Patients with COVID-19 infection are more susceptible to developing Transient Osteoporosis of the Hip (TOH). Therefore, on early suspicion of complaints of hip and thigh pain, diagnosis can be established by an early MRI scan of the hips. Patients with Transient osteoporosis of the hip can be successfully treated with bisphosphonate therapy.
Dr. Sanjay Agarwala, Department of Orthopedics and Traumatology, P D Hinduja Hospital and Medical Research Centre, Veer Savarkar Marg, Mahim (West), Mumbai - 400016, Maharashtra, India. E-mail: drsa2011@gmail.com
Introduction: Transient osteoporosis of the hip (TOH) presents with symptoms such as groin pain, discomfort, and the presence of bone edema detected on magnetic resonance imaging (MRI) scans. We have observed an increase in the occurrence of TOH in patients following the COVID-19 pandemic.
Case Report: In this series, we present four cases of TOH that developed after COVID-19 infection. The average cumulative dose of prednisolone exposure in these cases was 788 mg (range 300–1050 mg). The mean duration between diagnosis and COVID-19 infection was 102 days (range 90–123 days). The average duration from the resolution of symptoms to the initiation of bisphosphonate therapy was 98 days (range 90–120 days).
Conclusion: Bisphosphonate therapy appears to be an effective pharmacological treatment for TOH, providing rapid pain relief and shortening the disease’s natural course. This study demonstrates positive outcomes, including normalized MRI results and no progression to avascular necrosis, suggesting bisphosphonates as a promising management option for TOH patients.
Keywords: Transient osteoporosis of hip, bisphosphonates, long COVID-19.
The COVID-19 pandemic has claimed many lives, but even when the pandemic is over many are suffering from its long-term consequences. Long COVID-19 has affected every system, with musculoskeletal manifestations in the form of lethargy and muscle pain [1]. Agarwala et al. have published that patients with a history of COVID-19 infection are developing avascular necrosis (AVN) of Hips [2]. Recently one more study published a case report of transient osteoporosis of the hip (TOH) post-COVID-19 infection [3]. TOH is a rare condition caused by bone marrow edema, which is demonstrated on magnetic resonance imaging (MRI) and presents with sudden pain, or more often, mild progressive worsening pain or even asymptomatically. It is usually a benign self-limiting disease. TOH causes painful limp and joint osteopenia. Clinicoradiological appearance is identical to AVN; only MRI can accurately diagnose TOH [4]. TOH is a self-limiting illness that resolves spontaneously in 12–24 months. Bisphosphonates, calcitonin, and prostacyclin have all been used to abbreviate the natural history and resolve the disease early [5, 6, 7]. Unlike other therapies, bisphosphonates have shown promise in shortening the disease’s clinical course [5, 8]. Here, we report a series of four cases in which patients developed TOH with a history of COVID-19 infection. This is the longest series of cases of TOH as sequelae of “long COVID-19.”
We have studied the functional recovery of four cases of TOH after long COVID-19 treated with bisphosphonate combination therapy which included oral alendronate 35 mg twice a week for 6 months and a single dose of injection zolendronic acid 5 mg.
Case 1
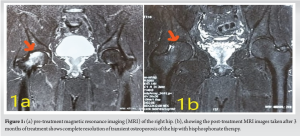
A man in his 60s complained of pain in his right hip. The patient had a COVID-19 infection 3 months prior, for which he was admitted and treated with an injection of methylprednisolone and oral dexamethasone over 19 days with a dose equivalent to 1050 mg of prednisolone. MRI scan indicated widespread bone marrow edema of the right femoral head and neck without sectoral involvement (Fig. 1a). The patient was started on bisphosphonate combination therapy. The patient was asymptomatic at 3 months, with complete radiological resolution of bone marrow edema (Fig. 1b).
Case 2
A man in his 30s was diagnosed with COVID-19 and given oral dexamethasone in tapering doses over 18 days (equivalent to 800 mg of prednisolone). One hundred and twenty-three days after the COVID diagnosis, the patient presented with right groin pain. MRI scan confirmed TOH of the right hip (Fig. 2a). The patient was started on bisphosphonate combination therapy. At 3-month follow-up, a repeat MRI confirmed the complete resolution of bone marrow edema (Fig. 2b); the patient was clinically asymptomatic and had no hip pain.
Case 3
A man in his 40s presented with left groin pain for 67 days. He had a history of COVID-19 infection, for which he was administered oral methylprednisolone 8 mg (equivalent to 300 mg prednisolone) twice a day for 15 days. (MRI scan 105 days after COVID-19) MRI scan suggested transient osteoporosis of the left hip (Fig. 3a). He was started on bisphosphonate combination therapy according to our protocol. At the 3-month follow-up, his pain score went down (from nine to four). At a 4-month follow-up, a repeat MRI showed complete resolution of bone marrow edema (Fig. 3b). The patient was clinically asymptomatic, and his pain score was zero.
Case 4
A man in his 40s presented with pain in his left groin. He was diagnosed with COVID-19 and given oral dexamethasone in tapering doses over 15 days with a total dose equal to 1000 mg of prednisolone. MRI scan confirmed TOH (90 days after COVID-19) in left hip (Fig. 4a). The patient was started on bisphosphonate combination therapy. At 6 months follow-up, a repeat MRI confirmed the complete resolution of bone marrow edema (Fig. 4b); the patient was clinically asymptomatic and had no hip .
TOH has controversial etiopathogenesis and in most cases, no direct or convincing causal events of the disease are detected. Theoretically, any insult, such as previous trauma, osteoarthritis, inflammatory and autoimmune diseases, or vascular damage (AVN, algodystrophy) could be possible causes. Cortisone, smoking, alcoholism, hypothyroidism, reduced testosterone, low Vitamin D levels, pregnancy or lactation, and other disorders have also been reported to be etiologically related, but without any convincing evidence [4]. In a recent development, Ciaffi et al. have described a case of TOH infection. They have put forward a hypothesis that bone marrow edema of the femoral neck might have avascular etiology caused by endothelial dysfunction induced by severe acute respiratory syndrome-coronavirus-2 for which they treated the patient with anticoagulant and bisphosphonate therapy and the patient had a favorable outcome [3]. Herein, we are reporting four cases of patients developing TOH with a previous history of COVID-19 infection. McCarthy found osteoclastic bone resorption in 14 of 19 TOH histological biopsy specimens. All specimens had edema, lymphocytes, and trabeculae thinning, indicating radiographic osteopenia. Histologically, it has been shown that there are two pathologies involved in TOH: Increased osteoclastic activity and bone resorption and edema. Due to their anti-inflammatory and anti-osteoclastic properties, it was speculated that bisphosphonates can reverse the pathology of TOH [9]. Medical management of TOH using bisphosphonates has been well established, giving the promising role of bisphosphonates in preventing collapse and progression of the disease to AVN [10]. Alendronate is effective in treating this debilitating condition. However, it took 4–17 weeks to resolve bone marrow edema and symptoms. Intravenous bisphosphonates like zoledronic acid, due to its increased bioavailability and faster onset of action, have been shown to shorten this duration to 2 weeks and normalize MRI changes at 3 months [5]. In this series, we report four cases of TOH developed after COVID-19 infection. With our combination bisphosphonate therapy, the disease resolved completely in all cases within 98 days (range 90–120) days. One of the primary limitations of our study lies in the relatively small number of cases analyzed. However, the study is the largest case series on this very rare complication of long COVID-19 with only another study being published has one case.
This study provides an effective pharmacotherapy option for patients with TOH. Our experience with bisphosphonate therapy reveals a shortening of the natural course of the disease, reflected in terms of pain relief as early as 2 weeks and normalization of MRI changes at 3 months. Furthermore, all the cases were observed to be performing well at their last follow-up (mean, 4–5 months), and none had progressed to AVN. We thus present an effective pharmacotherapy in the management of TOH.
Bisphosphonate therapy is an effective treatment option for TOH especially in post-COVID-19 sequelae, offering rapid symptom relief and potentially altering the disease course. It provides early pain reduction, faster radiological improvement, and may prevent progression to more serious conditions like AVN, making it a valuable pharmacological intervention for managing TOH in clinical .
References
- 1.Akbarialiabad H, Taghrir MH, Abdollahi A, Ghahramani N, Kumar M, Paydar S, et al. Long COVID, a comprehensive systematic scoping review. Infection 2021;49:1163-86. [Google Scholar]
- 2.Agarwala SR, Vijayvargiya M, Pandey P. Avascular necrosis as a part of ‘long COVID-19’. BMJ Case Rep 2021;14:e242101. [Google Scholar]
- 3.Ciaffi J, Vanni E, Facchini G, Miceli M, Ursini F. Transient osteoporosis of the hip: A novel vascular manifestation of COVID-19? Rheumatology (Oxford) 2023;62:e127-8. [Google Scholar]
- 4.Maisi N, Patoulias D, Tsagkaris C, Tsagatakis M, Goules D. Transient hip osteoporosis: Etiopathogenetic, clinical, and imaging approach. Mediterr J Rheumatol 2022;33:196-200. [Google Scholar]
- 5.Agarwala S, Vijayvargiya M. Single dose therapy of zoledronic acid for the treatment of transient osteoporosis of hip. Ann Rehabil Med 2019;43:314-20. [Google Scholar]
- 6.Arayssi TK, Tawbi HA, Usta IM, Hourani MH. Calcitonin in the treatment of transient osteoporosis of the hip. Semin Arthritis Rheum 2003;32:388-97. [Google Scholar]
- 7.Meizer R, Meraner D, Meizer E, Radda C, Landsiedl F, Aigner N. Outcome of painful bone marrow edema of the femoral head following treatment with parenteral iloprost. Indian J Orthop 2009;43:36-9. [Google Scholar]
- 8.Emad Y, Ragab Y, El-Shaarawy N, Rasker JJ. Transient osteoporosis of the hip, complete resolution after treatment with alendronate as observed by MRI description of eight cases and review of the literature. Clin Rheumatol 2012;31:1641-7. [Google Scholar]
- 9.McCarthy EF. The pathology of transient regional osteoporosis. Iowa Orthop J 1998;18:35-42. [Google Scholar]
- 10.Agarwala S, Shah S, Joshi VR. The use of alendronate in the treatment of avascular necrosis of the femoral head: Follow-up to eight years. J Bone Joint Surg Br 2009;91:1013-8. [Google Scholar]