Arthroscopic TTC nailing combines minimally invasive precision with the stability of intramedullary fixation, offering excellent outcomes in ankle and hindfoot fusion.
Dr. Satyam Jawa, Department of Orthopaedics, Dr. D.Y. Patil Medical College and Hospital, Pune, Maharashtra, India. E-mail: satyamjawa@gmail.com
Introduction: Arthroscopic tibiotalocalcaneal (TTC) arthrodesis with intramedullary nail fixation is a minimally invasive technique for managing complex hindfoot pathologies, especially in patients with soft tissue injuries or poor skin conditions after trauma.
Case Report: We present the case of a 44-year-old male farmer with post-traumatic instability over his left ankle and soft tissue injury over the lateral aspect of his left lower limb secondary to a degloving injury involving a runover by a tractor. The patient had previously undergone debridement with an anterolateral thigh flap for wound coverage 3 months ago. Examination revealed severe mediolateral instability, complete distal one-third fibular loss with severe functional impairment. An arthroscopically assisted TTC fusion using a retrograde intramedullary nail was performed. The technique allowed precise joint preparation, strong internal fixation, and minimized soft tissue disruption. Post-operatively, the patient achieved a stable, plantigrade, and pain-free foot with early mobilization and improved functional outcomes, as evidenced by a high American Orthopaedic Foot and Ankle Society score and Foot and Ankle Disability Index score.
Conclusion: his case demonstrates that arthroscopic TTC nailing can be a safe and effective solution in complex clinical scenarios, offering advantages, such as reduced risk of post-operative infections, earlier rehabilitation, quicker wound healing, and satisfactory limb alignment. Despite promising results, further research and long-term studies are needed to validate this technique across broader patient populations and establish standardized surgical protocols.
Keywords: Ankle instability, tibio-talo-calcaneal fusion, subtalar arthritis, ankle arthroscopy, ankle arthrodesis.
Arthroscopic tibiotalocalcaneal (TTC) nailing is a promising treatment modality for addressing complex hindfoot and ankle pathologies requiring joint fusion. This technique is particularly relevant in cases involving coexisting disease or damage of the tibiotalar and subtalar joints. Common indications for TTC arthrodesis include post-traumatic ankle deformities, advanced subtalar osteoarthritis, rheumatoid arthritis, talar avascular necrosis, adult-acquired flatfoot, non-unions, failed ankle arthroplasty or previous fusion attempts, and certain tumor reconstructions [1].
Traditional open approaches, though effective in providing solid fixation, often require extensive soft tissue dissection and are associated with significant post-operative wound complications, especially in patients with pre-existing comorbid conditions, such as diabetes, immunosuppression, or poor vascularity [2,3].
Minimally invasive techniques, particularly those utilizing arthroscopic assistance, have been developed to mitigate these risks [2,4]. Arthroscopic TTC fusion offers the advantage of reduced soft tissue trauma, lower complication rates, and faster post-operative recovery [4,5]. However, achieving stable fixation of both the ankle and subtalar joints remains a technical challenge, especially when using multiple screws. In this context, the use of a locked intramedullary nail under arthroscopic guidance provides a potentially more stable and less invasive alternative [5].
Despite its growing popularity, the literature on arthroscopically assisted TTC fusion with locked intramedullary nailing remains limited. This case report aims to contribute to the evolving understanding of this technique by detailing its application, technical nuances, and clinical outcome in a complex hindfoot pathology [6].
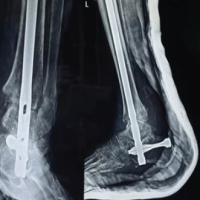
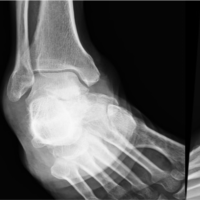
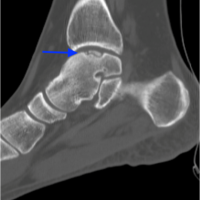
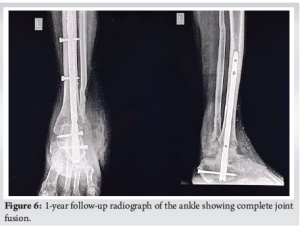
Here we report a case of 44-year-old male, a farmer by occupation, who presented to us with complaints of difficulty in weight bearing with ankle instability after he sustained a degloving injury over the lateral aspect of his left lower limb after being run over by a tractor 3 months back. At that time, he had a compound injury of the left ankle with distal fibula bone loss for which debridement of the necrotic tissue with an anterolateral thigh flap for wound coverage was done. On examination, the flap was present which was healed and accepted, the patient had significant mediolateral instability in the ankle and subtalar joint, varus opening, and antalgic gait with giving away sensation while walking. A plain radiograph of the ankle joint was ordered which showed complete loss of distal one-third of the fibula as shown in (Fig. 1). Basic blood investigations, chest radiograph, and pre-anesthetic work-up were performed. Pre-operative American Orthopaedic Foot and Ankle Society (AOFAS) score was 18/100 and the Foot and Ankle Disability Index (FADI) score was 26/104. Being a farmer, the patient wanted a stable, plantigrade, and pain-free limb for which arthroscopic ankle arthrodesis using an intramedullary tibio-talo-calcaneal nail was planned. In this case, the technique resulted in a stable, plantigrade, and pain-free limb, allowing for early mobilization without expected wound complications. At the 1-year post-operative follow-up as shown in the last figure, there was a notable improvement in clinical and functional outcomes, as evidenced by significant increases in AOFAS and FADI scores.

Surgical technique
Under spinal anesthesia, the patient was placed prone with a thigh tourniquet applied. The ankle was kept in neutral dorsiflexion with a bolster under the distal leg. Using a 4.5 mm, 30° arthroscope, posterior ankle arthroscopy was performed.
Step-1: TTC arthroscopy
The arthroscopic TTC arthrodesis procedure began with the creation of posterolateral and posteromedial portals near the Achilles tendon. An additional accessory portal was also created as shown in (Fig. 2). A 4.5-mm scope was inserted, and the trocar was positioned for optimal visualization. The shaver was used to remove fatty tissue and joint capsule as shown in (Fig. 3). Key anatomical structures, including the posterior talar process, ankle joint, subtalar joint, and flexor hallucis longus tendon were identified, while scar tissue around the flexor hallucis longus tendon was cleared to create a safe working zone. Reaming started from the posterior to the anterior tibiotalar joint, followed by debridement of cartilage using burrs and curettes to expose the subchondral bone.

Step-2: Nail insertion
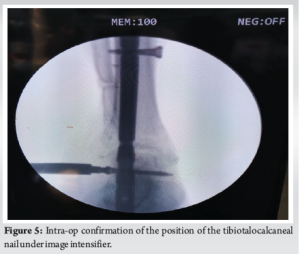
The tibia, talus, and calcaneus were carefully aligned to maximize bone contact and create a plantigrade foot. The hindfoot was positioned at 0° dorsiflexion, 5° heel valgus, and 5–10° external rotation. After debriding both articular surfaces, a guidewire was inserted as shown in (Fig. 4) through the subtalar and tibiotalar joints under arthroscopic guidance. Once the intramedullary reaming was completed, the appropriately sized retrograde nail was inserted, and confirmed under the image intensifier as shown in (Fig. 5). The proximal screw was inserted first followed by a talar screw and at last calcaneo-cuboid screw with compression device was inserted. Following the procedure, the ankle was stabilized in a below-knee plaster cast for a duration of 3 weeks to ensure immobilization and promote soft tissue healing. Graduated partial weight-bearing with bilateral axillary crutches was commenced at the 4-week post-operative mark to progressively restore functional mobility while minimizing stress on the healing structures (Fig. 6).
In this case, arthroscopic TTC arthrodesis provided an excellent functional outcome for a patient with post-traumatic ankle instability and soft tissue compromise following a high-energy injury and flap coverage. Minimally invasive and arthroscopic approaches offer several advantages over traditional open surgery. These include reduced soft tissue disruption, lower infection rates, and better preservation of the vascular supply, all of which are particularly beneficial in compromised patients. Arthroscopy specifically facilitates accurate joint preparation and debridement, even in anatomically distorted joints, allowing effective fusion while minimizing risks associated with open exposure [7,8]. In our case, arthroscopic joint preparation followed by retrograde nail insertion achieved a stable and plantigrade foot, enabling early mobilization. This is consistent with the findings of Sekiya et al., who reported successful fusion in eight of nine ankles using a finned intramedullary nail through an arthroscopic approach, with minimal complications even in patients with rheumatoid arthritis and poor bone quality [7]. Furthermore, studies by Vila y Rico et al. and Biz et al. support the use of retrograde nails in a minimally invasive setting, citing significant improvements in patient-reported outcomes, early fusion, and low complication rates [8,9]. Tuckett et al. and Kulakli-Inceleme et al. highlighted these challenges in randomized and retrospective studies, showing that TTC nailing allows immediate weight bearing and reduces the need for secondary procedures in elderly and high-risk patients [10,11]. Adverse outcomes such as nail breakage, nonunion, and subsequent reoperations have been observed, particularly among patients with comorbidities, such as diabetes or Charcot neuroarthropathy [12,13]. In contrast, our case benefitted from precise and meticulous alignment, adequate compression, and comprehensive post-operative care, which collectively helped prevent such complications and led to a successful recovery. A 2023 systematic review by Lameire et al. noted an 86% fusion rate and low infection risk using this approach, supporting its utility in cases with prior trauma or soft tissue compromise [14]. One of the studies included in the review compared arthroscopic and open TTC arthrodesis in high-risk patients [15]. It reported excellent union rates for both techniques but surgical site infections occurred in 50% of cases treated with open TTC fusion, whereas none of the arthroscopic procedures resulted in major infections. Thus, the outcomes of our case are consistent with present evidence supporting arthroscopic TTC arthrodesis as a safe and effective alternative to open techniques, particularly in patients with poor skin condition or complex ankle pathology. Despite promising results, there is a paucity of literature on arthroscopic TTC arthrodesis with intramedullary nails. Larger prospective studies are needed to standardize protocols and confirm its efficacy and safety across varied patient populations.
Arthroscopic TTC arthrodesis using intramedullary nail fixation is a reliable, minimally invasive technique for complex hindfoot conditions, particularly in patients with compromised soft tissues, pre-existing co-morbidities, or previous trauma. It ensures adequate joint stability, allows early movement, and yields excellent functional outcomes.
Arthroscopic TTC nailing is an effective and less invasive alternative for TTC fusion, especially beneficial in high-risk patients or those with poor soft tissue condition and hence, should be preferred in such cases.
References
- 1.Sekiya H, Horii T, Kariya Y, Hoshino Y. Arthroscopic-assisted tibiotalocalcaneal arthrodesis using an intramedullary nail with fins: a case report. J Foot Ankle Surg. 2006 Jul-Aug;45(4):266-70. [Google Scholar | PubMed]
- 2.Eleftheropoulos A, Giannaros IV, Christou A, Petrakis IG. Posterior arthroscopic tibiotalocalcaneal fusion: Surgical technique and early results. Foot Ankle Orthop 2016;1:1-5. [Google Scholar | PubMed]
- 3.Gong JC, Zhou BH, Tao X, Yuan CS, Tang KL. Tibiotalocalcaneal arthrodesis with headless compression screws. J Orthop Surg Res. 2016 Aug 19;11(1):91. [Google Scholar | PubMed]
- 4.Steele JR, Lazarides AL, DeOrio JK. Tibiotalocalcaneal arthrodesis using a novel retrograde intramedullary nail. Foot Ankle Spec 2020;13:463-469 [Google Scholar | PubMed]
- 5.Alexander BK, Arguello AM, Shah AB. Tibiotalocalcaneal nail failure in a 60-year-old male: Case report and surgical technique. J Clin Orthop Trauma 2020;11:482-6. [Google Scholar | PubMed]
- 6.International Orthopaedics. Tibiotalocalcaneal arthrodesis with a retrograde intramedullary nail: A prospective cohort study at a minimum five-year follow-up. Int Orthop 2021;45:2299-305. [Google Scholar | PubMed]
- 7.Sekiya H, Horii T, Sugimoto N, Hoshino Y. Arthroscopic tibiotalocalcaneal arthrodesis with intramedullary nail with fins: A case series. J Foot Ankle Surg 2011;50:589-92. [Google Scholar | PubMed]
- 8.Vila y Rico J, Rodriguez-Martin J, Parra-Sanchez G, Lopez-Amor CM. Arthroscopic tibiotalocalcaneal arthrodesis with locked retrograde compression nail. J Foot Ankle Surg 2013;52:523-8. [Google Scholar | PubMed]
- 9.Biz C, Hoxhaj B, Aldegheri R, Iacobellis C. Minimally invasive surgery for tibiotalocalcaneal arthrodesis using a retrograde intramedullary nail: Preliminary results of an innovative modified technique. J Foot Ankle Surg 2016;55:1112-9. [Google Scholar | PubMed]
- 10.Tuckett P, Hope M, Tetsworth K, Van De Pol J, McDougall C. Transarticular tibiotalocalcaneal nailing versus open reduction and internal fixation for treatment of the elderly ankle fracture: Protocol for a multicentre, prospective, randomised controlled trial. BMJ Open 2019;9:e026360. [Google Scholar | PubMed]
- 11.Kulakli-Inceleme E, Tas DB, Smeeing DP, Houwert RM, van Veelen NM, Link BC, et al. Tibiotalocalcaneal intramedullary nailing for unstable geriatric ankle fractures. Geriatr Orthop Surg Rehabil 2021 Jun 17;12:21514593211020705. [Google Scholar | PubMed]
- 12.Kowalski C, Stauch C, Callahan R, Saloky K, Walley K, Aynardi M, Juliano P. Prognostic risk factors for complications associated with tibiotalocalcaneal arthrodesis with a nail. Foot Ankle Surg. 2020 Aug;26(6):708-711. [Google Scholar | PubMed]
- 13.Levinson J, Reissig J, Schaheen E, Lee W, Park J. Complications and Radiographic Outcomes After Tibiotalocalcaneal Fusion With a Retrograde Intramedullary Nail. Foot Ankle Spec. 2021 Dec;14(6):521-527. [Google Scholar | PubMed]
- 14.Lameire DL, Abdel Khalik H, Del Balso C, Daniels T, Halai M. Transportal Tibiotalocalcaneal Nail Ankle Arthrodesis: A Systematic Review of Initial Series. Foot Ankle Orthop. 2023 Feb 28;8(1):24730114231156422. [Google Scholar | PubMed]
- 15.Baumbach SF, Luer K, Schröder M, Wiewiorski M, Zwicky L, Valderrabano V. Comparison of arthroscopic to open tibiotalocalcaneal arthrodesis in high-risk patients. Foot Ankle Surg 2018;24:492-8. [Google Scholar | PubMed]