Provided the sterilization is meticulously followed, methylene blue ink can be a cost-effective and equally safe alternative to commercially available surgical marker pens for pre-operative skin marking in joint replacement surgeries.
Dr. Niranjan Sunil Ghag, Department of Orthopedics, Dr. Shankarrao Chavan Government Medical College, Nanded, India. E-mail: ramantoshniwal34@gmail.com
Introduction: This study aimed to assess and compare the effectiveness and safety of methylene blue ink and commercially available surgical marker pens in pre-operative skin marking for joint replacement procedures. The objective was to evaluate the visibility of the surgical instruments during the operation and their influence on the occurrence of infections after the surgery, providing valuable information on the practical use and cost-effectiveness.
Materials and Methods: This retrospective randomized study involved 150 total cases, which included knee replacements, total hip replacements, and hip hemiarthroplasty performed between 2020 and 2023. The same surgeon conducted all procedures, and the patients were randomly assigned to two groups: One marked with methylene blue ink and the other with a commercially available sterile marker pen. Limb preparation followed an identical protocol for both groups. The primary outcomes assessed were the visibility of markings at the end of the procedure and the incidence of post-operative infections.
Results: The visibility of markings was satisfactory in both groups, with the methylene blue group displaying more pronounced visibility. Importantly, there were no cases of post-operative infections or permanent tattooing attributed to either marking method.
Conclusion: This study demonstrates that both methylene blue ink and commercially available surgical marker pens provide effective skin markings for surgical procedures without increasing the risk of post-operative infections or causing permanent tattooing. Methylene blue ink showed more evident marking post-procedure and ink form remains a cheaper alternative.
Keywords: Methylene blue ink, gentian violet, surgical marking pens, infection rates, joint replacement, skin marking.
Pre-operative skin marking is a critical procedure in orthopedic surgeries, particularly in joint replacement surgeries, to prevent wrong-side surgery and ensure precise incision placement [1]. Traditionally, methylene blue ink has been used due to its distinct color, making markings easily visible against the skin. However, the advent of commercially available sterile surgical marking pens has provided an alternative that is both user-friendly and sterile [2]. Methylene blue ink, a dark blue–green compound, is known for its effective staining properties and is available in 0.5% and 1% solutions which can be autoclaved or used after ethylene oxide (ETO) sterilization [3, 4]. Gentian violet is an antiseptic dye, which is available in either similar formulations which can be autoclaved/ETO, or in surgical markings which are gamma-sterilized to ensure they are free from contaminants [4, 5]. Despite the widespread use of both marking modalities, there is a lack of comprehensive studies comparing their efficacy and safety, particularly regarding post-operative infection rates and visibility during surgery. This study aims to fill this gap by retrospectively analyzing the outcomes of using methylene blue ink (autoclaved) versus commercially available surgical marker pens (gentian violet) in joint replacements.
Study design and population
This retrospective study included 150 patients undergoing joint replacements between July 2020 and January 2023 at a tertiary care center in Nanded. All surgeries were performed by the same experienced orthopedic surgeon to maintain consistency in surgical technique and outcomes. Patients were randomly assigned to two groups: One group marked with methylene blue ink (autoclaved) (Group A) and the other group marked with commercially available sterile surgical marker pens (gentian violet) (Group B) (Flowchart 1).
Pre-operative protocol
The pre-operative protocol for skin preparation was identical for both groups. It began with a thorough cleansing of the surgical site using a beta scrub solution, followed by marking the skin with the assigned marking agent. The markings included lines for incision placement and anatomical landmarks essential for the surgery.
The surgical incision was then marked with either the methylene blue ink (autoclaved) or the commercially available marker pen (gentian violet) as per the protocol. An antimicrobial incision drape was next applied over the marked site once the povidone solution had dried. All limbs were draped in an identical manner. This was a single surgeon series with operations being carried out at tertiary-level hospitals. In 75 patients commercially available marker pen was used. In the other 75 patients, methylene blue ink (autoclaved) was used. Methylene blue marking ink was prepared in the hospital pharmacy as follows – 2 g of methylene blue powder was mixed in 400 mL of demineralized water to prepare the methylene blue ink for marking. Thus, 400 mL of methylene blue marking ink was prepared at the cost of 50 rupees only which was used for 80 patients. Once the methylene blue ink was formulated, it was dispatched from the medical pharmacy in a sterile plastic container to the orthopedic operation theater store (Fig. 1). The prepared methylene blue ink was then taken in a glass bottle for autoclaving after covering the mouth with aluminum foil. This autoclaved bottle is transferred to the operation theater along with other autoclaved instruments. Once painting and draping are done the ink is applied to the skin with the help of an autoclaved sterile instrument (Blunt instrument or K-wire) (Fig. 2a). All the patients were followed up postoperatively for at least 12 months.

Outcome measures
The primary outcomes assessed were the visibility of the markings at the end of the procedure and the incidence of post-operative infections. Visibility was rated as satisfactory or unsatisfactory based on the surgeon’s ability to clearly see the markings throughout the surgery. Post-operative infections were monitored through clinical evaluations and laboratory tests, including white blood cell counts and C-reactive protein levels, during the follow-up period.
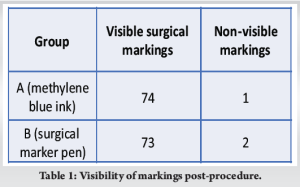
Visibility of markings
The visibility of skin markings was found to be satisfactory in both groups. In Group A (methylene blue ink), 74 out of 75 patients (98.7%) had markings that were clearly visible at the end of the surgery. Similarly, in Group B (surgical marker pen), 73 out of 75 patients (97.3%) had clearly visible markings (Table 1). The slight difference in visibility rates between the two groups was not statistically significant at P < 0.05 according to Fisher’s exact test calculator, indicating that both marking modalities are equally effective in maintaining visibility throughout the procedure (Figs. 2 and 3).
Post-operative infections
No post-operative infections were observed in either group. In Group A, none of the patients showed signs of infection during the follow-up period, which included regular clinical assessments and laboratory tests up to 1 year post-surgery. Similarly, in Group B, no infections were reported. The absence of infections in both groups suggests that neither methylene blue ink nor surgical marker pens contribute to an increased risk of post-operative infections.
Permanent tattooing
No cases of permanent tattooing were observed in either group. This was confirmed through follow-up examinations, where patients’ skin was evaluated for any residual markings. The lack of permanent tattooing further supports the safety of both marking agents.
Cost analysis
A cost analysis was conducted to compare the two marking modalities. Methylene blue ink was found to be significantly less expensive than the commercially available surgical marker pens. The cost difference, combined with the similar efficacy and safety profiles, suggests that methylene blue ink may be a more cost-effective option for pre-operative skin marking.
Pre-operative skin marking is a crucial step in ensuring the accuracy and safety of surgical procedures, particularly in joint replacements [6, 7]. This study aimed to compare the efficacy and safety of methylene blue ink versus commercially available sterile surgical marker pens in pre-operative skin marking. The results indicate that both marking agents provide satisfactory visibility and do not increase the risk of post-operative infections or permanent tattooing.
Visibility and practicality
The visibility of skin markings was found to be satisfactory in both groups, with methylene blue being more evidently visible post-procedure as well compared to commercial skin markers. This can be attributed to the distinct colors of methylene blue and gentian violet, which contrast well with the skin [3, 4, 8]. The high visibility ensures that the surgical site is accurately identified throughout the procedure, which is essential for precise incision placement and successful surgical outcomes [8].
Infection rates
The findings of the study are particularly significant regarding post-operative infection rates. Surgical site infections are a major concern in orthopedic surgeries, leading to increased health-care costs, prolonged hospital stays, and adverse patient outcomes [9]. Our study demonstrates that neither methylene blue ink nor surgical marker pens contribute to an increased risk of post-operative infections when standard pre-operative skin preparation protocols are followed. Gentian violet and methylene blue both have their own antimicrobial properties which can be the reason for these low infection rates [9, 10]. This aligns with existing literature suggesting that the sterility of the marking agent is less critical than the overall sterility of the surgical environment and skin preparation process [9]. All surgical marking preparations show more or less similar outcomes provided proper sterility is maintained in transport.
Cost-effectiveness
One of the key findings of this study is the cost-effectiveness of methylene blue ink (Rs. 1/patient) compared to commercially available surgical marker pens (Rs. 70–100/patient). Methylene blue ink is significantly less expensive, making it an attractive option for high-volume surgical settings where cost savings are essential. Given the similar efficacy and safety profiles of both, methylene blue ink preparations offer a practical and economical alternative to commercial markers without compromising patient safety or surgical outcomes [5].
Safety profile
No cases of permanent tattooing or adverse skin reactions were observed in either group, further supporting the safety of both marking modalities. This is important as permanent tattooing or skin reactions could lead to patient dissatisfaction and potential legal issues. The lack of such complications in our study suggests that both methylene blue ink and surgical marker pens are safe for use in pre-operative skin marking [3, 4, 5].
Strengths and limitations
This study has several strengths, including the use of a single experienced surgeon to ensure consistency in surgical technique and outcomes. However, there are notable limitations.
The limitations of our study were that we did not carry out any gray scale analysis but relied on the surgeon’s vision to quantify the visible marks post-adhesive drape removal in the two groups. The difference between the two groups was very evident to the naked eye; hence, we did not find the need to do so. Furthermore, we did not take any skin swabs in the follow-up period to look for organisms since there was no erythema/redness or wound discharge. None of the patients in either of the groups had clinical, local, or systemic signs of sepsis.
The retrospective nature of the study and the relatively short follow-up period may not capture all potential long-term outcomes. Furthermore, the study takes into account that all ink preparations should be properly formulated and sterilized using proper techniques, failure in any of the single steps can lead to a notable increase in infection rate.
Future directions
Future research should focus on prospective studies with larger sample sizes and longer follow-up periods to validate these findings. In addition, it would be beneficial to include multi-center studies to increase the generalizability of the results. Assessing patient satisfaction and practical aspects of each marking modality could provide further insights into their overall utility in clinical settings. Exploring the environmental impact of using disposable surgical marker pens compared to methylene blue ink may also be a valuable area of research.
This retrospective study demonstrates that methylene blue ink preparations and commercially available surgical marker pens are both effective and safe for pre-operative skin marking in joint replacement surgeries. Both modalities provide satisfactory visibility during surgery and do not increase the risk of post-operative infections or cause permanent tattooing. Given its cost-effectiveness, methylene blue ink preparations emerge as a viable and economical option for pre-operative marking provided all steps in preparation and sterilization of ink are meticulously followed. These findings support the continued use of both marking agents, contributing to safer and more efficient surgical practices.
Both commercially available surgical marker pens and methylene blue ink are equally effective and safe for marking the skin during joint replacement surgeries. These methods do not increase the risk of post-operative infections or result in permanent tattooing. Methylene blue ink is a practical and cost-efficient choice, as long as the necessary precautions for preparation and sterilization are carefully adhered to. This study provides evidence to justify the ongoing utilization of both marking agents, with no differentiating factor except for cost.
References
- 1.Canale ST. Wrong-site surgery: A preventable complication. Clin Orthop Relat Res 2005;433:26-9. [Google Scholar]
- 2.Granick MS, Heckler FR, Jones EW. Surgical skin-marking techniques. Plast Reconstr Surg 1987;79:573-80. [Google Scholar]
- 3.Cwalinski T, Polom W, Marano L, Roviello G, D’Angelo A, Cwalina N, et al. Methylene blue-current knowledge, fluorescent properties, and its future use. J Clin Med 2020;9:3538. [Google Scholar]
- 4.Prabha N, Arora RD, Ganguly S, Chhabra N. Gentian violet: Revisited. Indian J Dermatol Venereol Leprol 2020;86:600-3. [Google Scholar]
- 5.Chen TM, Castaneda M, Wanitphakdeedecha R, Nguyen TH, Tarrand JJ, Soares MK. Precautions with gentian violet: Skin marking made sterile, effective, and economical. Am J Infect Control 2009;37:244-6. [Google Scholar]
- 6.Saufl NM. Sentinel event: Wrong-site surgery. J Perianesth Nurs 2002;17:420-2. [Google Scholar]
- 7.Michaels RK, Makary MA, Dahab Y, Frassica FJ, Heitmiller E, Rowen LC, et al. Achieving the National Quality forum’s “never events”: Prevention of wrong site, wrong procedure, and wrong patient operations. Ann Surg 2007;245:526-32. [Google Scholar]
- 8.Mears SC, Davani AB, Belkoff SM. Does the type of skin marker prevent marking erasure of surgical-site markings? Eplasty 2009;9:e36. [Google Scholar]
- 9.Tenenhaus M, Bhavsar D. Do marking inks pose an infection risk? A surgeon’s perspective. Surg Infect (Larchmt) 2006;7:481-3. [Google Scholar]
- 10.Liu K, Luo Y, Hao L, Chen J. Antimicrobial effect of methylene blue in microbiologic culture to diagnose periprosthetic joint infection: An in vitro study. J Orthop Surg Res 2022;17:571. [Google Scholar]