Mueller–Weiss syndrome is a rare condition seen in adults due to spontaneous osteonecrosis of tarsal navicular bone. Early recognition and management of the condition prevents arthritic changes and disability.
Dr Adithya N, Department of Orthopaedics, Sri Madhusudhan Sai Institute of Medical sciences and Research, Chikkaballapur, Karnataka, India. E-mail: adithyamoorthy95@gmail.com
Introduction: Mueller–Weiss syndrome is a rare condition seen in adults due to spontaneous osteonecrosis of tarsal navicular bone unlike Koehler’s disease which is quite common in paediatric population.
Case Report: We report a single case of Mueller–Weiss syndrome in an adult female. After a trail of conservative treatment, operative management was done with excision of necrotic fragment and arthrodesis of mid-foot joints augmented with tricortical iliac crest graft. Good fusion and significant reduction of pain on weight-bearing was observed after a duration of 6 weeks.
Conclusion: Mueller–Weiss syndrome is relatively rare differential for mid-foot pain in adult population. Early recognition and management of the condition prevents arthritic changes and disability.
Keywords: Mueller–Weiss syndrome, mid-foot pain, adult population, arthrodesis of mid-foot joints.
Mueller–Weiss syndrome is a rare condition seen in adults due to spontaneous osteonecrosis of tarsal navicular bone. As opposed to Koehler’s disease, a common condition seen in children due to osteochondrosis of tarsal navicular bone [1]. Disorder first described by W. Müller, ascribed the cause to be either secondary to compressive forces from adjacent bones or a congenital defect [2,3]. Most commonly seen in females and has a bilateral predilection. Delayed ossification of tarsal navicular with short first metatarsal induces abnormal compressive forces causing early dysplasia and fragmentation of lateral aspect of navicular [4]. Motion at the talonavicular joint is transmitted by uniform force distribution in radial, axial and tangential directions from talar head to body of navicular. Structural abnormalities lead to abnormal force distribution in dorsal surface of the joint [1]. Main complaint in these patients is chronic midfoot pain on weight-bearing localised to dorsomedial aspect of the tarsus. Management of this condition is nonoperatively by symptomatic treatment and non-weight bearing and surgical intervention done in patients who fail to respond to conservative line of management [5].
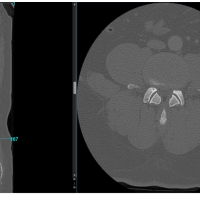
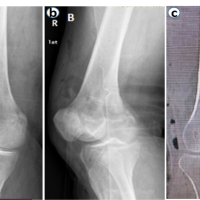
A 27-year-old female presented with complaints of pain in the right foot for 6 months. The patient had no history of significant trauma to foot or ankle. Pain was insidious in onset, non-progressive, dull aching type which aggravated on weight bearing and relieved on rest and medications. There was no associated swelling of the foot during intervals of pain. Clinical examination revealed B/L flat foot which was present from childhood, tenderness at talo-navicular joint on the dorsal surface. Mild swelling was noted over dorsolateral aspect of foot. No discolouration of skin or local rise of temperature was noted. Ankle and subtalar joint movements were within normal limits. No similar complaints were found in contralateral foot. Plain radiography of antero-posterior and oblique views (Fig. 1) of foot revealed flattening of navicular bone associated with sclerosis and cortical irregularity. Magnetic resonance imaging (Fig. 2) of foot showed reduced volume and sclerosis with marrow oedema, cortical buckling and arthritic changes at talonavicular joint. Talonavicular articulation showed inferiorly angled talar head with subchondral edema, cortical erosions, cartilage eburnation, and small geodes at anterior margin of talar head. Severe arthritic changes in talonavicular joint. Patient’s history, clinical examination findings combined with imaging suggested a provisional diagnosis of Mueller–Weiss syndrome. Laboratory results were under normal limits (complete blood counts, erythrocyte sedimentation rate, and C-reactive protein).
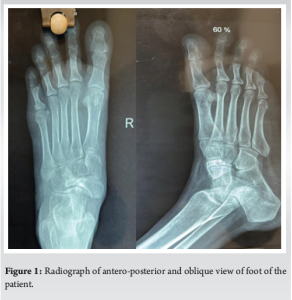

Initial treatment consisted of application of a below-knee slab with advice not bear weight on the involved limb. On persistence of pain and swelling after 4 weeks of conservative management, surgical management was planned. The removal of all sclerotic and necrotic bone with autologous bone graft and arthrodesis of talonavicular and other small tarsal joints. With patient in supine position, after spinal anaesthesia iliac crest was painted and a tricortical bone graft was harvested. From a dorsomedial approach (Fig. 3 and 4) to navicular bone was exposed, periosteum and capsule were reflected and necrotic and sclerosed bone marked under c-arm guidance and excised and sent for histopathological examination. After excising, the capsule of small tarsal joints and autologous tricortical iliac graft (Fig. 5) was filled in the void and stabilized with a cortico-cancellous screw from dorsolateral to ventromedial direction (Fig. 6). Skin closure (Fig. 7) was done in layers and a below knee slab was applied. After 6 weeks, with uptake of graft and arthrodesis of small tarsal joints was observed (Fig. 8). The patient was advised weight bearing with ankle range of motion exercises. Histopathological examination revealed bone necrosis associated with osteoporosis, no evidence of infection was noted confirming provisional diagnosis of Mueller–Weiss syndrome.





Differential diagnosis for adults with mid-foot pain include acute fracture, stress fracture, osteomyelitis, Koehler’s disease [5]. Idiopathic osteonecrosis of tarsal navicular is relatively rare compared to secondary causes of osteonecrosis of tarsal navicular namely rheumatoid arthritis, systemic lupus erythematosus, renal failure [6]. Muller–Weiss syndrome alludes to idiopathic osteonecrosis of tarsal navicular occurs due to excess mechanical strain both compressive and tensile disrupting vascular supply to the bone [6,7]. Muller and Weiss separately reported the adult-onset osteonecrosis of tarsal navicular in late 1920s [8-10]. Muller proposed precursor to be a congenital condition whereas Weiss concluded the cause to be osteonecrosis. Osteochondrosis of the tarsal navicular was also described by Koehler around the same time [1]. Koehler’s disease and Muller–Weiss syndrome are different from each other in terms of radiographic appearance, age of onset, and clinical features [1] Avascular necrosis of tarsal navicular presented with radiographic features of flattening of navicular none with increased sclerosis and cortical irregularities and magnetic resonance images showed reduced volume and sclerosis with marrow edema in tarsal navicular similar to findings of Haller et al. [6]. When left untreated the condition can progress to mid-talar arthritis and permanent disability. Our patient was managed surgically with resection of the affected segment with arthrodesis of talonaviculocuneiform joint with autologous bone graft from ipsilateral iliac crest after a trial of conservative management for 6 weeks. Mid foot joint fusion was opted due to severe arthritic changes in talonavicular joint and mild sclerotic changes in naviculocuneiform joints. Management done similar to surgical options on management of Mueller–Weiss syndrome by Monteagudo and Maceira [4] Below knee slab was applied postoperatively and was advised non-weight bearing. Postoperatively, the patient was assessed for wound healing up to 2 weeks with regular wound checks at 5 day intervals. After wound healing, radiological (fusion of joints) and clinical (pain and range of motion) parameters were assessed. Good fusion of talonaviculocuneiform joint was achieved at 6 weeks postoperatively (Fig. 8). The patient was mobilised after confirmation of joint fusion and no incidence of pain on weight bearing was noted at 6 weeks postoperatively.
In this case report, we explain the presentation, clinical signs and symptoms associated radiological changes of Mueller–Weiss syndrome and exhibit surgical management with mid-foot arthrodesis with aid of autologous bone graft from iliac crest. Significant reduction of pain noted on weight bearing after 6 weeks. Untreated cases might end up in severe mid-foot arthritis and disability.
- Incidence of Mueller–Weiss syndrome is rare in adults presenting with mid-foot pain but should always be a differential in adults presenting with mid-foot pain
- Early recognition is essential for management and prevention of arthritic changes in mid foot.
References
- 1.Reade B, Atlas G, Distazio J, Kruljac S. Mueller-weiss syndrome: An uncommon cause of midfoot pain. J Foot Ankle Surg 1998;37:535-9. [Google Scholar | PubMed]
- 2.Müller W. Über eine eigenartige doppelseitige veränderung des os naviculare beim erwachsenen. Dtsch Z Chir 1927;201:84-9. [Google Scholar | PubMed]
- 3.Müller W. Ueber eine typische gestaltsveraenderung beim os naviculare pedis und ihre klinische bedeutung. ROFO 1928;37:38-42. [Google Scholar | PubMed]
- 4.Monteagudo M, Maceira E. Management of müller-weiss disease. Foot Ankle Clin 2019;24:89-105. [Google Scholar | PubMed]
- 5.Tosun B, Al F, Tosun A. Spontaneous osteonecrosis of the tarsal navicular in an adult: Mueller-Weiss syndrome. J Foot Ankle Surg 2011;50:221-4. [Google Scholar | PubMed]
- 6.Haller J, Sartoris DJ, Resnick D, Pathria MN, Berthoty D, Howard B, et al. Spontaneous osteonecrosis of the tarsal navicular in adults: Imaging findings. Am J Roentgenol 1988;151:355-8. [Google Scholar | PubMed]
- 7.Scott-Moncrieff A, Forster BB, Andrews G, Khan K. The adult tarsal navicular: Why it matters. Can Assoc Radiol J 2007;58:279-85. [Google Scholar | PubMed]
- 8.Weiss K. Ueber die malacie des os naviculare pedis. ROFO 1929;48:63-7. [Google Scholar | PubMed]
- 9.Mueller, W. Ueber eine typische gestaltsveraenderung beim os naviculare pedis und irhe klinsche bedeutung. ROFO 37:38-42, 1928. [Google Scholar | PubMed]
- 10.Weiss, K. Ueber die malacie des os naviculare pedis. ROFO 48: 63-67, 1929 [Google Scholar | PubMed]