Accurate diagnosis of Tuberculosis versus Hodgkin’s lymphoma requires advanced imaging and multiple biopsies, as symptoms can overlap. PET CT scans and comprehensive testing are crucial for differentiating malignancies. Delays in diagnosis and treatment can worsen outcomes, highlighting the need for timely and thorough evaluation when initial treatments fail.
Dr. Vyankatesh Deshpande, Centre for Bone and Joint, Kokilaben Dhirubhai Ambani Hospital and Medical Research Institute, Mumbai, Maharashtra, India. E-mail: drvyankateshortho@gmail.com
Introduction: Tuberculosis (TB) is a leading cause of spinal infections, frequently presenting as spondylodiscitis. However, its clinical and radiological features can resemble those of Hodgkin’s Lymphoma (HL). While Gene X-pert MTB/Rif Ultra and computed tomography (CT)-guided biopsies are common diagnostic tools for TB, they may sometimes be inconclusive. In such cases, HL should be considered as a differential diagnosis. Positron emission tomography-CT (PET-CT) scans are useful in assessing whether the disease is metabolically active. Accurate and timely diagnosis is essential for effective treatment, especially when initial tests suggest an infectious cause.
Case Report: A 16-year-old male presented with lower back pain radiating to the lower limbs and difficulty walking. Magnetic resonance imaging revealed vertebral body destruction suggestive of spondylodiscitis. Despite anti-tubercular therapy, his condition worsened. Gene X-pert MTB/Rif Ultra and multiple CT-guided biopsies initially suggested a granulomatous lesion but did not confirm TB. Subsequent imaging revealed systemic nodular lesions, raising the suspicion of malignancy. Immunohistochemical studies confirmed HL with positivity for CD15 and CD30. The patient responded positively to chemotherapy and has been in remission for 1 year.
Conclusion: This case underscores the diagnostic challenges of distinguishing between spinal TB and HL. Initial tests such as Gene X-pert MTB/Rif Ultra and CT-guided biopsies can sometimes produce false negatives, leading to delays in accurate diagnosis and appropriate treatment. The use of PET-CT and detailed immune-histochemical analysis proved crucial in this case, emphasizing the importance of a comprehensive diagnostic approach when conventional treatments fail. This case contributes to the orthopedic literature by highlighting the need to consider HL in differential diagnoses and the role of advanced imaging and biopsies in ensuring timely and accurate diagnosis.
Keywords: Hodgkin’s lymphoma, spondylodiscitis, tuberculosis, gene X-pert MTB/Rif ultra, computed tomography-guided biopsy, positron emission tomography-computed tomography, differential diagnosis.
Tuberculosis (TB) is a prevalent cause of spinal infections and a leading contributor to infection-related mortality globally [1]. Skeletal TB (STB) accounts for approximately 10% of extra-pulmonary TB (EPTB), with spinal TB being the most common manifestation, representing around half of skeletal EPTB cases [2]. Spondylodiscitis, a severe form of spinal TB, can result in significant motor weakness or paralysis in about 25% of patients, and some may require surgical intervention. Delays in diagnosis or treatment can significantly worsen outcomes [3]. While the guidelines for diagnosing and treating pulmonary TB are well established, managing EPTB remains challenging [4]. Magnetic resonance imaging (MRI) is the preferred imaging technique for suspected spondylodiscitis [3]. The gold standard for confirming Mycobacterium tuberculosis (MTB) is bacterial culture, which typically requires six to eight weeks for results, limiting its practicality. Histopathological examination is crucial for diagnosis but is technically demanding in cases of skeletal TB. The Xpert MTB/Rif assay, an automated molecular test, has enhanced the detection of TB and rifampicin resistance. However, its sensitivity is limited in patients with paucibacillary disease or HIV. To address these limitations, the Gene X-pert MTB/Rif Ultra (X-pert Ultra) was developed. This assay offers improved sensitivity and specificity, particularly for multidrug-resistant TB [5]. Additional diagnostic tools include CT scans, biopsies from affected sites, PET CT scans, and blood investigations [2]. Hodgkin’s Lymphoma (HL), characterized by Reed-Sternberg cells, is a rare malignancy that can present similarly to TB, especially in cases of low back pain [6]. This similarity can lead to diagnostic confusion, particularly when initial biopsies reveal granulomatous lesions [7]. This case report highlights how multiple CT-guided biopsies and Gene X-pert MTB/Rif Ultra may sometimes lead to deceptive diagnoses, underscoring the need for careful differential diagnosis in cases of suspected infectious spondylodiscitis.
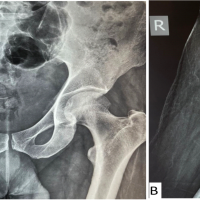
A 16-year-old boy presented to our outpatient department with lower back pain radiating to both lower limbs, accompanied by difficulty walking and prolonged sitting. His symptoms had begun six months prior and were initially treated with analgesics at his native place, but they had worsened over the past two weeks. An MRI of the lumbar spine revealed destruction of the D12 and S1 vertebral bodies with paravertebral collection (Fig. 1). Laboratory tests showed elevated white blood cell (WBC) count (15,000/µL) with 80% polymorphs, high platelet count (510,000/µL), elevated erythrocyte sedimentation rate (60 mm/h), and C-reactive protein (40 mg/L). Both the Mantoux test and Interferon Gamma Release Assay (IGRA) were negative.
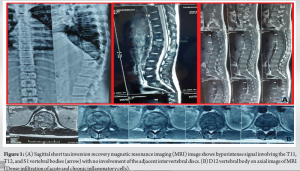
A CT-guided biopsy of the affected vertebrae was performed, and during the procedure, the radiologist noted parenchymal lung lesions. Histopathological analysis revealed dense infiltrates of acute and chronic inflammatory cells without evidence of granulomas or malignancy. An acid-fast bacilli (AFB) smear was negative, and the sample was not sent for Gene X-pert MTB/Rif Ultra. Aerobic cultures identified Pseudomonas aeruginosa, which was sensitive to all pseudomonal antibiotics. The patient initially improved with antibiotic treatment, but his condition deteriorated after 2 months, with complete blood count showing elevated WBC (18,800/µL) and 88% polymorphs. A repeat CT scan revealed nodular lesions in the lungs, spleen, and liver (Fig. 2).
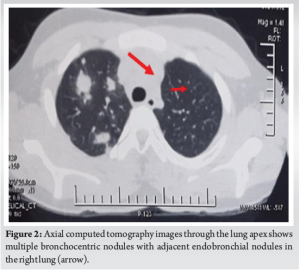
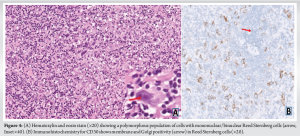
The patient was started on anti-tubercular therapy with Isoniazid, Rifampicin, Pyrazinamide, and Ethambutol. Following consultation with a pulmonologist, further investigations included bronchoscopy with bronchoalveolar lavage (BAL), endobronchial ultrasound-guided transbronchial subcarinal lymph node biopsy (EBUS-TBNA), and lung biopsies. BAL cytology was unremarkable, but Gene X-pert MTB/Rif Ultra was “positive (trace)” with “indeterminate” rifampicin resistance. Immunohistochemistry showed positivity for CD3 and CD20, suggesting a reactive lymphocyte population, and was negative for CD15 and CD30, ruling out Hodgkin’s disease. Gene X-pert MTB/Rif Ultra on lung biopsy and lymph node was negative, and Mycobacterium cultures from all specimens (BAL, lung biopsy, and lymph node biopsy) were also negative. In light of the indeterminate rifampicin result and lack of response to initial treatment, a diagnosis of drug-resistant TB was made, and a second-line regimen was initiated, including moxifloxacin, amikacin, clofazimine, linezolid, cycloserine, and para-aminosalicylic acid. Despite 2 weeks on this regimen, there was no improvement. A review of radiographic images led to suspicion of malignancy, prompting a CT-guided biopsy of left para-aortic nodes. This biopsy revealed numerous high-grade malignant cells with pleomorphic, hyperchromatic nuclei and prominent nucleoli, along with Reed-Sternberg cells. PET-CT scans showed multiple metabolically active lymph nodes and lesions in the liver, spleen, and lungs (Fig. 3).
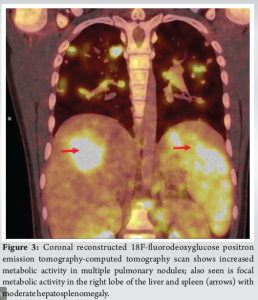
The final diagnosis was HL with a high load of Reed-Sternberg cells (Fig. 4). The patient was treated with chemotherapy using the vincristine, etoposide, prednisolone, and doxorubicin (OEPA) and cyclophosphamide, vincristine, prednisolone, and dacarbazine (COPDAC) protocol, receiving two cycles of OEPA followed by four cycles of COPDAC. A PET-CT scan after two cycles of chemotherapy showed complete resolution of FDG uptake in all lesions. The patient has remained in remission for the past year.
This case highlights the significant diagnostic challenges encountered when distinguishing between spinal TB and HL, particularly when initial tests are inconclusive. One critical area for improvement was the diagnostic testing approach. The initial CT-guided biopsy of the D12 and S1 vertebrae included histopathology, aerobic culture, and TB culture but did not utilize Gene X-pert MTB/Rif Ultra (CBNAAT). Given the low sensitivity of AFB smear tests (10%) and the moderate sensitivity of AFB culture (71%), incorporating Gene X-pert MTB/Rif Ultra, which offers higher sensitivity and specificity, could have potentially expedited the diagnosis of TB [8]. This advanced test was notably missing, which may have delayed the identification of the correct pathology. In addition, the use of IGRA and Mantoux tests, which were negative in this case, illustrates their limited utility for diagnosing TB in children in India, as current guidelines recommend against their use [9]. This situation underscores the need for more definitive and reliable diagnostic methods when faced with atypical presentations [10]. In terms of imaging, the case would have benefited significantly from an 18F-FDG PET-CT scan rather than a standard CT scan of the chest and abdomen. PET-CT scans provide both anatomical and metabolic imaging, with a 100% sensitivity for malignant tumors [11]. They are crucial for identifying metabolically active lesions and can guide the selection of biopsy sites more effectively, potentially revealing underlying malignancies sooner. The use of PET-CT could have provided more insightful data and facilitated a more accurate diagnosis. Regarding biopsy techniques, a core needle biopsy of the liver might have been more beneficial than BAL and EBUS-TBNA. Core needle biopsies often yield more definitive results, which could have been critical in this case where malignancy was a significant concern. The limitations of Gene Xpert MTB/Rif Ultra, particularly its potential to produce indeterminate results for rifampicin resistance, further complicated the diagnostic process. Such indeterminate results highlight the need for considering differential diagnoses when initial tests do not provide clear answers [12]. In cases where MTB is not detected despite comprehensive testing, it is crucial to consider other conditions, such as HL [7]. Finally, the overlap in clinical presentation and radiological findings between TB and HL can lead to diagnostic confusion. This case demonstrates how HL can mimic the appearance of spinal TB, emphasizing the importance of advanced imaging and specific diagnostic techniques. Early PET-CT imaging and thorough immunohistochemical analysis for Reed-Sternberg cells could have enabled a more accurate diagnosis sooner. This case illustrates the importance of employing a comprehensive diagnostic strategy that includes advanced imaging techniques, additional biopsy methods, and an awareness of the limitations of current diagnostic tests to ensure a timely and accurate diagnosis.
Our case report underscores the need for a thorough diagnostic approach when TB is suspected but the patient does not respond to anti-tubercular treatment. In such scenarios, if repeated investigations and CT-guided biopsies fail to yield a definitive diagnosis, performing a PET-CT scan is essential to ascertain the correct diagnosis. HL can often be misdiagnosed as TB, leading to delays in appropriate treatment and potentially worsening patient outcomes due to disease progression. Literature indicates that several cases initially diagnosed as TB were later found to be different conditions. Therefore, reliance solely on multiple CT-guided biopsies and Gene X-pert MTB/Rif Ultra can be misleading in diagnosing infectious spondylodiscitis. Comprehensive diagnostic strategies, including advanced imaging and consideration of alternative diagnoses, are crucial to avoid misdiagnosis and ensure timely and accurate treatment.
When a patient presents with symptoms suggestive of TB but does not respond to standard anti-tubercular therapy, it is crucial to consider alternative diagnoses, such as HL. Relying solely on conventional diagnostic methods such as multiple CT-guided biopsies and Gene X-pert MTB/Rif Ultra can be misleading. Incorporating advanced imaging techniques, such as PET CT scans, can provide critical insights and help differentiate between TB and malignancies. Early and accurate diagnosis is essential to prevent delays in treatment and improve patient outcomes.
References
- 1.Patel J, Upadhyay M, Kundnani V, Merchant Z, Jain S, Kire N. Diagnostic efficacy, sensitivity, and specificity of xpert MTB/RIF assay for spinal tuberculosis and rifampicin resistance. Spine (Phila Pa 1976) 2020;45:163-9. [Google Scholar | PubMed]
- 2.Rajasekaran S, Soundararajan DC, Shetty AP, Kanna RM. Spinal tuberculosis: Current concepts. Global Spine J 2018;8:96S-108. [Google Scholar | PubMed]
- 3.Kasalak Ö, Wouthuyzen-Bakker M, Adams HJ, Overbosch J, Dierckx RA, Jutte PC, et al. CT-guided biopsy in suspected spondylodiscitis: Microbiological yield, impact on antimicrobial treatment, and relationship with outcome. Skeletal Radiol 2018;47:1383-91. [Google Scholar | PubMed]
- 4.Karthek V, Bhilare P, Hadgaonkar S, Kothari A, Shyam A, Sancheti P, et al. Gene Xpert/MTB RIF assay for spinal tuberculosis- sensitivity, specificity and clinical utility. J Clin Orthop Trauma 2021;16:233-8. [Google Scholar | PubMed]
- 5.Sharma SK, Kohli M, Yadav RN, Chaubey J, Bhasin D, Sreenivas V, et al. Evaluating the diagnostic accuracy of Xpert MTB/RIF assay in pulmonary tuberculosis. PLoS One 2015;10:e0141011. [Google Scholar | PubMed]
- 6.Banerjee A, Bhuller K, Sudhir R, Bajaj A. Diagnostic dilemma of Hodgkin’s lymphoma versus tuberculosis: A case report and review of the literature. J Med Case Rep 2021;15:351. [Google Scholar | PubMed]
- 7.Djossou HJ, Ghassem MA, Toufik H, Oukabli M, Bezza A, Achemlal L. Hodgkin lymphoma mimicking lumbar spine tuberculosis. Case Rep Rheumatol 2022;2022:5298960. [Google Scholar | PubMed]
- 8.Seo YS, Kang JM, Kim DS, Ahn JG. Xpert MTB/RIF assay for diagnosis of extrapulmonary tuberculosis in children: A systematic review and meta-analysis. BMC Infect Dis 2020;20:14. [Google Scholar | PubMed]
- 9.Swaminathan S. Role of interfeoron gamma release assays in childhood tuberculosis. Indian J Pediatr 2012;79:250-2. [Google Scholar | PubMed]
- 10.Working Group on Tuberculosis, Indian Academy of Pediatrics (IAP). Consensus statement on childhood tuberculosis. Indian Pediatr 2010;47:41-5. [Google Scholar | PubMed]
- 11.Elshalakani MO, Chalabi N, Hanafy HM, Othman AI. Diagnostic value of FDG-PET/CT in fever of unknown origin. Egypt J Radiol Nucl Med 2022;53:55. [Google Scholar | PubMed]
- 12.Rigouts L, Keysers J, Rabab R, Fissette K, van Deun A, de Jong BC. GeneXpert MTB/RIF Ultra performance to detect uncommon rpoB mutations in Mycobacterium tuberculosis. BMC Res Notes 2023;16:146. [Google Scholar | PubMed]