- 6.Jensen JS. Trochanteric fractures. An epidemiological, clinical and biomechanical study. Acta Orthop Scand Suppl 1981;188:1-100. [Google Scholar]
- 7.Cobelli NJ, Sadler AH. Ender Rod versus compression screw fixation of hip fractures. Clin Orthop Relat Res 1985;201:123-9. [Google Scholar]
- 8.Esser MP, Kassab JY, Jones DH. Trochanteric fractures of the femur. A randomised prospective trial comparing the Jewett nail-plate with the dynamic hip screw. J Bone Joint Surg Br 1986;68:557-60. [Google Scholar]
- 9.Harwin SF, Stern RE, Kulick RG. Primary Bateman-leinbach bipolar prosthetic replacement of the hip in the treatment of unstable intertrochanteric fractures in the elderly. Orthopedics 1990;13:1131-6. [Google Scholar]
- 10.Haidukewych GJ, Berry DJ. Hip arthroplasty for salvage of failed treatment of intertrochanteric hip fractures. J Bone Joint Surg Am 2003;85:899-904. [Google Scholar]
- 11.Sheikh IS. Intertrochantric femur fracture in elderly treated with bipolar vs dhs-a prospective study. J Med Thesis 2014;2:45-9. [Google Scholar]
- 12.Stern MB, Goldstein TB. The use of the Leinbach prosthesis in intertrochanteric fractures of the hip. Clin Orthop Relat Res 1977;128:325-31. [Google Scholar]
- 13.Patil A, Ansari M, Pathak A, Goregaonkar AB, Thakker CJ. Role of cemented bipolar hemiarthroplasty for comminuted inter-trochanteric femur fracture in elderly osteoporotic patients through a modified transtrochanteric approach-“SION hospital modification”. IOSR J Dent Med Sci 2013;9:40-7. [Google Scholar]
- 14.Sinno K, Sakr M, Girard J, Khatib H. The effectiveness of primary bipolar arthroplasty in treatment of unstable intertrochanteric fractures in elderly patients. N Am J Med Sci 2010;2:561-8. [Google Scholar]
- 15.Siwach R, Jain H, Singh R, Sangwan K. Role of hemiarthroplasty in intertrochanteric fractures in elderly osteoporotic patients: A case series. Eur J Orthop Surg Traumat 2012;22:467-72. [Google Scholar]
- 16.Liang YT, Tang PF, Guo YZ, Tao S, Zhang Q, Liang XD, et al. Clinical research of hemiprosthesis arthroplasty for the treatment of unstable intertrochanteric fractures in elderly patients. Zhonghua Yi Xue Za Zhi 2005;85:3260-2. [Google Scholar]
- 17.Sancheti KH, Sancheti PK, Shyam AK, Patil S, Dhariwal Q, Joshi R. Primary hemiarthroplasty for unstable osteoporotic intertrochanteric fractures in the elderly: A retrospective case series. Indian J Orthop 2010;44:428-34. [Google Scholar]
- 18.Gupta SK, Pathania VP, Sharma M. Primary modular bipolar hemiarthroplasty for unstable osteoporotic intertrochanteric fractures in elderly. J Evol Med Dent Sci 2014;3:3148-54. [Google Scholar]
- 19.Bassiony A, Asal MK, Mohamed HA. Cemented calcar replacement hemiarthroplasty for unstable intertrochanteric fracture femur in elderly patients. Egypt Orthop J 2013;48:190-3. [Google Scholar]
- 20.Kiran Kumar GN, Meena S, Kumar NV, Manjunath S, Vinaya Raj MK. Bipolar hemiarthroplasty in unstable intertrochanteric fractures in elderly: A prospective study. J Clin Diagn Res 2013;7:1669-71. [Google Scholar]
- 21.Pradeep C, Anuj A, Abhishek G. Treatment of comminuted unstable inter-trochanteric fracture in elderly patients with cemented bipolar prosthesis. Indian J Orthop 2015;1:255-60. [Google Scholar]
- 22.Puttakemparaju KV, Beshaj NR. Unstable intertrochanteric fracture in elderly treated with bipolar hemiarthroplasty: A prospective case series. Afr J Trauma 2014;3:81-6. [Google Scholar]
- 23.Agrawal PV, Wagh N, Pangavane S. To study the functional outcome of primary cemented bipolar hemiarthroplasty in the management of unstable inter-trochanteric fracture of femur among elderly. MVP J Med Sci 2017;4:78-83. [Google Scholar]
- 24.Sahoo PK, Dash SK, Panigrahi R, Kissan D, Das DS, Biswal MR. Cemented bipolar hemiarthroplasty versus proximal femoral nails: A prospective comparative outcome analysis in unstable elderly intertrochanteric fractures. Int J Health Sci Res 2015;5:99-106. [Google Scholar]
- 25.Almohammad A, Saad M, Barhoum S. Cemented bipolar hemiarthroplasty versus proximal femoral nail for the treatment of unstable intertrochanteric fractures in elderly: A comparative study. World J Adv Healthc Res 2023;7:153-5. [Google Scholar]
- 26.Venkataraman, Pradeep E, Kumar PM, Prajin Raj M. Comparative study of PFN A2 vs bipolar hemiarthroplasty in unstable senile intertrochanteric fractures. Int J Orthop Sci 2020;6:312-6. [Google Scholar]