Combined total knee arthroplasty and open reduction with internal fixation can be an effective solution for managing rare non-union Hoffa’s fractures with joint degeneration in younger adults.
Dr. S S Khatri, Robotics by Dr. Khatri, vaishali nagar Jaipur, Rajasthan, India. E-mail: drsskhatrirobotics@gmail.com
Introduction: Coronal plane fractures of the femoral condyle, known as Hoffa’s fractures, are uncommon intra-articular injuries. Non-union of such fractures is rarely reported, particularly in younger patients, and presents a complex clinical scenario.
Case Report: A case of a 38-year-old male who reported chronic right knee pain, swelling, and difficulty in ambulation due to a non-union Hoffa’s fracture. Radiological findings indicated joint surface degeneration and instability. Given the chronicity and extent of articular damage, the patient underwent total knee arthroplasty (TKA) along with open reduction and internal fixation (ORIF) of the medial femoral condyle under spinal anesthesia. A posterior-stabilized knee system (Smith and Nephew, femur-5, tibia-5, polyethylene insert 13 mm) was implanted using Palacos bone cement. The patient recovered well and regained mobility with significant pain relief.
Conclusion: In rare cases of non-union Hoffa’s fractures with joint degeneration, combined TKA and ORIF can provide functional improvement and pain relief, even in younger adults, when performed with appropriate surgical planning.
Keywords: Non-union, Hoffa’s fracture, total knee arthroplasty, distal, internal fixation, distal femur fracture, adult, case report.
Albert Hoffa gave an initial acknowledge of this kind of fracture in the year 1904. Hoffa fractures are coronal plane fractures of the femoral condyle and are particularly rare in adolescents [1]. A non-union happens when healing or repair is not complete in an expected period of time and there is no visible healing signs for the past 3 months [2]. Hoffa fracture is very rare and incidence merely accounts for 0.65% of all types of distal femoral fractures [3]. Their diagnosis can be challenging due to inconspicuous findings on standard radiographs. Computed tomography is crucial for confirmation. According to many relative literature, they show the incidence of fracture of the medical condyle is higher than the lateral condyle [3] and occur due to high-energy trauma involving shear forces. Treatment options vary, and no consensus exists on the optimal surgical approach or fixation method. Non-union of Hoffa’s fracture is an exceedingly rare complication and often results from missed diagnosis, inadequate fixation, or conservative treatment. In young adults, non-union presents a significant management dilemma due to the dual concerns of joint preservation and long-term functional outcome. Various case reports have suggested that fractures should be treated with debridement and open reduction and internal fixation (ORIF) [4] remains the standard of care, advanced degenerative changes and chronic instability may necessitate arthroplasty as a salvage procedure. This article presents a rare case of a 38-year-old male with a non-union lateral Hoffa’s fracture managed successfully with total knee arthroplasty (TKA), highlighting the clinical decision-making and surgical outcomes.
A 38-year-old male presented with complaints of persistent right knee pain, swelling, and difficulty walking for several months. He had a history of trauma to the knee, for which he had previously received surgical ORIF screw, and afterward one more surgery was done to remove the screws. The symptoms gradually worsened, leading to restricted mobility and decreased quality of life due to this the patient is not able to walk with balanced gait. He was otherwise healthy, with no history of smoking or chronic illnesses. He reported occasional alcohol intake and had no known drug, food, or environmental allergies. On physical examination, there was localized swelling over the right knee, tenderness along the medial joint line, and reduced range of motion (ROM). The patient was unable to bear full weight on the affected limb.
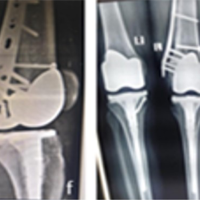
Radiographic evaluation revealed a non-union of the medial femoral condyle consistent with a chronic Hoffa’s fracture (Fig. 1-3). Joint space narrowing and irregularity of the articular surface were also observed, indicating degenerative changes. After multidisciplinary consultation and patient consent, a decision was made to proceed with TKA along with ORIF of the medial condyle.

Treatment
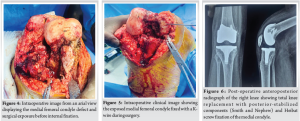
After discussing treatment options, including revision fixation, osteotomy, and arthroplasty, and given the chronic nature of the injury and degenerative articular changes, the decision was made to proceed with TKA. The procedure was performed under spinal anesthesia with full aseptic and antiseptic precautions. After painting and draping, a standard medial parapatellar incision was made. Bone cuts were taken as per protocol. Intraoperative findings revealed a fibrous non-union with articular surface damage (Fig. 4 & 5). The medial condyle non-union was exposed, debrided, and fixed using a Heibat screw for stable internal fixation.
Following fixation, trial components were assessed for proper alignment and soft tissue balancing. A posterior-stabilized knee replacement system from Smith and Nephew was implanted with the following component sizes:
- Femur: Size – 5
- Tibia: Size – 5
- Polyethylene insert: 13 mm
- Cement: Palacos (for femoral and tibial components).
After a thorough saline wash, components were cemented, and final prosthesis placement was confirmed. The surgical site was closed in layers with a drain inserted. The procedure was uneventful. The patient was monitored in the post-operative unit and began physiotherapy and mobilization with partial weight-bearing on the 2nd post-operative day and wound healing was also satisfactory.
Outcome and follow-up
The patient was monitored in the post-operative unit and began physiotherapy and mobilization with partial weight-bearing on the 2nd post-operative day. Wound healing was satisfactory, and the patient was mobilized on day 2 with partial weight-bearing using a walker. Physiotherapy was continued to regain ROM and muscle strength. Gradual weight-bearing began after 3 weeks. At the 6-week follow-up, the patient reported significant pain relief and improved ROM (0°–100°). At the 3-month follow-up, he resumed independent ambulation without support. Post-operative radiograph showed well-aligned total knee prosthesis with condylar screw fixation (Fig. 6) and no signs of loosening or infection. Radiographs confirmed healing of the fracture and osteochondral plugs.
Hoffa’s fractures are rare intra-articular injuries that require precise anatomical reduction and rigid fixation for optimal outcomes [5]. Non-union, though uncommon, may result from delayed diagnosis, inadequate initial management, or poor vascularity of the condylar fragment. In non-union fractures, the effects of age and gender are less understood and 38 out of 62 studies show the patient’s age is a risk factor for non-union fractures [6]. Conservative treatment of Hoffa’s fracture, especially in young and active individuals, is not advisable due to the intra-articular nature and propensity for complications. Our patient’s initial ORIF management was failed, likely contributed to non-union and early degenerative changes, necessitating a salvage procedure [7]. Although ORIF is preferred, in chronic non-unions with joint destruction, it may not yield functional success [8]. In such scenarios, TKA, although unconventional in younger patients, offers pain relief, correction of deformity, and restoration of function [9]. Single-compartment arthroplasty was another option considered, but for long-term results, TKA has been established by worldwide literature. On the other hand, in a review of literature showing any correlation, the use of TKA in adult male patient was not found. Kitamura et al. put light on the survival rates of implants with the relationship of age, so in age <55 years, the 5-year survival rate of implant is 92% [10]. In our case, the patient had significant improvement in function and quality of life post-arthroplasty. The long-term durability of prosthesis in young patients remains a concern, but patient selection, implant design, and rehabilitation play crucial roles in determining outcomes. Hoffa fractures require surgical stabilization due to the risks of non-union and osteoarthritis. The novel use of osteochondral plug re-implantation in this case minimized cartilage damage and preserved joint integrity. This technique may offer better long-term outcomes and deserves further study.
This case highlights the rare presentation of non-union Hoffa’s fracture and the role of TKA as a viable treatment modality in carefully selected patients. Early diagnosis and proper surgical intervention remain the mainstay of management; however, in cases with chronic non-union and advanced joint degeneration, knee replacement can offer excellent functional outcomes even in younger individuals. This approach could serve as a potential treatment standard for similar cases.
Hoffa’s fractures, if missed or not properly managed in the early stages, may lead to non union and significant loss of knee function. This case underlines the need for timely diagnosis and tailored treatment of such complex intra-articular injuries. In longstanding cases with joint degeneration and non-union, Total Knee Arthroplasty can be a valuable solution to relieve pain and restore mobility.
References
- 1.Goel A, Sabat D, Agrawal P. Arthroscopic-assisted fixation of Hoffa fracture: A case report and description of technique. J Clin Orthop Trauma 2016;7:61-5. [Google Scholar | PubMed]
- 2.Nandra R, Grover L, Porter K. Fracture non-union epidemiology and treatment. Trauma 2016;18:3-11 [Google Scholar | PubMed]
- 3.Huang G, Zhang M, Zhang Y, Wang X, Zhang M, Liu G. Hoffa fracture combined with rotational dislocation of the knee joint: A novel case report. Medicine (Baltimore) 2021;100:E25253. [Google Scholar | PubMed]
- 4.Iguchi M, Takahashi T, Nakashima M, Matsumura T, Takeshita K. Valgus knee deformity due to nonunion of lateral Hoffa fracture: A case report. Trauma Case Rep 2022;40:100662. [Google Scholar | PubMed]
- 5.Akel A, Sarhan MY, Abu-Jeyyab M, Daradkeh ST, Moseley S, Dawoud MS. Medial Hoffa fracture: A case report and literature review of approach and management. Am J Case Rep 2024;25:e943136. [Google Scholar | PubMed]
- 6.Stewart SK. Fracture non-union: A review of clinical challenges and future research needs. Malays Orthop J 2019;13:1-10. [Google Scholar | PubMed]
- 7.Reddy VG, Mootha AK, Chiranjeevi T, Kantesaria P. Total knee arthroplasty as salvage for Non Union in bicondylar Hoffa fracture: A report of two cases. J Orthop Case Rep 2011;1:26-8. [Google Scholar | PubMed]
- 8.Supe A, Atal S, Mahajan NP, Prasanna Kumar GS, Sadar A, Kondewar P. Non -union of lateral Hoffa fracture - a case report. J Orthop Case Rep 2021;11:33-6. [Google Scholar | PubMed]
- 9.Albuquerque RP, Giordano V, Amaral NP, Carvalho AC, Barretto JM. Total knee arthroplasty in a patient with hoffa fracture pseudarthrosis: Case report. Rev Bras Ortop (Engl Ed) 2011;46:460-3. [Google Scholar | PubMed]
- 10.Kitamura T, Fukui T, Matsumoto T, Oe K, Sawauchi K, Kuroda R, et al. Nonunion of Hoffa fracture successfully treated by total knee arthroplasty: A case report. Cureus 2023;15:e35780. [Google Scholar | PubMed]