This case report presents a novel surgical approach for addressing a proximal 1/3rd tibial shaft fracture with an ipsilateral PCL avulsion fracture, using ORIF with an LCP and advanced fixation techniques like a CC screw and spiked washer. It highlights the rarity of this injury combination and the need for tailored surgical strategies due to the lack of existing literature.
Dr. Yuvraj Vimal, Department of Orthopaedics, 5th Floor, New Surgery Building, SN Medical College, Agra, Uttar Pradesh, India 282002. E-mail: yuvrajvimal@gmail.com
Introduction: Posterior cruciate ligament (PCL) avulsion fractures of the tibia with ipsilateral tibial shaft represent a rare but challenging orthopedic injury, necessitating careful consideration of surgical interventions for optimal outcomes. This case report presents the successful management of tibial shaft fracture (proximal 1/3rd junction) along with ipsilateral PCL avulsion fracture of tibia using a novel approach using open reduction internal fixation (ORIF) of tibial shaft with Locking compression plate (LCP) with cannulated cancellous screw and spiked washer fixation of PCL avulsion. There are no case reports or research articles available for the management of PCL avulsion fracture of tibia associated with ipsilateral tibial shaft fracture.
Case Report: The patient, 34-year old male, presented with significant pain, swelling, and limited range of motion following a road traffic accident. Radiographic evaluation revealed a comminuted fracture proximal tibia and fibula with PCL avulsion fracture of the tibia, prompting a comprehensive surgical intervention. We planned to manage both fractures in a two-stage surgery. The selected approach involved ORIF of the proximal tibia fracture by utilizing LCP, followed by open reduction and internal fixation of PCL avulsion using cannulated cancellous screws, supplemented by the innovative application of a spiked washer for enhanced stability. Patients underwent monthly follow-ups during the initial 3 months. During each follow-up, both clinical and radiological assessments were conducted. Clinical evaluations focused on stability and range of motion (ROM), employing a drawer test for stability assessment. Radiological evaluations were based on the union shown in X-rays. The follow-up duration was up to 6 months, culminating in the calculation of the final functional outcome using the Lysholm knee scoring system.
Conclusion: This case report contributes valuable insights into the successful management of PCL avulsion fractures associated with ipsilateral tibial shaft fracture, emphasizing the importance of customized surgical techniques and the utilization of advanced fixation devices. The presented approach with cannulated cancellous screws and a spiked washer showcases a promising option for achieving stable fixation and promoting efficient healing in such challenging cases. Further, research and long-term studies are warranted to validate the efficacy and durability of this innovative surgical method.
Keywords: Posterior cruciate ligament avulsion, spiked washer fixation, novel technique, internal fixation.
Posterior cruciate ligament (PCL) avulsion fractures of the tibia represent a unique subset of orthopedic injuries, characterized by the detachment of the ligament from its bony insertion site. PCL injuries are less prevalent compared to anterior cruciate ligament (ACL) injuries [1]. Due to the robust nature of the PCL, avulsion fractures at its attachment sites are frequently observed [2]. PCL avulsion fractures pose a distinct challenge to orthopedic surgeons due to the intricate anatomical and biomechanical characteristics of the PCL, as well as the complex nature of tibial avulsion fractures. The PCL plays a crucial role in maintaining the stability of the knee joint by preventing posterior displacement of the tibia relative to the femur. Avulsion fractures occur when excessive force is applied to the ligament, leading to the detachment of a bony fragment from the posterior aspect of the tibia. It commonly results in an intra-substance tear; however, instances of avulsion fractures occurring at the femoral or tibial attachment sites have also been documented [3]. The clinical presentation typically includes pain, swelling, and impaired range of motion, often necessitating prompt diagnosis and intervention. Various surgical techniques have been proposed for the management of PCL avulsion fractures, ranging from conservative measures to surgical fixation. At present, there is a diverse range of materials accessible for internal fixation, such as hollow lag screws, steel wires, absorbable screws, suture anchors, and straddle nails [4,5]. The choice of intervention depends on factors such as the size and displacement of the avulsed fragment, associated injuries, and the patient’s functional demands. This case report focuses on a specific approach to the management of tibial shaft fracture (proximal 1/3rd junction) along with ipsilateral PCL avulsion fracture of tibia using a novel approach using open reduction internal fixation (ORIF) of tibial shaft with Locking compression plate (LCP) with cannulated cancellous screws and spiked washer fixation of PCL avulsion. This technique offers a novel solution to address the challenges associated with achieving stable fixation and promoting efficient healing. The introduction of this innovative method aims to contribute to the existing body of knowledge, providing clinicians with insights into a potentially promising surgical option for this complex orthopedic condition.
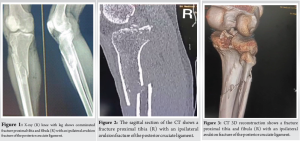
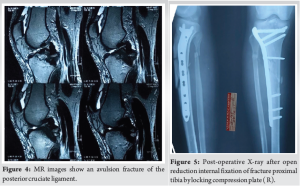
A 34-year-old male was admitted to the emergency department at S N Medical College, Agra, as a case of comminuted fracture proximal tibia and fibula (R) with ipsilateral avulsion fracture of PCL (Fig. 1-4), due to motorcycle-motorcycle collision 3 days before the admission.
Management
We planned to manage both fractures in a two-stage surgery. The selected approach involved open reduction internal fixation of fracture proximal tibia by LCP followed by open reduction and internal fixation of PCL avulsion using cannulated cancellous screws, supplemented by the innovative application of a spiked washer for enhanced stability. Post-operative X-ray after open reduction and internal fixation of the proximal tibial fracture with an LCP (R) (Fig. 5). The implant is appropriately aligned, with satisfactory reduction and fixation of the fracture fragments, ensuring stability for healing. The interval between the two surgeries was 10 days, allowing time for the skin incision to heal and the soft-tissue swelling to subside. Following the acquisition of informed consent, the patient was planned for ORIF using cannulated cancellous screws and spiked washer, employing the modified posterior approach as detailed by Burks and Schaffer [6]. The patient underwent surgery under spinal anesthesia. He was placed in a prone position on a radiolucent operating table, ensuring adequate padding for pressure points. The lower extremity was positioned with a 30° flexion at the knee joint, supported by a bolster at the ankle, and a pneumatic tourniquet was applied to the patient. An inverted “L”-shaped incision was performed, starting from the medial aspect of the gastrocnemius and curving along the joint’s flexor crease toward the lateral side (Fig. 6).
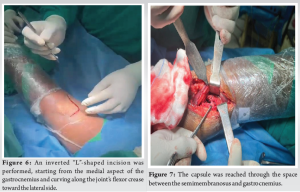
The fascia was cut following the path of the skin incision. The capsule was reached through the space between the semimembranosus and gastrocnemius (Fig. 7). A lengthwise incision was made, exposing the joint at the location of the avulsed fragment. The avulsed fragment was carefully refreshed and realigned. A slight flexion of the knee joint aided in the reduction process. Temporary fixation was achieved using a K-wire to maintain the reduction (Fig. 8 and 9).
The insertion site for the cannulated cancellous (CC) screw was located and subsequently drilled with a cannulated drill bit. Ultimately, the avulsed fragment was secured by employing a 4 mm cannulated cancellous screw along with a spiked washer, which was screwed in place over the guide wire. The K-wire used for temporary fixation was then removed (Fig. 10-12).
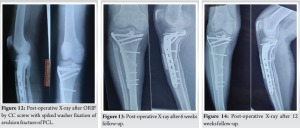
Following the closure of the incision and the application of an antiseptic dressing with appropriate padding, the limb was immobilized using an above-knee pop slab set at a 15° flexion angle for a duration of 6 weeks. The posterior support in place served to prevent any potential subluxation of the tibia [7,8]. Quadriceps strengthening exercises were introduced on the second day post-surgery. Suture removal was performed 10–12 days after the operation. Passive knee bending in the prone position commenced at the 2-week mark. Active mobilization of the knee was initiated approximately 3 weeks post-surgery. After 6 weeks of surgery, partial weight-bearing was permitted, and full weight-bearing was allowed after 12 weeks. It was also at this point that the brace was discontinued. Patients underwent monthly follow-ups during the initial 3 months. During each follow-up, both clinical and radiological assessments were conducted. Clinical evaluations focused on stability and range of motion (ROM), employing a drawer test for stability assessment. Radiological evaluations were based on the union shown in X-rays. The follow-up duration was up to 6 months, culminating in the calculation of the final functional outcome using the Lysholm knee scoring [9] system. The Lysholm knee scoring scale evaluates eight criteria: pain (0–25 points), swelling (0–10 points), limp (0–5 points), need for support using a cane or crutches (0–5 points), ability to climb stairs (0–10 points), instability (0–25 points), ability to squat (0–5 points), and locking sensation in the knee (0–15 points). Treatment outcomes are classified as “excellent” for scores above 85 points, “good” for scores between 70 and 85 points, “intermediate” for scores between 60 and 69 points, and “poor” for scores below 60 points.
At 6 weeks after surgery, the ROM was 20–60o. No instability was present in the posterior drawer test (Fig. 13).
At 12 weeks after surgery, the ROM was 10–90o. The posterior drawer test showed no instability (Fig. 14 and 15).
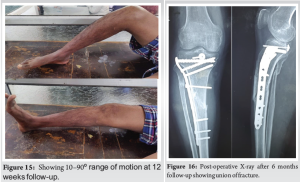
At 6 months after surgery, the ROM was 0–120o. The posterior drawer test showed no instability. Patient was able to do straight leg raise and was able to walk without support. Lysholm knee score was 95 showing excellent result (Fig. 16 and 17).

Current surgical choices for tibial avulsion fractures of the PCL include arthroscopic repair, open reduction, and internal fixation (ORIF). Arthroscopic treatment of these fractures, first reported in 1995, has gained considerable attention with advancements in arthroscopic techniques [10-13]. Despite its minimally invasive nature and the ability to address concurrent injuries such as meniscal and synovial damage, arthroscopic repair is a complex procedure with high technical demands, a prolonged learning curve, and specific equipment requirements. Furthermore, achieving reduction and fixation is often more challenging with arthroscopic methods compared to open surgery. The open posteromedial approach, introduced to avoid complications related to nerves and blood vessels, offers the potential for a clearer view of the fractured bone ends. It allows for complete fracture reduction and the effective fixation of bone fragments. In a study conducted by Sasaki et al. [14] in 2007, examining 20 knee specimens to compare the mechanical properties of tibias with PCL avulsion fractures fixed either with ORIF or arthroscopic sutures, no significant differences in tibial backward shift were observed between the two treatments. The advantages of the open posteromedial approach become evident, especially for primary-level hospitals facing challenges in accessing arthroscopic techniques. (Video 1).
There are no case reports or research articles available for the management of PCL avulsion fracture of tibia associated with ipsilateral tibial shaft fracture. This case report contributes valuable insights into the successful management of PCL avulsion fractures complicated by ipsilateral fracture of the tibial shaft, emphasizing the importance of customized surgical techniques and the utilization of advanced fixation devices. The presented approach with cannulated cancellous screws and a spiked washer for the management of PCL avulsion fractures showcases a promising option for achieving stable fixation and promoting efficient healing in such challenging cases. Further research and long-term studies are warranted to validate the efficacy and durability of this innovative surgical method.
This case report contributes valuable insights into the successful management of PCL avulsion fractures associated with ipsilateral tibial shaft fracture, emphasizing the importance of customized surgical techniques and the utilization of advanced fixation devices. The presented approach with cannulated cancellous screws and a spiked washer showcases a promising option for achieving stable fixation and promoting efficient healing in such challenging cases.
References
- 1.Allen CR, Kaplan LD, Fluhme DJ, Harner CD. Posterior cruciate ligament injuries. Curr Opin Rheumatol 2002;14:142-9. [Google Scholar | PubMed]
- 2.Sonin AH, Fitzgerald SW, Hoff FL, Friedman H, Bresler ME. MR imaging of the posterior cruciate ligament: Normal, abnormal, and associated injury patterns. Radiographics 1995;15:551-61. [Google Scholar | PubMed]
- 3.Hooper PO 3rd, Silko C, Malcolm TL, Farrow LD. Management of posterior cruciate ligament tibial avulsion injuries: A systematic review. Am J Sports Med 2018;46:734-42. [Google Scholar | PubMed]
- 4.Sun HQ, Ren YJ, Zhang YQ. Treatment of posterior cruciate ligament avulsion fracture with pressurized staples. Chi J Orthop Trauma 2011;13:1189-90. [Google Scholar | PubMed]
- 5.Fu YP, Hang CM, Fam HQ. Treatment of posterior cruciate ligament avulsion fracture using anchor system combined with cannulated screw. J Pract Orthop 2011;17:73-4. [Google Scholar | PubMed]
- 6.Burks RT, Schaffer JJ. A simplified approach to the tibial attachment of the posterior cruciate ligament. Clin Orthop Relat Res 1990;254:216-9. [Google Scholar | PubMed]
- 7.Jung YB, Tae SK, Lee YS, Jung HJ, Nam CH, Park SJ. Active non-operative treatment of acute isolated posterior cruciate ligament injury with cylinder cast immobilization. Knee Surg Sports Traumatol Arthrosc 2008;16:729-33. [Google Scholar | PubMed]
- 8.Meyers MH, McKeever FM. Fracture of the intercondylar eminence of the tibia. J Bone Joint Surg Am 1978;52:1677-84. [Google Scholar | PubMed]
- 9.Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med 1982;10:150-4. [Google Scholar | PubMed]
- 10.Zhao JZ, He YH, Wang JH. Treatment of acute posterior cruciate ligament avulsion fracture via arthroscopically assisted double posteromedial approach. Chi J Orthop 2005;25:16-20. [Google Scholar | PubMed]
- 11.Lu HX, Huangpu XQ, Zhang J. Treatment of acute posterior cruciate ligament avulsion fracture with arthroscopically assisted cannulated screw fixation. J Pract Orthop 2012;18:797-9. [Google Scholar | PubMed]
- 12.Horas U, Meissner SA, Heiss C, Schnettler R. Arthroscopic fixation of posterior cruciate ligament avulsion fractures: A new minimally invasive technique. Knee Surg Sports Traumatol Arthrosc 2010;18:781-3. [Google Scholar | PubMed]
- 13.Chen W, Tang D, Kang L, Ding Z, Sha M, Hong J. Effects of microendoscopy-assisted reduction and screw fixation through a single mini-incision on posterior cruciate ligament tibial avulsion fracture. Arch Orthop Trauma Surg 2012;132:429-35. [Google Scholar | PubMed]
- 14.Sasaki SU, Da Mota e Albuquerque RF, Amatuzzi MM, Pereira CA. Open screw fixation versus arthroscopic suture fixation of tibial posterior cruciate ligament avulsion injuries: A mechanical comparison. Arthroscopy 2007;23:1226-30. [Google Scholar | PubMed]