Acute compartment syndrome (ACS) is an emergency condition in which, should be given priority and fasciotomy must be done properly so as to ensure adequate decompression of intercompartmental pressure, this should be followed by fixation of the fractures.
Dr. Akshay Phupate, Government Medical College and Hospital, Nagpur - 440 003, Maharashtra, India. E-mail: akshayphupate2@gmail.com
Introduction: Fractures involving the supracondylar or distal end radius are the most common fracture in pediatric population. Although they have similar mechanisms of injury, i.e., hyperextension, they occur in isolation and combined supracondylar and distal end radius injuries in the same limb are extremely uncommon. We are reporting an extremely rare clinical presentation of a child with ipsilateral supracondylar fracture with fracture of distal end radius and ulna associated with acute compartment syndrome (ACS).
Case Report: A 13-year-old male had sustained trauma to left upper limb due to fall from tree. He was initially treated elsewhere with suturing of wound over his forearm and was brought to our emergency room after 12 h with complaints of swelling and severe pain in left arm, forearm, and hand. On clinical examination, there was tense swelling over the left arm, forearm, and hand. Passive stretch pain was present. Limb was warm, there were multiple blisters present over the flexor aspect over anti-cubital fossa of the left limb. On vascular and neurological evaluation, sensation was decreased compared to other limb over the volar aspect of the hand and forearm, also the pulses were feeble. The patient was immediately sent for Doppler of the left upper limb which showed biphasic flow. X-rays revealed ipsilateral left supracondylar humerus fracture (Type 4 according to Gartland Classification) with distal end radius and distal ulna fracture. As the patient had developed ACS which was evident from the tense swelling and passive stretch pain, we decided to urgently operate the patient with fasciotomy followed by fracture fixation. Wound was closed by shoelace suturing technique, and then, split-thickness skin grafting was done. K-wires were after a period of 6 weeks and gradual range of motion exercises was started.
Conclusion: Ipsilateral supracondylar with distal end radius with ACS is a rare entity. ACS should be given priority and fasciotomy must be done properly so as to ensure adequate decompression of intercompartmental pressure. This should be followed by fixation of the fractures. If appropriate intervention is done urgently, good results can be achieved even in such challenging injuries.
Keywords: Supracondylar fracture, acute compartment syndrome, fasciotomy, distal end radius, pediatrics.
Fractures involving the supracondylar or distal end radius are the most common fracture in pediatric population. Although they have similar mechanisms of injury, i.e., hyperextension, they occur in isolation and combined supracondylar and distal end radius injuries in the same limb are extremely uncommon. There have been few articles mentioning ipsilateral supracondylar and forearm fracture. The incidence varies from 2% to 13% as cited in various articles [1-4]. Acute compartment syndrome (ACS) in children is a rare but potentially devastating condition affecting orthopedic patients. ACS can result from a number of different injuries, including fractures crush injuries, vascular problems, burns, and, rarely, infection [5-10]. It may also be iatrogenic in nature, due to tight casting and bandages or extravasation of intravenous fluids [11-13]. Regardless of the specific etiology, the final common pathway of ACS is excessive pressure within non-yielding closed muscle compartments, which leads to impaired perfusion. Left untreated, myonecrosis, contracture, neurologic dysfunction, and long-term disability can result [6, 9, 12-14]. We are reporting an extremely rare clinical presentation of a child with ipsilateral supracondylar fracture with fracture of distal end radius and ulna associated with ACS. To the best of our knowledge, such kind of injury has not been previously reported in English literature.
A 13-year-old male sustained injury to left upper limb due to fall from tree. He was initially treated elsewhere with suturing of wound over his forearm and was brought to our emergency room after 12 h with complaints of swelling and severe pain in left arm, forearm, and hand. He was hemodynamically stable. On clinical examination, there was tense swelling over the left arm, forearm, and hand. Passive stretch pain was present. Tenderness was present at elbow joint and at wrist joint. There was a sutured wound present over the volar aspect on distal forearm of size 2 cm × 1 cm (Fig. 1). Limb was warm, and there were multiple blisters present over the flexor aspect over anti-cubital fossa of the left limb (Fig. 2). Deformity and abnormal mobility at fracture site were present. On vascular and neurological evaluation, sensation was decreased compared to other limbs over the volar aspect of the hand and forearm, also the pulses were feeble. The patient was immediately sent for Doppler of the left upper limb which showed biphasic flow.
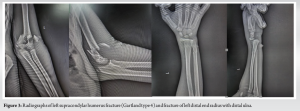
X-rays revealed ipsilateral left supracondylar humerus fracture (Type 4 according to Gartland Classification which is multidirectional instability with circumferential periosteal disruption) with distal end radius and distal ulna fracture (Fig. 3). As the patient had developed ACS which was evident from the tense swelling and passive stretch pain, we decided to urgently operate the patient with fasciotomy followed by fracture fixation.
Surgical procedure
The patient was in supine position with the left arm abducted on the side table. Under general anesthesia, wound over the volar aspect of distal forearm was debrided. Then, forearm fasciotomy was done through the midline volar incision, and superficial and deep compartments were released (Fig. 4). We could appreciate muscles popping out due to the release of intercompartmental pressure. Then, fasciotomy at the arm was done through a lateral incision at the inter-muscular septum releasing the anterior and posterior compartment (Fig. 4). Finally, fasciotomy of the hand was done through dorsal approach by longitudinal incision between second-third and fourth-fifth metacarpals (Fig. 4).
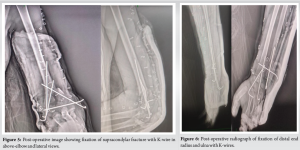
Following this, the fractures were fixed. The supracondylar fracture was tackled first and was reduced by holding the forearm in supination and giving traction and appropriate reduction maneuver. The fracture was fixed using two K-wires passed from lateral epicondyle. In view of medial commination, an additional K-wire was passed from the medial side with the elbow in extension (Fig. 5). Then, distal end radius fixation was done with two K-wires and proximal ulna was fixed with intramedullary K-wire. Furthermore, distal radioulnar junction was unstable so ulno-radial K-wire was put (Fig. 6).
We used the shoelace technique for closure of the fasciotomy wound (Fig. 7). The patient was given above elbow slab post-operative. Gradual approximation of the wound was started by tightening the shoelace and after 4 days, the wounds were covered with a split-thickness skin graft (STSG) taken from the ipsilateral thigh.
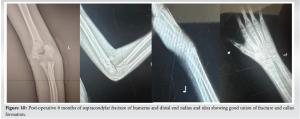
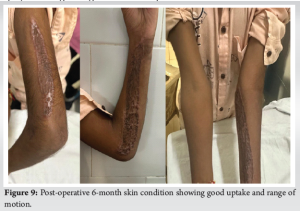
Postoperatively, the patient was much comfortable. Neurovascular examination was normal. Wounds healed well with good uptake of STSG (Fig. 8). K-wire was removed at 6 weeks once; X-ray’s showed satisfactory fracture healing. Physiotherapy was started gradually with active and passive elbow range of motion exercises. At 6-month follow-up, the patient had elbow ROM of 0–100°, full ROM at wrist, and full prono-supination (Fig. 9) and X-rays showed good union at fracture site (Fig. 10).
The combination of a supracondylar fracture of the humerus and an ipsilateral fracture of the forearm is rare but a severe injury in the growing child. The reported incidence varies between 3 and 13% [15, 16]. Palmer et al. in their analysis of 78 supracondylar fractures found four ipsilateral fractures of the radius and ulna, two ipsilateral fractures of the radius alone, and one ipsilateral midshaft ulna fracture [17]. Stanitski coined the term floating elbow for such injuries. They are considered high energy injuries with the force so much that single fracture could not dissipate all the energy of trauma [18-20]. In the true sense, floating elbow should include fracture supracondylar humerus with fracture of both bone forearm wherein the elbow is effectively dissociated from rest of the upper limb. However, various reports have included the association of single bone fracture also in floating elbow [21, 21]. The incidence of compartment syndrome is higher in these injuries [11, 22] so, the management is sometimes challenging. Blakemore et al. reported an incidence of compartment syndrome of 33% in ipsilateral displaced supracondylar humeral and forearm fractures [5]. In the largest series to date, Grottkau et al. [7] identified 131 cases of ACS in children over a period of 4 years, with 27 cases involving the upper extremity. The average age of these children was 12 years, with boys outnumbering girls in a ratio of 4:1. The study identified the most common mechanisms of injury to be forearm fractures (74%), supracondylar humerus fractures (15%), and carpal or metacarpal fractures (11%). The incidence of compartment syndrome following forearm fracture was found to be 1.04% (20/1,905), with a significantly increased risk in open fractures (relative risk = 2.2) [7]. The most common early presenting signs of compartment syndrome in adults include increasing pain, swelling, and pain with passive stretch. Later findings include paralysis, pulselessness, and neurologic symptoms. However, in children, these symptoms are often unreliable. In a study by Bae et al., pain, pallor, paresthesia, paralysis, and pulselessness were found to be inconsistent indicators of impending compartment syndrome in children [6]. The authors suggested instead that the physician should look for increasing analgesic needs as an early warning sign for potential problems. Because the early presentation of ACS can be subtle, several authors recommend the routine measurement of compartment pressures for certain patients, namely those who are uncooperative, have altered mental status, are very young, or have unreliable or inconsistent clinical symptoms [23]. Several studies have shown that the time from injury to surgery has an effect on long-term outcomes [8, 9, 24]. In a study conducted by Prasarn et al. [8], favorable outcomes were found in patients that had decompression surgery <6 h from the time of diagnosis. Finkelstein reviewed five patients that had fasciotomies more than 35 h from the time of injury [25]. Of these patients, one died of multiorgan failure and septicemia, and the remaining four required limb amputations. Hence, according to the literature, compartment release should be done within 24 h [26]. Although several techniques for closing fasciotomy wounds have been described, delayed primary closure is the procedure of choice. The shoelace technique as detailed above was first described by Cohn et al. for forearm fasciotomy closure and used rubber vessel loops as the lace component [27]. Delayed primary closure of a fasciotomy wound is often difficult because of skin edge retraction and fixation to swollen muscles. Using the shoelace technique of delayed closure of the wounds allows for gradual closure of open fasciotomy incisions, thus eliminating the need for STSG or reliance on secondary intention healing.
Ipsilateral supracondylar fractures with forearm fractures are rare, high-energy injuries requiring prompt management. ACS, must be prioritized to prevent myonecrosis and long-term complications. Early diagnosis and timely fasciotomy, followed by proper fracture fixation, are critical for achieving favorable outcomes in these challenging cases. Late fasciotomy can save limbs and children should be given a chance of fasciotomy even in late cases.
In ipsilateral supracondylar fracture with fracture distal end radius and ulna with ACS is an emergency condition in which, ACS should be given priority and fasciotomy must be done properly so as to ensure adequate decompression of intercompartmental pressure. This should be followed by fixation of the fractures. Late fasciotomy can save limbs and children should be given a chance of fasciotomy even in late cases.
References
- 1.Dhoju D, Shrestha D, Parajuli N, Dhakal G, Shrestha R. Ipsilateral supracondylar fracture and forearm bone injury in children: A retrospective review of thirty one cases. Kathmandu Univ Med J (KUMJ) 2011;9:11-6. [Google Scholar]
- 2.Siemers F, Obertacke U, Fernandez ED, Olivier LC, Neudeck F. Combination of ipsilateral supracondylar humeral-and forearm fractures in children. Zentralbl Chir 2002;127:212-7. [Google Scholar]
- 3.Tabak AY, Celebi L, Muratli HH, Yağmurlu MF, Aktekin CN, Biçimoglu A. Closed reduction and percutaneous fixation of supracondylar fracture of the humerus and ipsilateral fracture of the forearm in children. J Bone Joint Surg Br 2003;85:1169-72. [Google Scholar]
- 4.Powell RS, Bowe JA. Ipsilateral supracondylar humerus fracture and Monteggia lesion: A case report. J Orthop Trauma 2002;16:737-40. [Google Scholar]
- 5.Blakemore LC, Cooperman DR, Thompson GH, Wathey C, Ballock RT. Compartment syndrome in ipsilateral humerus and forearm fractures in children. Clin Orthop Relat Res 2000;376:32-8. [Google Scholar]
- 6.Bae DS, Kadiyala RK, Waters PM. Acute compartment syndrome in children: Contemporary diagnosis, treatment, and outcome. J Pediatr Orthop 2001;21:680-8. [Google Scholar]
- 7.Grottkau BE, Epps HR, Di Scala C. Compartment syndrome in children and adolescents. J Pediatr Surg 2005;40:678-82. [Google Scholar]
- 8.Prasarn ML, Ouellette EA, Livingstone A, Giuffrida AY. Acute pediatric upper extremity compartment syndrome in the absence of fracture. J Pediatr Orthop 2009;29:263-8. [Google Scholar]
- 9.Erdös J, Dlaska C, Szatmary P, Humenberger M, Vécsei V, Hajdu S. Acute compartment syndrome in children: A case series in 24 patients and review of the literature. Int Orthop 2011;35:569-75. [Google Scholar]
- 10.Kalyani BS, Fisher BE, Roberts CS, Giannoudis PV. Compartment syndrome of the forearm: A systematic review. J Hand Surg Am 2011;36:535-43. [Google Scholar]
- 11.Kadiyala RK, Waters PM. Upper extremity pediatric compartment syndromes. Hand Clin 1998;14:467-75. [Google Scholar]
- 12.Ramos C, Whyte CM, Harris BH. Nontraumatic compartment syndrome of the extremities in children. J Pediatr Surg 2006;41:e5-7. [Google Scholar]
- 13.Prasarn ML, Ouellette EA. Acute compartment syndrome of the upper extremity. J Am Acad Orthop Surg 2011;19:49-58. [Google Scholar]
- 14.Heckman MM, Whitesides TE Jr., Grewe SR, Judd RL, Miller M, Lawrence JH 3rd. Histologic determination of the ischemic threshold of muscle in the canine compartment syndrome model. J Orthop Trauma 1993;7:199-210. [Google Scholar]
- 15.Williamson DM, Cole WG. Treatment of ipsilateral supracondylar and forearm fractures in children. Injury 1992;23:159-61. [Google Scholar]
- 16.Flynn JC, Matthews JG, Benoit RL. Blind pinning of displaced supracondylar fractures of the humerus in children. Sixteen years’ experience with long-term follow-up. J Bone Joint Surg Am 1974;56:263-72. [Google Scholar]
- 17.Palmer EE, Niemann KM, Vesely D, Armstrong JH. Supracondylar fracture of the humerus in children. J Bone Joint Surg Am 1978;60:653-6. [Google Scholar]
- 18.Suresh S. Management of “floating elbow” in children. Indian J Orthop 2007;41:386-9. [Google Scholar]
- 19.Stanitski CL, Micheli LJ. Simultaneous ipsilateral fractures of the arm and forearm in children. Clin Orthop Relat Res 1980;153:218-22. [Google Scholar]
- 20.Ring D, Waters PM, Hotchkiss RN, Kasser JR. Pediatric floating elbow. J Pediatr Orthop 2001;21:456-9. [Google Scholar]
- 21.Harrington P, Sharif I, Fogarty EE, Dowling FE, Moore DP. Management of the floating elbow injury in children. Simultaneous ipsilateral fractures of the elbow and forearm. Arch Orthop Trauma Surg 2000;120:205-8. [Google Scholar]
- 22.Templeton PA, Graham HK. The ‘floating elbow’ in children. Simultaneous supracondylar fractures of the humerus and of the forearm in the same upper limb. J Bone Joint Surg Br 1995;77:791-6. [Google Scholar]
- 23.Matsen FA 3rd. Compartmental syndromes. Hosp Pract 1980;15:113-7. [Google Scholar]
- 24.Sheffler LC, Lattanza L, Hagar Y, Bagley A, James MA. The prevalence, rate of progression, and treatment of elbow flexion contracture in children with brachial plexus birth palsy. J Bone Joint Surg Am 2012;94:403-9. [Google Scholar]
- 25.Finkelstein JA, Hunter GA, Hu RW. Lower limb compartment syndrome: Course after delayed fasciotomy. J Trauma 1996;40:342-4. [Google Scholar]
- 26.Kanj WW, Gunderson MA, Carrigan RB, Sankar WN. Acute compartment syndrome of the upper extremity in children: Diagnosis, management, and outcomes. J Child Orthop 2013;7:225-33. [Google Scholar]
- 27.Cohn BT, Shall J, Berkowitz M. Forearm fasciotomy for acute compartment syndrome: a new technique for delayed primary closure. Orthopedics. 1986;9: 1243-1246. [Google Scholar]