This case highlights the difficulty of deciding between limb salvage and amputation in complex trauma and states the importance of long-term functionality for patients, along with a structured approach to reconstruction.
Dr. Mikail Chatzivasiliadis, Department of Spine and Deformities, European Interbalkan Medical Center, Thessaloniki, Greece. E-mail: mikail@chatzi.com
Introduction: Complex upper extremity trauma poses us with significant challenges in orthopedic and reconstructive surgery due to the complex anatomy and functional importance of the extremities. These injuries are often the result of high-energy mechanisms like motor vehicle collisions, which makes their management particularly demanding. Making the decision between limb salvage and amputation in such cases requires careful consideration of multiple factors such as functionality, risk of complications, and recovery.
Case Report: We describe the case of a 39-year-old male who had sustained an open fracture of the elbow, avascular necrosis of the olecranon, a displaced ulna fracture, and transections of the triceps tendon and ulnar nerve. We tried to salvage the limb through planned reconstructive surgeries despite the complexity of the injuries and recommendations for amputation.
Conclusion: Managing complex upper extremity trauma requires a structured approach that balances innovative techniques with effective infection control and soft-tissue reconstruction.
Keywords: Complex upper extremity trauma, limb salvage, reconstruction, tricep tendon rupture, sural nerve graft.
Complex upper extremity trauma is a challenge in orthopedic and reconstructive surgery due to the complicated anatomy and functional role of the hand and arm. Such injuries are often the result of high-energy mechanisms which make their management very demanding. These kinds of traumas have a huge impact on the patient’s quality of life, especially for individuals in professions where they are required to use their arms or hands. The goal in these cases goes way beyond achieving structural repair; it involves the restoration of motor and sensory function to enable the patient to reintegrate into daily life and work. When considering salvaging the limb versus amputating, we need to carefully evaluate multiple important factors. Limb salvage aims to preserve functionality but often involves long treatments, higher costs, more surgeries, and the risk of complications. On the other hand, amputation offers quicker recovery and reduced risk of complications, but it leads to significant physical and emotional challenges [1,2]. We describe the case of a patient who sustained complex traumatic upper extremity injuries following a high-energy motor vehicle accident. We mention the series of reconstructive procedures and transformed what seemed like an unsalvageable injury into a successful outcome. In this case, we were faced with the critical decision to either save the limb or amputate, and we chose to attempt reconstruction to give the patient the best chance at recovery.
Clinical presentation
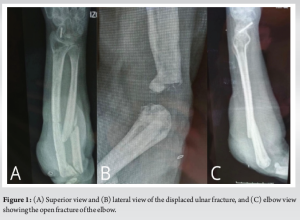
A 39-year-old male presented to the emergency department following a high-energy motor vehicle accident in which his car collided with a truck and got caught underneath it. The patient was reported to have been driving under the influence of alcohol and sustained severe trauma to his left upper extremity. Physical examination revealed a large open wound of 20 × 10 cm over the elbow with exposed bone and tremendous soft-tissue damage. The injury included an open fracture of the elbow and avascular necrosis (AVN) of the olecranon, which had no signs of infection at the time of presentation. In addition, there was a displaced fracture of the ulna along with a complete transection of the triceps tendon and cubital (ulnar) nerve. These transection injuries resulted in considerable loss of elbow extension and sensory and motor deficits. The patient’s medical history included a surgical repair of a scaphoid fracture 10 years ago, which might be unrelated to the current injury, but provided us with insight into his prior orthopedic care. The pre-operative X-rays are presented in Fig. 1.
Initial management
The patient was taken to the operating room for emergency surgical debridement to remove the necrotic tissue and reduce the risk of infection (Figs. 2 and 3). A temporary external fixator was put in to stabilize the fracture and to preserve access for further reconstructive surgeries. The severed cubital nerve was identified and placed underneath the muscle to protect it from getting damaged (Fig. 4). After surgically stabilizing this patient, he underwent two additional debridement procedures to clean the wound and prepare it for reconstruction. A chlorhexidine-based wound irrigation solution (Irrisept) was utilized in these procedures, as it has been consistently effective in preventing infections in previous patients of ours.


Given the severity of the injuries and the complex challenges that had to be faced, some physicians recommended to amputate the arm. However, by leveraging the expertise of our multidisciplinary team of surgeons, the decision was made to try and spare the limb with reconstructive surgery.
Surgical intervention
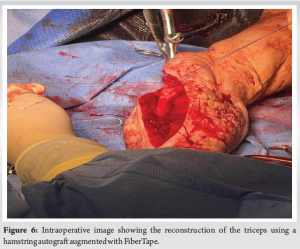
Over the course of four surgeries, rotational and advancement flaps were used to repair the lateral forearm defect. The left subcutaneous tissue was temporarily exposed to make it easier for the tissue to granulate. In addition, during this phase a vacuum-assisted closure (VAC) system was applied as well to promote wound healing and to make sure that there was adequate vascularization of the wound bed. Once enough granulation tissue had developed, a skin graft from the patient’s thigh was used to cover the forearm defect. This way we prepared the extremity for structural reconstruction. Regarding the management of the necrotic olecranon, a partial debridement of the affected olecranon was performed which left a 3 × 4 cm wound. This remaining wound was closed with rotational flaps over the course of two additional surgeries. Throughout this phase, the external fixator remained in place. Once the soft tissue had healed and the wound did not have any infections, the patient was ready to undergo reconstruction of the elbow and forearm. The displaced ulnar fracture was stabilized using a locking compression plate (LCP) and a total elbow prosthesis was implanted as the damage to the elbow joint was too severe to restore the original joint (Fig. 5). Furthermore, a hamstring autograft was made, and secured into place using FiberTape. The intraoperative reconstruction of the triceps using the hamstring autograft is presented in Fig. 6.

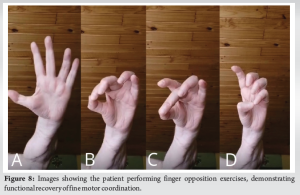
Fortunately, the patient was found to have some compensatory function which was provided by the Berrettini anastomosis of the median and ulnar nerve. However, he still wanted better function of his hand as he needed it during his duty as a police officer. To address this, a microsurgeon performed a sural nerve graft 2 months after he had his last reconstructive surgery to bridge the gap in the affected ulnar nerve.
Surgical outcome
After all these reconstructive surgeries and nerve repairs, the patient ultimately had full range of motion in all joints of the affected upper extremity, with a graded muscle strength of M2-3. It is important to mention that he had no infections during his treatment and recovery, which highlights the effectiveness of wound care and infection control measures. At last, the patient was able to successfully return to his job as a police officer. Figs. 7 and 8 display the post-operative X-rays as well as the patient’s doing the finger opposition exercise.
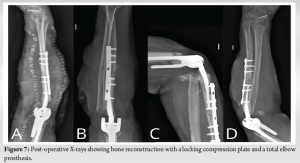
Complex trauma of the upper extremities presents us with difficult challenges due to the complicated anatomy and functional importance of the hand and arm. These injuries are often the result of high-energy mechanisms and they frequently involve the nerves, blood vessels, and soft tissues, not limited to the skeletal system. The upper extremity’s close anatomical relationship between these neurovascular structures and bones makes these injuries difficult to manage and requires a deep understanding of the interplay of the form and structure of these extremities. The successful management of these types of traumatic injuries is measured by the degree of functional restoration, which enables the patient to reintegrate into society. Following an algorithmic approach based on trauma principles we can achieve a meaningful functional outcome even in the most challenging cases [3]. There are just a few similar cases in the literature. However, no case was as complete as the one which is being described in this paper. The following case of a 39-year-old patient with an open elbow fracture is remarkably similar to our patient [4]. Both our cases involve soft-tissue loss, ulnar nerve damage, distal triceps loss, olecranon destruction, and instability of the elbow joint. In addition, the way this surgeon approached the reconstruction also resembles our case. In this case, they did a repetitive radical debridement, VAC therapy, and covered the soft-tissue defect with a fasciocutaneous flap [4]. However, there are some key differences in the surgical management that emphasize the innovative strategies of our approach. They employed a total elbow arthroplasty which they reinforced with an autologous bone graft from the proximal radius. On the other hand, in our patient’s treatment, we utilized a LCP for the displaced ulnar fracture. In addition, in our case, the triceps tendon which was damaged was reconstructed using a hamstring autograft hence restoring not only the passive extension as described by Cibula et al. but also active extension. Moreover, while this patient’s ulnar neuropathy was not resolved, our case made use of a sural nerve graft to repair the ulnar nerve. These distinctions highlight the necessity of being able to adapt in managing such complex injuries and emphasize the uniqueness of our case. By integrating innovative techniques, we are able to provide key insights to optimize outcomes for similarly devastating injuries. In another similar case report, Zeng et al. described a complex traumatic upper extremity injury where they faced the decision to either amputate or salvage the limb, like in our case. They ultimately chose to salvage the limb and in this way, we can demonstrate that both our cases are perfect examples of the potential for functional restoration of limbs through aggressive reconstructive approaches [5]. However, again in this case the injury is described in the area of the forearm up to the wrist and not the elbow. Triceps tendon ruptures are very rarely reported when discussing tendon injuries, with the majority managed through primary repair techniques [6]. Cases like ours which involve poor tissue quality need alternative strategies to ensure effective repair. The only available cases of triceps tendon ruptures with associated fractures or injuries are limited to the olecranon, which shows the rarity of our complex multi-injury case. Weistroffer et al. and Wolf et al. described the use of hamstring autografts to reconstruct triceps tendons in recurrent cases of rupture or poor tissue quality [7,8]. Weistroffer et al. used a Bunnell weaving technique with hamstring autografts, while Wolf et al. employed a crossing technique using Krackow sutures. Both approaches effectively addressed the poor triceps tendon quality [7,8]. When we compare it to our case, the surgical techniques employed in these previously mentioned cases were less complex, which is most probably due to the isolated nature of these injuries. In our patient, we used a hamstring autograft augmented with FiberTape to address the poor quality of the native triceps tendon. Schneider and Ek described a case which is the only documented literature of AVN of the olecranon, which they treated via arthroscopic assisted core decompression [9]. This minimally invasive approach successfully resolved the patient’s symptoms and gained him full elbow function. In contrast, our case involved trauma-related AVN to the olecranon, including many other injuries. To address the AVN in our patient, we surgically debrided the necrotic tissue, followed by a total elbow arthroplasty to compensate for the extensive bone loss. Unlike the atraumatic case, our approach required a multidisciplinary strategy reflecting the functional demands in our case. Even though this case was isolated and not a complex traumatic injury, it is worth mentioning as it highlights the rarity of AVN of the olecranon and serves as an important reference that helps us understand and manage this uncommon pathology. The present case shows that it is important to have a structured approach in managing complex trauma cases. The success that was achieved in this case is only made possible by great multidisciplinary efforts. Recent articles emphasize that one of the most important factors required to achieve optimal outcomes in major upper extremity trauma when deciding between limb salvage and amputation is having tight collaborations between surgeons from multiple specialties [10,11]. The present case is a key example of this principle, highlighting that a joint effort between different specialties could convert a devastating injury into a successful recovery.
This case demonstrates that when confronted with the decision to amputate or pursue limb salvage, opting to save the limb can lead to positive outcomes. Using innovative solutions, planning precisely, and a collaborative approach, we were able to restore function and allow the patient to return to his professional and personal life. The present case reflects the possibilities of modern reconstructive surgery in overcoming even the most challenging injuries.
This case demonstrates the complexities of managing severe upper extremity trauma, particularly the critical decision that sometimes needs to be made regarding limb salvage and amputation. It highlights the importance of making functionality a priority for patients and integrating a structured approach to reconstruction. This report provides important insights into innovative surgical strategies and multidisciplinary collaboration that can serve as a guide for similar challenging cases in current clinical practice.
References
- 1.Beeharry MW, Walden-Smith T, Moqeem K. Limb salvage vs. amputation: Factors influencing the decision-making process and outcomes for mangled extremity injuries. Cureus 2022;14:e30817. [Google Scholar | PubMed]
- 2.Qureshi MK, Ghaffar A, Tak S, Khaled A. Limb salvage versus amputation: A review of the current evidence. Cureus 2020;12:e10092. Erratum in: Cureus 2020;12:c38. [Google Scholar | PubMed]
- 3.Ng ZY, Askari M, Chim H. Approach to complex upper extremity injury: An algorithm. Semin Plast Surg 2015;29:5-9. [Google Scholar | PubMed]
- 4.Cibula Z, Hrubina M, Kiss J, Melisik M, Necas L. Complex open elbow fracture Gustilo-Anderson type IIIB treated with the primary elbow arthroplasty: A case report. Chin J Traumatol 2021;24:120-4. [Google Scholar | PubMed]
- 5.Zeng Q, Cai G, Liu D, Wang K, Zhang X. Successful salvage of the upper limb after crush injury requiring nine operations: A case report. Int Surg 2015;100:540-6. [Google Scholar | PubMed]
- 6.Anzel SH, Covey KW, Weiner AD, Lipscomb PR. Disruption of muscles and tendons; an analysis of 1, 014 cases. Surgery 1959;45:406-14. [Google Scholar | PubMed]
- 7.Weistroffer JK, Mills WJ, Shin AY. Recurrent rupture of the triceps tendon repaired with hamstring tendon autograft augmentation: A case report and repair technique. J Shoulder Elbow Surg 2003;12:193-6. [Google Scholar | PubMed]
- 8.Wolf JM, McCarty EC, Ritchie PD. Triceps reconstruction using hamstring graft for triceps insufficiency or recurrent rupture. Tech Hand Up Extrem Surg 2008;12:174-9. [Google Scholar | PubMed]
- 9.Schneider AK, Ek ET. Isolated avascular necrosis of the olecranon. J Shoulder Elbow Surg 2017;26:e198-202. [Google Scholar | PubMed]
- 10.Nayar SK, Alcock HMF, Edwards DS. Primary amputation versus limb salvage in upper limb major trauma: A systematic review. Eur J Orthop Surg Traumatol 2022;32:395-403. [Google Scholar | PubMed]
- 11.Xu AL, Jain D, Humbyrd CJ. The decision for amputation versus limb salvage in patients with limb-threatening lower extremity indications: An ethical analysis. Orthop Clin North Am 2025;56:67-74. [Google Scholar | PubMed]











