Isolated bladder bowel symptoms can be a presentation of cauda equine syndrome; thus, clinicians should be vigilant to diagnose and provide treatment in time. Delayed surgical treatment can also lead to recovery in bladder symptoms
Dr. Kiran Dhole, Department of Orthopaedics, Government Medical College Nagpur, Maharashtra, India. E-mail: k_dhole178@yahoo.com
Introduction: Cauda equina syndrome (CES) is a constellation of symptoms that include lower limb paralysis, saddle anesthesia, bowel bladder incontinence, and sexual dysfunction. However, atypical cases of CES may present with isolated bladder-bowel involvement without motor weakness. This often leads to late patient presentation to an orthopedic surgeon and late surgical intervention. Surgical outcomes in such cases are unpredictable owing to chronic bladder incontinence. The purpose of this case series is to evaluate the effect of surgical decompression in delayed presentation of CES with isolated bladder bowel involvement.
Case Report: We attended three such patients at our institute with massive lumbar disc herniation. All of them had bladder and bowel dysfunction with the absence of lower limb weakness. Patients were operated with conventional laminectomy and discectomy. Bladder ultrasonography was done preoperatively and postoperatively. Bladder and bowel function improved in all three patients, but recovery duration was different in all three cases.
Conclusion: Atypical presentation of CES presenting to other broad specialties, especially urology, may not detect massive lumbar disc herniation in the absence of lower limb deficit. Clinicians should be highly suspicious about the isolated presentation of CES and refer to spine surgeons. Thus, surgical decompression of massive lumbar disc prolapse can be done in the initial stages of bladder-bowel dysfunction. Surgical decompression is effective in delayed presentation of CES with good long-term prognosis.
Keywords: Cauda equina syndrome, massive lumbar disc herniation, isolated bladder-bowel involvement, laminectomy and discectomy.
Cauda equine syndrome (CES) is an emergency condition that presents with the neurological and urological symptoms due to lumbar disc herniation causing cauda equina compression, which requires urgent decompression [1]. CES presents with various symptoms, but it is often accompanied by pain in the lower back and the lower extremities, motor weakness, and bladder-bowel dysfunction because of massive lumbar disc prolapse [2-4]. In patients with bladder and bowel dysfunction who do not present with intractable pain and lower extremity weakness, diagnosis of CES may be delayed, and the operative outcomes might be poor. In such a situation, surgeon can become skeptical about considering the surgical procedure as treatment. We came across three patients with massive lumbar disc herniation at lower lumbar and lumbosacral levels who presented to us with chronic isolated bladder incontinence. The purpose of this case series is to evaluate the outcome of surgical decompression in massive lumbosacral disc herniation causing CES with isolated bowel bladder involvement.
We analyzed data of three patients presented to our institute who underwent lumbar decompression surgery for a massive lumbar disc herniation causing bladder–bowel incontinence. In absence of any lower limb motor weakness. All three patients were male, with an average age of 35. The average time from presentation after onset of symptoms to surgical decompression was 41.6 days. Detailed history of presenting complaints, clinical findings, and radiographic findings were noted. Pre-surgical and post-surgical transabdominal ultrasonography (USG) guided post-void residual volume (PVRV) tests were done in all three patients. PVRV was measured within 10 min of micturition. Less than 100 mL of PVRV was considering normal [5]. All three patients had significant PVRV preoperatively. Post-operative recovery was labeled excellent when bowel bladder function recovered completely within 1 month without any altered urethral sensation. Complete recovery of bladder bowel symptoms if delayed beyond 1 month it was labelled as good, and if there is no recovery in bladder function with persistent incontinence was considered poor outcome.
Case 1
A 24-year-old male patient laborer by occupation presented to us with a history of lifting heavy object with sudden onset of severe low back pain and bilateral lower limb radiculopathy 20 days ago before presenting to our center. The patient perceived altered urethral sensation while micturition and perianal numbness from day of onset of low back pain. The patient was unable to sit stand and walk due to severe low back pain radiating to bilateral lower limb below knee level. The patient had taken local consultation of private physician for his complaints and was given analgesic for pain management. His bladder bowel complaints worsened over few days with urinary retention and constipation. USG Kidney Ureter and Bladder study with PVRV study was done at the district hospital 5 days after the onset of low back pain. It was suggestive of significant PVRV. He presented to us 20 days after the onset of symptoms. On examination, the patient had a bilateral positive straight leg raising test of 20° with bilateral hypoesthesia in L5 S1 dermatome and saddle anaesthesia. Interestingly, the patient did not have motor weakness in the lower limb. Magnetic resonance imaging (MRI) was suggestive of broad-based posterior central bilateral paracentral and foraminal disc protrusion at L5S1 level indenting the anterior thecal sac bilateral L5 exiting nerve roots compressing bilateral S1 traversing nerve roots and significant canal stenosis (Fig. 1). Sequestered disc at S1 level, causing complete canal stenosis. The patient was operated using a posterior midline approach to the lumbar spine. Complete wide L5 laminectomy and L5S1 discectomy were done with the removal of sequestered fragments (Fig. 2). Dura regained its volume after decompression. There was no dural leak intraoperatively. The patient received standard post-operative care and mobilized on the 2nd post-operative day. The patient recovered completely with normal bladder and bowel function before 1 month time. Post-surgical PVRV done at 1 month suggested a normal study with no significant abnormality.

Case 2
A 48-year-old male patient presented to our institute with complaints of urinary incontinence for 2 and 1/2 months. He gave a history of sudden onset low back pain with left lower limb radiating pain due to lifting heavy objects 2 and 1/2 months ago. The patient noticed loss of bladder and bowel control which progressed from altered urethral sensation and perianal numbness to complete urinary incontinence and bowel dysfunction. He visited our institute after persistent symptoms of perianal numbness and bladder–bowel incontinence for 2 and 1/2 months. On examination, the patient had tenderness in the lower lumbar region without any motor deficit.
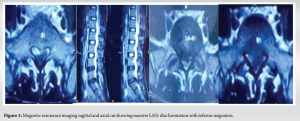
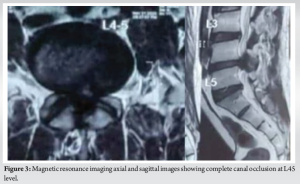
Lumbar spine X-rays were suggestive of reduced disc space at the L45 level with no signs of instability. MRI was suggestive of diffuse disc bulge at L4-5 level with ligamentum flavum hypertrophy with near complete canal occlusion (Fig. 3). We went ahead with L45 laminectomy, flavectomy, and discectomy (Fig. 4). Immediate post-operative period patient had improvement in perianal sensation but persistent urinary incontinence and anal sphincter dysfunction. The patient recovered his desire to void and anal sphincter control after 2 months after surgery but persistent perianal numbness did not recover completely. At 6-month follow-up, the patient has regained good bladder control with no significant abnormality of PVRV.

Case 3
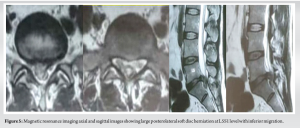
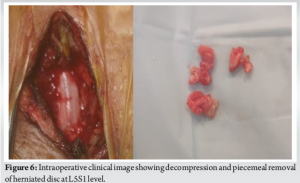
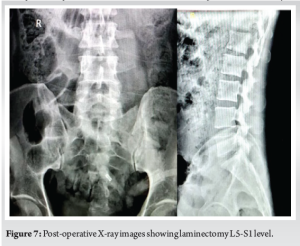
A 32-year-old male patient, laborer by occupation, had a history of sudden onset pain and tingling sensation in the right lower limb for 3 months before presenting to our hospital. The patient started to have severe low back pain along with lower limb radiculopathy, for which he took advice from the district hospital. He was managed with analgesics and neuroprotective medications. In the last 2 month before the presentation, he had an alteration in perianal sensation, which worsened to dribbling of urine and constipation. The patient had taken the opinion of a urologist for his complaints and undergone ultrasound-guided bladder USG, which was suggestive of significant PVRV. The patient presented to us with his complaint of urinary retention and constipation, for which we suspected CES. Lumbosacral X-ray showed reduced L5S1 disc space without any instability. MRI lumbosacral spine which was suggestive of large L5S1 disc herniation with posterior right paracentral extrusion and inferior migration causing severe indentation of thecal sac with compression of traversing nerve roots in right lateral recess at L5 and S1 level (Fig. 5). Patient was operated within 2 days of admission with wide laminectomy and discectomy at L5S1 (Figs. 6 and 7). After the removal of the herniated and sequestered fragment, the thecal sac was free of compression and achieved its volume. Bilateral L5 and S1 nerve roots were free at the end of decompression. The patient improved in his right lower limb radicular symptoms within few days, but urinary retention recovered only after 1 month time and residual altered urethral sensation. Bladder USG at two and a half showed normal PVRV.
CES is a rare presentation of massive lumbar and lumbosacral disc herniation, which requires urgent surgical decompression. CES is a constellation of symptoms that include low back pain, lower limb radiculopathy, saddle anesthesia, motor weakness in the lower limb, and bladder bowel dysfunction. Though classical CES is a rare entity following lower lumbar and lumbosacral disc herniation but the occurrence of subtle urinary and bowel dysfunction and saddle hypoesthesia due to lower lumbar disc herniation is significantly higher and often missed [6]. Urinary and anal sphincter dysfunction associated with CES has a wide spectrum of symptoms which includes altered urethral sensation, absence of desire to void, poor urine stream, feeling of urinary retention, micturition by straining, perianal numbness, and loss of rectal control. Gleave and McFarlane classified the severity of sphincter dysfunction into two types which include incomplete CES (CESI) and CES in retention (CESR) [7]. In CESI, there is reduced sphincter control, whereas in CESR, there is a complete loss of sphincter control. Srikandarajah et al. showed in a retrospective study that surgical intervention done within 72 h has given a good outcome in terms of bladder and sphincter control recovery IN CESI cases [8]. Early decompression is vital to prevent the progression of CESI to CESR. The early part of CES generally involves bilateral peripheral nerve dysfunction with associated sensory or motor deficit in the lower extremity. Early symptoms are followed by urinary and rectal disorders. Thus, it is very important for clinician to detect early symptoms of CES. In our case series, patients gives a history mild lower limb numbness and perianal anesthesia in the early period of symptoms without motor deficit. Delay in recognition of these early symptoms has led to worsening of bladder and bowel dysfunction to complete incontinence. In literature, cases have been described in which massive central LDH at L4/5 or L5/S1 causing CES in the absence of lower extremity weakness [9,10,11]. The bladder and external anal sphincter are innervated by somatic fibres which are originating from the sacral spinal cord. These fibers travel through the cauda equina and exit through the sacral foramen. Massive central disc herniation at the lower lumbar and lumbosacral spine impinges on only sacral roots supplying the bladder and external anal sphincter, avoiding lumbar roots. This is probably the reason of having isolated bladder and bowel symptoms. All three patients of our series initially had mild symptoms like altered urethral sensation, which were not diagnosed to be impending cauda equina compression. This led to delayed presentation of lower lumbar disc herniation with cauda equina compression, which ultimately resulted in complete urinary retention. As per recommendation in classical cauda equine syndrome with motor weakness needs to be treated with urgent surgical decompression within 48 h to get a good prognosis. However, the speed of recovery of bladder symptoms is not related to the timing of surgery. Rather, it is related with severity of sphincter disturbance and the extent of sensory loss [12]. In case series of Chang et al., recovery of bladder function after surgical decompression was slow process that took months to years together. In our case series one patient presented within a month time of urinary symptoms recovered early as compared to other two patients with a delay of 2–3 months. This suggests that long-standing symptoms can cause worsening of the severity of symptoms, thus affecting surgical outcomes. But on the other side, it shows that even in delayed presentation of bladder incontinence, surgical decompression is vital for recovery of bladder function. The surgeon and another physician should be aware that isolated bladder incontinence can be a consequence of massive lower lumbar and lumbosacral herniation and thus can be diagnosed early. Surgical decompression is must irrespective of the duration of the presentation.
Isolated bladder incontinence with saddle anesthesia is a common presentation of massive central disc herniation at the lower lumbar and lumbosacral level and is often missed. Thus, this clinical presentation should be diagnosed with a high degree of suspicion. Surgical decompression is beneficial for the recovery of bladder function.
CES can present with atypical presentation of bladder-bowel incontinence and often lead to late presentation to spine surgeons. Meticulous history taking and examination by clinicians will help for early diagnosis of this rare entity. Surgical intervention is effective for recovery of bladder symptoms even in delayed presentations.
References
- 1.Mixter WJ, Barr JS. Rupture of the intervertebral disc with involvement of the spinal canal. N Engl J Med 1934;211:210-5. [Google Scholar | PubMed]
- 2.DeLong WB, Polissar N, Neradilek B. Timing of surgery in cauda equina syndrome with urinary retention: Meta-analysis of observational studies. J Neurosurg Spine 2008;8:305-20. [Google Scholar | PubMed]
- 3.Gardner A, Gardner E, Morley T. Cauda equina syndrome: A review of the current clinical and medico-legal position. Eur Spine J 2011;20:690-7. [Google Scholar | PubMed]
- 4.Kostuik JP, Harrington I, Alexander D, Rand W, Evans D. Cauda equina syndrome and lumbar disc herniation. J Bone Joint Surg Am 1986;68:386-91. [Google Scholar | PubMed]
- 5.Asimakopoulos AD, De Nunzio C, Kocjancic E, Tubaro A, Rosier PF, Finazzi-Agrò E. Measurement of post-void residual urine. Neurourol Urodyn 2016;35:55-7. [Google Scholar | PubMed]
- 6.Bartels RH, De Vries J. Hemi-cauda equina syndrome from herniated lumbar disc: A neurosurgical emergency? Can J Neurol Sci 1996;23:296-9. [Google Scholar | PubMed]
- 7.Gleave JR, Macfarlane R. Cauda equina syndrome: What is the relationship between timing of surgery and outcome. Br J Neurosurg 2002;16:325-8. [Google Scholar | PubMed]
- 8.Nesathurai S, Jessiman TL. L4-5 disk lesion resulting in back pain with bowel, bladder and sexual dysfunction without paraparesis. Spinal Cord 1999;37:228-30. [Google Scholar | PubMed]
- 9.Chang HS, Nakagawa H, Mizuno J. Lumbar herniated disc presenting with cauda equina syndrome. Long-term follow-up of four cases. Surg Neurol 2000;53:100-5. [Google Scholar | PubMed]
- 10.Nesathurai S, Jessiman TL. L4-5 disk lesion resulting in back pain with bowel, bladder and sexual dysfunction without paraparesis. Spinal Cord 1999;37:228-30. [Google Scholar | PubMed]
- 11.Sylvester PA, McLoughlin J, Sibley GN, Dorman PJ, Kabala J, Ormerod IE. Neuropathic urinary retention in the absence of neurological signs. Postgrad Med J 1995;71:747-8. [Google Scholar | PubMed]
- 12.O’Laoire S, Crockard H, Thomas D. Prognosis for sphincter recovery after operation for cauda equina compression owing to lumbar disc prolapse. Br Med J (Clin Res Ed) 1981;282:1852-4. [Google Scholar | PubMed]