The treatment and post-operative management of elbow pathologies in the younger population can be difficult to treat, but using interpositional arthroplasty with a post-operative hinged elbow brace is a viable option in high-demand patients.
Dr. Morgan Turnow, Department of Orthopedic Surgery, OhioHealth Doctors Hospital, 5100 W. Broad Street, Columbus, Ohio, United States. E-mail: morgan.turnow@ohiohealth.com
Introduction: The treatment of post-traumatic elbow arthritis poses a significant challenge for orthopedic surgeons, especially in young active patients. Total elbow arthroplasty is often the recommended treatment option in older patients; however, interpositional arthroplasty remains a viable option in high-demand patients.
Case Report: We report a case of a 50-year-old male who presented after the development of post-traumatic arthritis of the elbow after multiple prior surgeries. He was treated with an interpositional arthroplasty using an Achilles tendon graft and allowed immediate range of motion as tolerated in a hinged elbow brace without the use of any form of distraction external fixation. At his final follow-up, he has significantly improved pain, range of motion, and patient-reported Visual Analog Scale , American shoulder and elbow surgeons, mayo elbow performance score, and disabilities of the arm, shoulder and hand scores.
Conclusion: This case report demonstrated that interpositional arthroplasty is a viable option for managing post-traumatic elbow osteoarthritis in young patients and with good ligamentous stability, immediate protected range of motion, as tolerated, can lead to excellent outcomes.
Keywords: Elbow, arthroplasty, interpositional arthroplasty, post-traumatic elbow osteoarthritis, case report.
Elbow pathologies in younger patient populations can be difficult to treat, and long-term complications, including pain, non-union, and stiffness, can be debilitating [1]. Different pathologies of the elbow joint can arise from aging or prior trauma, including fractures of the distal humerus, which account for approximately 2% of all fractures in adults [2]. Operative treatment is often recommended for these fractures to restore motion and function. Treatment options for post-traumatic arthritis include fusion, prosthetic replacement, debridement, soft tissue contracture release, and arthroplasty [3]. Total elbow arthroplasty (TEA) is a consideration for primary treatment of severe elbow pathologies; however, it is limited in its indications secondary to the functional limitations that follow. In addition, TEA can be indicated as a salvage procedure when there is failure of primary fixation with plates and screws or post-traumatic changes [4]. After undergoing TEA, patients are subject to strict activity limitations, which are problematic for the working population or younger patients [5]. A viable alternative to this is the elbow interpositional arthroplasty, which allows for greater functional motion in comparison to TEA without the strict lifting restrictions [1]. The addition of tissue into the joint space helps prevent painful contact over the arthritic joint. Here we present a case report of a patient who experienced an intra-articular distal humerus fracture and underwent open reduction and internal fixation that was later revised to an elbow interpositional arthroplasty due to the development of post-traumatic osteoarthritis. Most previously reported case series utilized some form of distraction or hinged external fixation post-operatively. In this patient, we allowed immediate range of motion as tolerated after surgery while wearing a hinged elbow brace. He did incredibly well in the post-operative period and has no concerns at this time.
A 50-year-old right-hand dominant male presented to the orthopedic office for evaluation of chronic right elbow pain. He states this has been ongoing since he sustained an injury, while in the military, about 7 years ago. Over this period, he underwent 7 different surgeries related to this injury, with the most recent procedure in January of 2011. He noted considerable pain, stiffness, and significant difficulty performing tasks at work and activities of daily living. His pre-operative Visual Analog Scale (VAS) pain score was a 10 out of 10, mayo elbow performance score (MEPS) was 15/100 (<60 indicating poor performance), American shoulder and elbow surgeons (ASES) score of 18/100, and disabilities of the arm, shoulder and hand (DASH) score of 70/100 with additional noted severe difficulty performing his required work activities as a sports photographer. He also indicated that he was unable to participate in bowling, his sport of most importance, on pre-operative questionnaires. Radiographs and a computed tomography scan were obtained, which demonstrated advanced degenerative changes in the radiocapitellar and ulnohumeral joints (Fig. 1). Given his age, job requirements, and lifestyle, we felt the patient would not be a great candidate for a total elbow replacement given the activity and post-operative weight restrictions. Instead, we recommended treatment with an interpositional arthroplasty for the treatment of his post-traumatic osteoarthritis (Figs. 2 and 3).

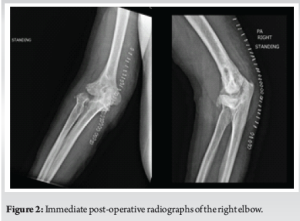

To begin the procedure, a curvilinear incision was made over the posterior aspect of the elbow. Medial and lateral full-thickness soft tissue envelopes were developed, and the ulnar nerve was identified and gently retracted with a vessel loop. There was significant scarring throughout the cubital tunnel. A lateral para-olecranon approach to the elbow joint was used, which has been described by Studer et al. [6] The triceps were significantly scarred down to the posterior aspect of the distal humerus from prior surgeries. A scalpel was used to remove the collateral ligament origin on both the medial and lateral epicondyle to skeletonize the distal humerus. There was significant scarring throughout the anterior and posterior aspects of the joint capsule; therefore, an extensive capsular release was performed to obtain adequate mobility of the elbow to allow for dislocation. A bur was used on the remaining cartilage of the trochlea and capitellum to create a bleeding portion of subchondral bone. A 2 mm drill bit was used to drill 3 holes from posterior to anterior and just proximal to the articular surface of the distal humerus. The Achilles tendon allograft was then prepared and affixed to the distal humerus with #2 Fiber Wire for added lateral stability. One Arthrex 4.75 mm swivel lock anchor was inserted in the ulnar collateral ligament origin at the anterior inferior aspect of the medial epicondyle, and a second 4.75 mm swivel lock anchor was placed in the isometric point of the lateral epicondyle. The lateral ulnar collateral ligament was then repaired back to the distal humerus, resulting in excellent stability of the lateral aspect of the joint. This technique was then repeated for the ulnar collateral ligament, back to the inferior aspect of the medial epicondyle, with excellent medial stability of the elbow joint. The common flexor and common extensor origins were then repaired back to their original spot on the distal humerus. The medial and lateral windows were closed with an excellent repair of the deep soft tissues. Following the closure of the deep soft tissues, the patient had an excellent range of motion with flexion to approximately 140° and near full extension, lacking the last 15°, which was significantly improved from the pre-operative range of motion. The ulnar nerve transposition was then performed subcutaneously, and the incisions were closed. No complications occurred during the procedure. Post-operatively, the patient was placed in a posterior slab splint without active range of motion of the right elbow. At the second post-operative visit 2 weeks later, the patient was placed in an unlocked hinged elbow brace with motion as tolerated and advised to follow-up with occupational therapy. During this visit, he also noted mild paresthesia’s in the ulnar nerve distribution. At his 5-month post-operative visit, the patient stated he was overall pleased with the surgery, and the paresthesia’s in the right ulnar nerve distribution had significantly improved. On exam, the patient was able to range from 10° to 120° of flexion, 10° of supination, and 80° of pronation without pain. His post-operative course has been uncomplicated up to this point with excellent pain control and functional range of motion. The patient was seen at his past post-operative visit 2.5 years out from surgery and stated that he was overall “very satisfied” with his elbow and surgical outcome. His range of motion continued to improve with 10°–125° of flexion, 10° of supination, and 90° of pronation. His self-reported VAS pain score was 0/10, MEPS had improved to 100/100, ASES scores 100/100, DASH score of 0/100, but indicated on the optional form that he was still unable to participate in his bowling.
Elbow interpositional arthroplasty is a salvage procedure used in young, healthy, active patients for post-traumatic osteoarthritis. Although this procedure is rarely performed, previous studies have shown satisfactory functional outcomes, and it is considered a viable alternative treatment to TEA [7]. A study conducted by Ersen presented a small case series that underwent an Achilles allograft interposition. They reported good outcomes with improved range of motion for all patients and no revision surgeries [8]. In addition, a recent systematic review including 122 studies demonstrated that patients undergoing interposition arthroplasty (IPA) of the elbow demonstrated positive improvements and pain and function [9]. The overall post-operative pain scores and Mayo Elbow Performance Index functional scores had both improved in patients <65 years of age, demonstrating its use in patients as opposed to undergoing a TEA [9]. Another retrospective study by Larson and Morrey studied a total of 69 elbows that were treated with an Achilles tendon allograft. The mean flexion-extension arc was significantly improved from 51° pre-operatively to 97° post-operatively [10]. In this study, it was reported that MEPS improved by 41 points from pre-operative to post-operative assessments; however, outcomes varied widely between excellent to poor, with 7 patients requiring revision [10]. Of note, data regarding the type of allograft selection vary widely. A systematic review by Almeida et al. found allograft selection to vary with reports of the use of Achilles grafts as well as fascia lata. They found there to be varied results with no strong evidence regarding graft choice [11]. A downside to performing an IPA is the high rate of revision, which is currently around 20% as reported in the literature [7]. This number does vary widely from study to study, with some studies reporting revision rates as low as 8.8%, and others reporting rates as high as 33.3% [10,11,12]. Despite this, 90% of published studies evaluating IPA in the elbow report results as positive rather than negative [11]. This subjective rating has little clinical value but does give insight into the subjective outcomes in the setting of a procedure, such as this that lacks substantive randomized data. The post-operative protocol for instability remains a debated topic in the literature. Multiple studies have included an external fixator as a part of their post-operative protocol to help with preventing instability after fixation [1,10,13]. While this may help with post-operative stability, complications, including stiffness and wound complications with pin site-related problems, are a possibility. In our case, the patient did exceptionally well with range of motion as tolerated 2 weeks after surgery in a hinged elbow brace as opposed to an external fixator. The main factor when deciding to allow patients early range of motion is the patient’s overall elbow stability and competency of the collateral ligaments. The decision on in situ release versus transposition of the ulnar nerve during the procedure is another factor to consider when deciding to immobilize the elbow during the initial post-operative course. In our case, stability and adequate range of motion were achieved in the operating room; however, an ulnar nerve transposition was performed, and since this patient was active pre-operatively, we decided to immobilize him for the first 2 weeks. Our study reports a case of a 50-year-old male who underwent an IPA of his right elbow in the setting of severe post-traumatic arthritis. TEA was an option for this patient, but given his young age and functional requirements, an IPA was elected as the treatment of choice. Literature, as described above, supports this as a salvage procedure with mixed results. The patient described in this study had a follow-up of 2.5 years and an excellent outcome. He was instructed to return to the orthopedic office for any concerns or further follow-up.
IPA is often considered a salvage procedure for the treatment of severe elbow arthritis when a total joint replacement is contraindicated or the patient has failed conservative management. Our patient had a significant improvement in range of motion and pain after the elbow IPA was performed, and he was allowed early protected range of motion as tolerated while in a hinged elbow brace. To date, he is back to work and is exceptionally satisfied with his outcome, with notable improvements in VAS, ASES, MEPS, and DASH scores.
IPA is a viable treatment option for young, active, high demand patients with post-traumatic arthritis. Post-operatively, we have shown that a hinged elbow brace is an option as opposed to an external fixator.
References
- 1.Morrey M, Dutta A, Whitney I, Morrey B. Interposition arthroplasty: Current indications, technique and expectations. J Clin Orthop Trauma 2021;19:175-82. [Google Scholar | PubMed]
- 2.Lauder A, Richard MJ. Management of distal humerus fractures. Eur J Orthop Surg Traumatol 2020;30:745-62. [Google Scholar | PubMed]
- 3.O’Driscoll SW. Optimizing stability in distal humeral fracture fixation. J Shoulder Elbow Surg 2005;14:186S-94. [Google Scholar | PubMed]
- 4.Yetter TR, Weatherby PJ, Somerson JS. Complications of articular distal humeral fracture fixation: A systematic review and meta-analysis. J Shoulder Elbow Surg 2021;30:1957-67. [Google Scholar | PubMed]
- 5.Moro JK, King GJ. Total elbow arthroplasty in the treatment of posttraumatic conditions of the elbow. Clin Orthop Relat Res 2000;370:102-14. [Google Scholar | PubMed]
- 6.Studer A, Athwal GS, MacDermid JC, Faber KJ, King GJ. The lateral para-olecranon approach for total elbow arthroplasty. J Hand Surg Am 2013;38:2219-26.e3. [Google Scholar | PubMed]
- 7.Lanzerath F, Hackl M, Pucher CJ, Leschinger T, Uschok S, Müller LP, et al. Interposition arthroplasty for post-traumatic osteoarthritis of the elbow: A systematic review. Int Orthop 2022;46:2603-10. [Google Scholar | PubMed]
- 8.Ersen A, Demirhan M, Atalar AC, Salduz A, Tunalı O. Stiff elbow: Distraction interposition arthroplasty with an Achilles tendon allograft: Long-term radiological and functional results. Acta Orthop Traumatol Turc 2014;48:558-62. [Google Scholar | PubMed]
- 9.Gedailovich S, Monas A, Schrier R, Aibinder WR. Do outcomes of interposition arthroplasty in young patients differ based on indication? A systematic review. J Shoulder Elbow Surg 2023;32:2412-20. [Google Scholar | PubMed]
- 10.Larson AN, Morrey BF. Interposition arthroplasty with an Achilles tendon allograft as a salvage procedure for the elbow. J Bone Joint Surg Am 2008;90:2714-23. [Google Scholar | PubMed]
- 11.Almeida TB, Reis ED, Pascarelli L, Bongiovanni RR, Teodoro RL. Interposition-arthroplasty of the elbow: Systematic review. Acta Ortop Bras 2021;29:219-22. [Google Scholar | PubMed]
- 12.Cheng SL, Morrey BF. Treatment of the mobile, painful arthritic elbow by distraction interposition arthroplasty. J Bone Joint Surg Br 2000;82:233-8. [Google Scholar | PubMed]
- 13.Blaine TA, Adams R, Morrey BF. Total elbow arthroplasty after interposition arthroplasty for elbow arthritis. J Bone Joint Surg Am 2005;87:286-92. [Google Scholar | PubMed]