To establish the functional and radiological outcome of operative management of supracondylar fracture humerus in children.2
Dr. Sanavvar Ali, Department of Orthopaedics, GSVM Medical College, Kanpur, Uttar Pradesh, India. E-mail: sanavvarali786@gmail.com
Introduction: Supracondylar fractures of the humerus are the most frequently encountered injuries around the elbow with predominantly occurring in age group 5–7 years, with a higher incidence among male. Research has indicated that for displaced humeral supracondylar fractures, both closed and open reduction with internal fixation using K-wires results in more stable outcomes.
Objectives: The purpose of this study was to determine the functional and radiological outcome of operative management of supracondylar fracture humerus in children.
Materials and Methods: It was a prospective study from 2022 to 2024. The study included 53 patients with close supracondylar fractures humerus who were surgically managed by either closed reduction and percutaneous pinning (CRPP) or open reduction and internal fixation (ORIF) by K-wire fixation, cross pinning, or lateral pinning fixation. The functional and radiological outcomes were assessed by Flynn’s criteria.
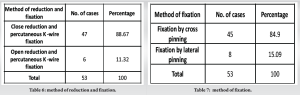
Results: Out of 53, according to Flynn criteria out of 53 patients, 14 (26.4%) of the patients had excellent outcomes, 28 (52.83%) had good outcomes, 7 (13.2%) had fair outcomes, and 4 (7.5%) had poor outcomes. Satisfactory results in 49 patients (93.33%) and unsatisfactory results in 4 (7.54%) patients.
Conclusion: CRPP is a preferred method for treating displaced supracondylar humeral fractures in children due to its minimally invasive nature, ability to maintain fracture alignment, and generally favorable outcomes with complete functional range of motion and good pain relief along with fracture union. CRPP and ORIF groups had no significant difference with respect to functional outcome. Neurovascular complications most frequently occur with Gartland type 3 and type 4 extension supracondylar fractures.
Keywords: Fracture , humerus, k-wire, pinning, supracondylar
Supracondylar fractures of the humerus are the most common fracture around elbow [1], predominantly affecting boys aged 5–7 years. These fractures often occur when a child falls on an outstretched wrist, causing the elbow to hyperextend and leading to a fracture at the supracondylar region of the humerus. Approximately 98% of these fractures are extension-type, displaced. The treatment of supracondylar humeral fractures demands careful consideration, as they often come with a range of complications more so than other fractures, including compartment syndrome, brachial artery injury, Volkmann’s ischemic contracture, elbow stiffness, nerve injury, cubitus varus, pin tract infection, and myositis ossificans [2, 3]. Conservative management with cast fixation is typically used for non-displaced (Gartland type I) fractures. However, displaced fractures require accurate anatomical reduction and internal fixation to restore elbow movement, maintain alignment, and prevent complications such as cubitus varus and nerve injuries [3-5]. Research indicates that closed or open reduction with K-wire fixation offers more stable outcomes, better alignment, and less complications in displaced fracture. Crossed pins provide better mechanical stability but increase the risk of ulnar nerve damage, while lateral entry pins reduce this risk [6-8] but may compromise stability. Outcomes of supracondylar humerus (SCH) fractures can be assessed both clinically by carrying angle and elbow range of motion (ROM) and radiologically, with Baumann’s angle being a useful radiological measure for satisfactory reduction [9, 10]. The normal range for Baumann’s angle in children is approximately 64–81°.
The modified Gartland classification for supracondylar fracture of the humerus includes:
- Type I: Non-displaced or minimally displaced fractures (<2 mm)
- Type IIA: Displaced fractures (>2 mm) with an intact posterior hinge
- Type IIB: Displaced fractures with an intact posterior hinge and malrotation
- Type III: Fully displaced fractures disrupting the posterior periosteum, with subtypes:
-
- Posterior medial displaced
- Posterior lateral displaced
- Type IV: Fully displaced fractures with multidirectional instability.
The aims and objectives of the study are to determine the functional and radiological outcome after operative management of supracondylar fracture humerus in children by assessing pain, elbow ROM, carrying angle, Baumann angle, fracture union, and complications. Primary outcome is based on Baumann angle, carrying angle, ROM at elbow, Flynn criteria and disabilities of the arm, shoulder, and hand (DASH) score. Secondary outcome fracture union, complication and compare between closed reduction and percutaneous pinning (CRPP) and Image 1.
The study was conducted on pediatric patients with supracondylar fractures of the humerus, admitted to the Department of Orthopaedics at Lala Lajpat Rai Hospital and Ganesh Shankar Vidyarthi Memorial Medical College in period of November 2022–July 2024 and was designed as a prospective study with inclusion criteria – Age: 2–16 years, both sexes, skeletally immature patients, modified Gartland’s type II, type III, and type IV fractures and exclusion criteria -Intra-articular fractures of the lower end of the humerus, flexion-type supracondylar fractures, fractures in children over 16 years of age, neuromuscular and metabolic disorders, polytrauma patients, compound fractures. The study included 53 pediatric patients who met the inclusion and exclusion criteria. Upon admission, each patient underwent a detailed examination following hemodynamic stabilization. Standard anteroposterior and lateral view X-rays were taken to classify fractures using the modified Gartland classification. Emergency management involved providing general supportive measures, examining associated injuries, and immobilizing the elbow with a long arm splint in 30–40° of flexion using a Plaster of Paris (POP) slab. The affected limb was elevated to reduce swelling, and active and passive movements of the fingers were encouraged. Ice fomentation was applied in cases of swelling, and analgesics were administered for pain control. Preoperative go thorough physical examination, focusing on assessing the neurovascular status beyond the fracture site, signs of compartment syndrome, radial pulse, and nail bed circulation. Initial management included try closed reduction and application of an above-elbow posterior POP slab with the elbow flexed at 90°, and the affected limb was elevated to minimize swelling. Patients were scheduled for surgery after written informed consent was obtained from the child’s parents or guardians. In cases of closed reduction with K-wire fixation, antibiotics were discontinued after 3 days. For open reduction procedures, intravenous antibiotics were given for 5 days, followed by oral antibiotics until suture removal. Closed reduction method included biaxial longitudinal traction, fracture site correction, and checking radial pulse. Reduction adequacy was verified with an image intensifier, and satisfactory alignment led to either plaster slab application or K-wire fixation. Open reduction was performed for unsuccessful closed reductions. Post-operative included post-surgery limb elevation, finger movement encouragement, close observation for compartment syndrome, dressing changes, X-rays, and K-wires were removed between 4 and 6-week post-surgery. Follow-up appointments assessed clinical and radiological outcomes, using Flynn criteria and modified DASH score at 12 weeks.
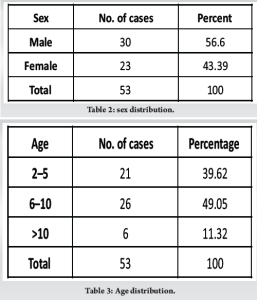
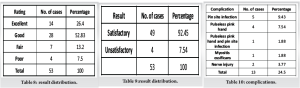
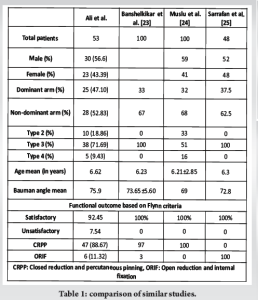
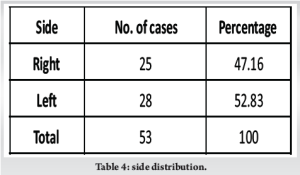
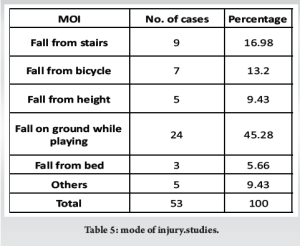
The fracture was found more common in males 30 (56.60%) patients Table 2 and Fig. 1 and in patient with age group of 5–10 years. Out of 53 patients, 23 patients belong to this age group Table 3 and Fig. 2, 17 patients in age group of 2–5 years, and 5 patients in age group of >10 years and left side (52.83%) more common than right side (47.16%) Table 4 and Fig. 3. The fracture was found more common in patients with age group of 5–10 years. The fracture was found more common in left upper limb than right. In majority of patients, SCH fracture occurs due to injury during playing or recreational activities Table 5 and Fig. 4. 47 patients (84.9%) out of 53 managed by close reduction and percutaneous K-wire fixation, in whom 40 patients (85.10%) fixed by cross pinning and 7 (14.89%) patients fixed by lateral pinning and others 6 patients (11.32%) by open reduction and percutaneous K-wire fixation Table 6 and Fig. 5. Out of 6, 5 (83.33%) patients fixed by cross pinning and 1 (16.66%) patients fixed by lateral pinning. Out of 53, 45 patients (84.9%) managed by crossed pinning fixation and others 8 patients (15.1%) by lateral pinning fixation Table 7 and Fig. 6. According to Flynn criteria out of 53 patients, 14 (26.4%) of the patients had excellent outcomes, 28 (52.83%) had good outcomes, 7 (13.2%) had fair outcomes, 4 (7.5%) had poor outcomes, satisfactory result in 49 patients (92.45%), and unsatisfactory result in 4 (7.54%) patients. Functional outcome in CRPP versus oRIF: According to Flynn criteria, patients treated with CRPP, 93.61% of patient had satisfactory result and 6.38% patients had unsatisfactory result. Patients treated with ORIF by K-wire have satisfactory result in 83.33% patients and unsatisfactory result in 16.66% patients. In functional outcome cross pinning versus lateral pinning in the cross pinning group, 93.33% patients had satisfactory result and 6.66% patients had unsatisfactory result. In the lateral pinning group, satisfactory result was 87.5% patients and unsatisfactory result in 16.66% patients Tables 8 and 9, Fig. 7and 8. There was no statistically significant difference between the two groups (cross pinning and lateral pinning) according to age, pain (Visual Analog Scale [VAS]), Baumann angle, and carrying angle and significant difference was present according to duration between injury to operative procedure and m-DASH score.
Complication
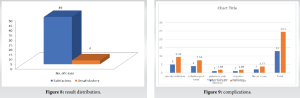
13 patients (24.5%) out of 53 had complication. One patient (1.8%) had a neurological deficit (median nerve) as a result of the fracture, one patient (1.8%) had iatrogenic ulnar nerve injury, and both were neurapraxias that resolved with conservative management for the nerve injury. Vascular compromise (pink pulseless hand) was noted in 9.43%. Total patients of neurovascular injury 12 (22.64%). Pin site infection occurs in 6 patients (11.32%). In our study, neurovascular complications most frequently occur with Gartland type III extension supracondylar fractures, 7 (13.2%) patients had neurovascular complications, 1 was Gartland type II, 4 was Gartland type III, and 2 was Gartland type IV. Myositis ossificans was seen in one patient (1.8%) Table 10 and Fig. 9.
Supracondylar humeral fractures are the most common elbow fractures in children. Historically, the primary treatment for displaced fractures was closed reduction and casting, which often led to Volkmann’s ischemic contracture. In the 1920s, Dunlop introduced traction, reducing severe complications but resulting in lengthy and costly hospital stays. Consequently, surgical intervention became more prevalent. Management of pediatric supracondylar humeral fractures includes non-operative and operative methods, tailored based on factors like fracture type (open or closed), Gartland classification, and physician preference. CRPP is the standard for displaced fractures. However, debate persists about the optimal pinning technique (lateral vs. crossed pinning). In this study of 53 patients, the mean age was 6.62 years, with a peak incidence between 5 and 10 years. This result is comparable to the series done by Patel et al. [12], where they reported a peak incidence in the 6–8-year age group with an average age of 7.48 years. There was a male predominance (56.60% males, 43.40% females) and also noted in Patel et al. [12], Wilkins [13], and Solak and Aydin table no.1 [14]. The left side was more commonly affected (52.83%) compared to the right side (47.16%). According to the Gartland classification, type III fractures were most common. The majority of injuries occurred during playing or recreational activities. For operative treatments, CRPP was the primary method for managing displaced extension type supracondylar fractures. However, there is ongoing debate about the optimal pinning technique, specifically whether lateral pinning or crossed pinning is more effective [15-17]. In a study of 53 patients with SCH fractures, 47 (88.67%) were managed by closed reduction and percutaneous K-wire fixation (CRPP), while 6 (11.32%) underwent open reduction and percutaneous K-wire fixation (ORIF). Overall, 45 (84.9%) were managed with cross pinning and 8 (15.1%) with lateral pinning. Outcomes were assessed using Flynn criteria. For CRPP, 23.4% had excellent outcomes, 57.44% good, 12.76% fair, and 6.38% poor, with 93.61% achieving satisfactory results. For ORIF, 50% had excellent outcomes, 16.66% good, 16.66% fair, and 16.66% poor, with 83.33% achieving satisfactory results. There was no statistically significant difference in age, pain (VAS), or Baumann angle between CRPP and ORIF groups, but significant differences were found in the duration between injury and operation, carrying angle, and m-DASH score. Complications occurred in 24.5% of patients, including one case each of median nerve injury and iatrogenic ulnar nerve injury (both neurapraxias resolved conservatively), vascular compromise in 9.43% of patients, pin site infections in 11.32%, and one case of myositis ossificans. Most neurovascular complications occur with Gartland type III and IV fractures[18], and most surgeons agree that a pink pulseless hand requires immediate closed reduction and stabilization. Louahem et al. [18] examined 26 patients with a pink pulseless hand out of 210 patients with severely displaced supracondylar fractures. In 21 of these cases, pulses returned right after the closed reduction of the fracture. Surgical exploration was recommended for persistent pink pulseless hands only if severe pain or deteriorating neurological function persisted [19]. For cross pinning, 28.88% had excellent outcomes, 53.33% good, 11.11% fair, and 6.66% poor, with 93.33% achieving satisfactory results. For lateral pinning, 12.5% had excellent outcomes, 50% good, 12.5% fair, and 12.5% poor, with 87.5% achieving satisfactory results. There was no statistically significant difference in age, pain (VAS), Baumann angle, or carrying angle between cross pinning and lateral pinning groups, but significant differences in duration between injury and operation and m-DASH score were noted. Cross pinning had a higher risk of iatrogenic ulnar nerve injury. Their major disadvantage of cross pinning is the iatrogenic ulnar nerve injury. The studies estimated it to occur 3–5 times more than lateral pins alone [17, 20, 21], Hamdi et al. [22]. Overall, fractures generally united in 6–12 weeks without loss of reduction. In our study radiographic outcome, mean 75.9° (range 65°–83°) Baumann’s angle, indicates satisfactory reduction in children’s SCH fractures, with a normal range of approximately 64–81°. The study concluded that CRPP for displaced SCH fractures in children produced favorable results, with a preference for cross pinning despite the higher risk of iatrogenic ulnar nerve injury. Surgical exploration was recommended for persistent pink pulseless hands only if severe pain or deteriorating neurological function persisted [19]. Image 2.
93% patients of our study had satisfactory results according to Flynn criteria, with complete functional ROM and good pain relief along with fracture union around 6–12 weeks with mean carrying angle 7.1° and mean Baumann angle 75.9°. CRPP and ORIF groups had no significant difference with respect to functional outcome. Neurovascular complications most frequently occur with Gartland type 3 and type 4 extension supracondylar fractures.
Operative management of supracondylar fracture of humerus in children has better functional and radiological outcomes.
References
- 1.Cheng JC, Ng BK, Ying SY, Lam PK. A 10-year study of the changes in the pattern and treatment of 6,493 fractures. J Pediatr Orthop 1999;19:344-50. [Google Scholar]
- 2.Leitch KK, Kay RM, Femino JD, Tolo VT, Storer SK, Skaggs DL. Treatment of multidirectionally unstable supracondylar humeral fractures in children. A modified Gartland type-IV fracture. J Bone Joint Surg Am 2006;88:980-5. [Google Scholar]
- 3.Vaquero-Picado A, González-Morán G, Moraleda L. Management of supracondylar fractures of the humerus in children. EFORT Open Rev 2018;3:526-40. [Google Scholar]
- 4.Ozan F. Type III supracondylar humerus fractures in children: Open reduction and pinning. J Clin Anal Med 2015;???:783-7. [Google Scholar]
- 5.Smajic N, Smajic J, Sadic S, Jasarevic M, Ahmetovic-Djug J, Hodzic R. Correlation between Bauman’s and carrying angle in children with supracondylar fracture of humerus. Med Arch 2013;67:195-7. [Google Scholar]
- 6.Lyons JP, Ashley E, Hoffer MM. Ulnar nerve palsies after percutaneous cross-pinning of supracondylar fractures in children’s elbows. J Pediatr Orthop 1998;18:43-5. [Google Scholar]
- 7.Blanco JS. Ulnar nerve palsies after percutaneous cross-pinning of supracondylar fractures in children’s elbows. J Pediatr Orthop 1998;18:824. [Google Scholar]
- 8.Lee SS, Mahar AT, Miesen D, Newton PO. Displaced pediatric supracondylar humerus fractures: Biomechanical analysis of percutaneous pinning techniques. J Pediatr Orthop 2002;22:440-3. [Google Scholar]
- 9.James D, Gajendran M, Paraseth T. Functional and radiological correlation in surgically managed severe supracondylar humerus fracture in a pediatric cohort using pediatric outcomes data collection instrument upper extremity scale: A report from a level V trauma center in rural Central India. CHRISMED J Health Res 2017;4:43-8. [Google Scholar]
- 10.Brubacher JW, Dodds SD. Pediatric supracondylar fractures of the distal humerus. Curr Rev Musculoskelet Med 2008;1:190-6. [Google Scholar]
- 11.Rockwood CA Jr., Wilkins KE, King RE. Fractures in Children. 3rd ed., Vol. 3. Philadelphia, PA: JB Lippincott; 1991. p. 526-617. [Google Scholar]
- 12.Patel N, Patil P, Gaonkar K, Kulkarni H, Gupta K. A comparative study of outcomes of percutaneous crossed versus lateral divergent pinning in the treatment of displaced (grade-3) supracondylar fractures of humerus in children. J Evid Based Med Healthc 2015;2:789-98. [Google Scholar]
- 13.Wilkins KE. The operative management of supracondylar fractures. Orthop Clin North Am 1990;21:269-89. [Google Scholar]
- 14.Solak S, Aydin E. Comparison of two percutaneous pinning methods for the treatment of the pediatric type III supracondylar humerus fractures. J Pediatr Orthop B 2003;12:346-9. [Google Scholar]
- 15.Vuillermin C, May C, Kasser J. Closed reduction and percutaneous pinning of pediatric supracondylar humeral fractures. JBJS Essent Surg Tech 2018;8:e10. [Google Scholar]
- 16.Isa AD, Furey A, Stone C. Functional outcome of supracondylar elbow fractures in children: A 3- to 5-year follow-up. Can J Surg 2014;57:241-6. [Google Scholar]
- 17.Prashant K, Lakhotia D, Bhattacharyya TD, Mahanta AK, Ravoof A. A comparative study of two percutaneous pinning techniques (lateral versus medial-lateral) for Gartland type III pediatric supracondylar fracture of the humerus. J Orthop Traumatol 2016;17:223-9. [Google Scholar]
- 18.Louahem DM, Nebunescu A, Canavese F, Dimeglio A. Neurovascular complications and severe displacement in supracondylar humerus fractures in children: Defensive or offensive strategy? J Pediatr Orthop B 2006;15:51-7. [Google Scholar]
- 19.Mangat KS, Martin AG, Bache CE. The “pulseless pink” hand after supracondylar fracture of the humerus in children: The predictive value of nerve palsy. J Bone Joint Surg Br 2009;91:1521-5. [Google Scholar]
- 20.Kocher MS, Kasser JR, Waters PM, Bae D, Snyder BD, Hresko MT, et al. Lateral entry compared with medial and lateral entry pin fixation for completely displaced supracondylar humeral fractures in children. A randomized clinical trial. J Bone Joint Surg Am 2007;89:706-12. [Google Scholar]
- 21.Dekker AE, Krijnen P, Schipper IB. Results of crossed versus lateral entry K-wire fixation of displaced pediatric supracondylar humeral fractures: A systematic review and meta-analysis. Injury 2016;47:2391-8. [Google Scholar]
- 22.Hamdi A, Poitras P, Louati H, Dagenais S, Masquijo JJ, Kontio K. Biomechanical analysis of lateral pin placements for pediatric supracondylar humerus fractures. J Pediatr Orthop 2010;30:135-9. [Google Scholar]
- 23.Banshelkikar S, Sheth B, Banerjee S, Maaz M. Functional outcome of supracondylar humerus fracture in children with the use of pin configuration as per Bahk classification. J Clin Orthop Trauma 2021;13:78-81. [Google Scholar]
- 24.Muslu O, Cengiz T, Aydın Şimşek Ş, Yurtbay A, Keskin D. Radiological and clinical outcomes of pediatric patients with a supracondylar humerus fracture surgically treated with closed reduction and percutaneous pinning. Cureus 2023;15:e49358. [Google Scholar]
- 25.Sarrafan N, Nasab SA, Ghalami T. Treatment of displaced supracondylar fracture of the humerus in children by open pining from lateral approach: An investigation of clinical and radiographical results. Pak J Med Sci 2015;31:930-5. [Google Scholar]