Proper surgical planning and technique are crucial for achieving optimal outcomes in medial-end clavicle non-union cases with small distal fragments.
Dr. Aditya A. Agarwal, MS(Orth), PG resident, Department of Orthopedics, Grant Government Medical College and Sir JJ Group of Hospitals, Mumbai, ; Email id: dradiagr@gmail.com
Introduction: Medial end clavicle fractures are rare, constituting only 2–3% of all clavicular fractures. Although these fractures are typically managed conservatively with favorable outcomes, symptomatic non-union occurs in approximately 8% of cases, often requiring surgical intervention. Non-union, particularly in medial end fractures, presents a significant challenge due to the anatomical complexity and biomechanical forces involved. This report presents a symptomatic non-union of a medial end clavicle fracture successfully treated with dual plating, resulting in favorable clinical and functional outcomes.
Case Report: A 42-year-old male laborer with a history of chronic alcoholism sustained a medial end clavicle fracture following a fall. Initially managed conservatively, the patient presented 2 years post-injury with persistent pain, instability, and deformity. Imaging confirmed a non-union with a small distal fragment. Surgical management involved open reduction and internal fixation using a dual plating technique – utilizing a lateral end clavicle locking plate anteriorly and a superior recon plate. The procedure was successful, with no intraoperative complications. At the 12-month follow-up, the patient demonstrated radiographic union, significant improvement in the Constant-Murley score from 34 to 85, and restored range of motion without pain, enabling him to return to his previous activity level. Mild implant prominence was noted but did not necessitate removal.
Conclusion: Dual plating for medial end clavicle non-union provides enhanced stability, reduces the risk of hardware migration, and yields excellent clinical outcomes, particularly in cases involving small or unstable fragments. This technique effectively achieves union and restores function, making it a viable option in challenging clavicle non-union.
Keywords: Medial end clavicle fracture, non-union, dual plating, open reduction internal fixation, Constant-Murley score.
Clavicle fractures comprise 5–10% of all fractures, with the midshaft being the most commonly affected site. However, fractures of the medial end of the clavicle are rare, representing only 2–3% of all clavicular fractures [1]. The medial end is challenging to treat due to its anatomical proximity to vital structures, limited bone stock, and biomechanical forces that make achieving stable fixation difficult [2]. Non-union of clavicle fractures, while relatively uncommon, can lead to significant morbidity. Non-union in medial end fractures is particularly problematic, with studies showing a symptomatic non-union rate of approximately 8% in such cases. This non-union can result in chronic pain, instability, deformity, and functional limitations, profoundly impacting a patient’s quality of life [3]. The complex anatomy of the medial clavicle, coupled with the small fragment size, complicates surgical management, making it a formidable challenge for orthopedic surgeons. Medial end clavicle fractures can be commonly managed with conservative modalities, such as braces or bandages [4,5]. However, despite good clinical outcomes with conservative modality, symptomatic non-union occurs in about 8% of medial clavicular fractures [6]. In those cases, surgical management becomes a significant approach to obtaining clavicular union, preventing lasting pain, and restoring normal shoulder function in patients. At present, no single surgical modality is used to treat small oblique fragments distally to manage non-union of the medial clavicular fracture. Open reduction and internal fixation (ORIF) with plates and screws have shown fair to good outcomes in treating symptomatic non-union of medial clavicle fractures [7]. Stiff reconstructions of the sternoclavicular (SC) joint create high bending forces dissipated through the construct during the full range of movement of the shoulder girdle and clavicle, and very hard to obtain good purchase with proper fixation of metal implants, especially in non-union cases with a small medial fragment leads to early failure and migration of the implant [8]. The dual plating technique, a relatively novel approach, has been proposed to address these challenges by providing enhanced biomechanical stability in cases with small or unstable fragments. This report discusses a 42-year-old male patient who underwent dual plating for non-union of a medial end clavicle fracture, with a follow-up of 12 months, including functional outcome measures.
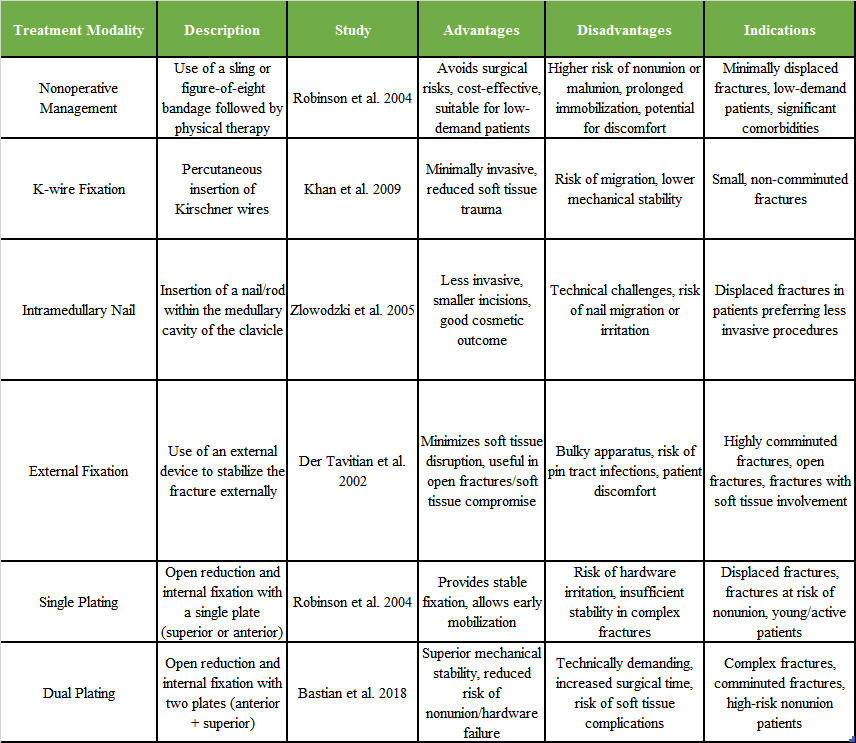
A 42-year-old male was referred from a regional center to our center for symptomatic abnormal prominence of the medial clavicle with non-union post-traumatic stress due to a fall under the influence of alcohol. The patient was a chronic alcoholic laborer from a remote village area. The patient sustained trauma in a drunken state on the right side of their clavicle. Initially, the patient didn’t consult for the trauma. The patient has taken local treatment in the form of medication and sling support for pain and swelling for 3 weeks. The patient is a laborer from a remote village area, and after 3 weeks, he resumed his work but was in some pain. The pain continued later on, and he noticed swelling over the medial end of the clavicle after a few months. The patient continued ice fomentation and pain medications for nearly 20–24 months. After almost 2 years, they came to our center for pain and sensation of instability at the fracture site with abnormal prominence fragments over the skin (Fig. 1). We have assessed him clinically and done the basic X-ray (Fig. 2a) and computed tomography (CT) scan (Fig. 2b, c, d) with 3D reconstruction. Range of movement at the shoulder joint abduction around 50° with pain further 20° is possible, rotation 30 external rotation and 40° of internal rotation with mobility in the vertical plane with mild tenderness (not significant) with neurological strength of abductor and rotator grade 4 might be due to pain and instability. Radiologically (X-ray and CT scan) found to be a non-union of the medial end of the clavicle with a tiny medial fragment with complete overlapping and abnormal prominence at the fracture site (poking skin). The patient is a laborer and wanted stable fixation with functional movement at the shoulder joint.

Figure 1: Clinical image showing abnormal prominence and swelling at the medial end of the clavicle before surgery.
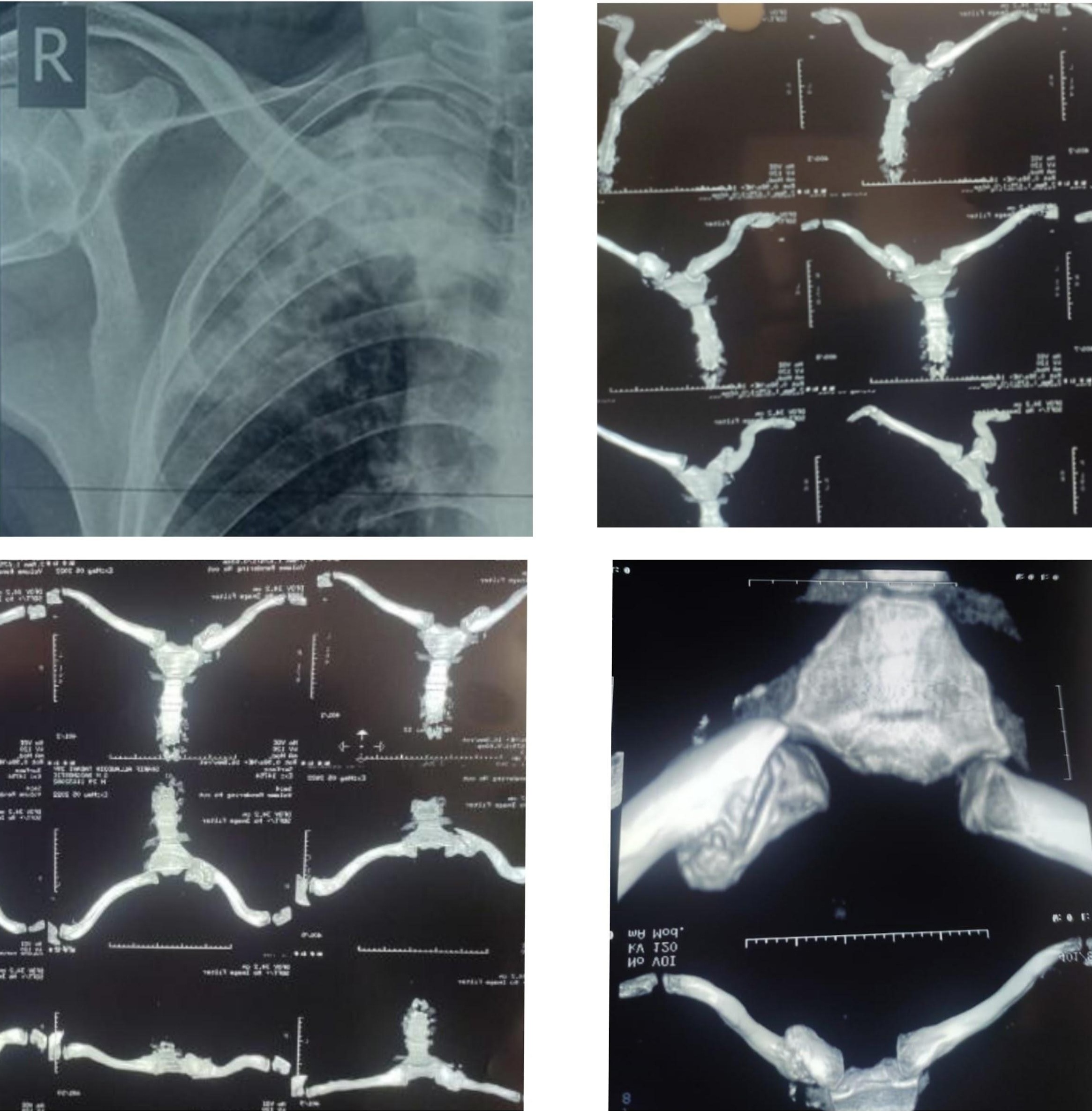
Figure 2: (a) Pre-operative X-ray showing non-union of the medial end clavicle fracture with overlapping fragments. (b) computed tomography (CT) scan axial view confirming non-union with a small medial fragment. (c) CT sagittal reconstruction showing complete overlap at the fracture site. (d) CT 3D reconstruction illustrating the extent of non-union and fragment anatomy.
Operative procedure
Surgical management of the non-union with an ORIF was performed under interscalene block with sedation. In a semi-sitting position, the non-union site was opened using a 10-cm longitudinal incision at the SC joint. The fracture site was exposed, edges curated, and hypertrophic callous was removed from the lateral sharp overriding edge (Fig. 3a), both edges have bleeding bone, approximated fixed by using left-sided lateral end clavicle locking plate (usually lateral portion could fit on the clavicle medial end) anteriorly with 4, 2.7 mm locking screw in medial fragment and 3, 3.5 mm cortical locking screw in the lateral fragment (Fig. 3b). Intraoperatively we found the purchase of 2 screws in the medial fragment unstable. Hence, we have augmented the fixation with a 3.5 mm recon plate superiorly with two simple screws in the medial fragment and two simple screws in the lateral fragment (Fig. 3c). A stable fixation was obtained without bridging the SC joint. The c-arm image is attached (Fig. 4).

Figure 3: (a) Intraoperative image showing the hypertrophic callus at the fracture site after exposure. (b) Fixation with lateral end clavicle locking plate anteriorly. (c) Augmentation with a superior recon plate for enhanced stability.
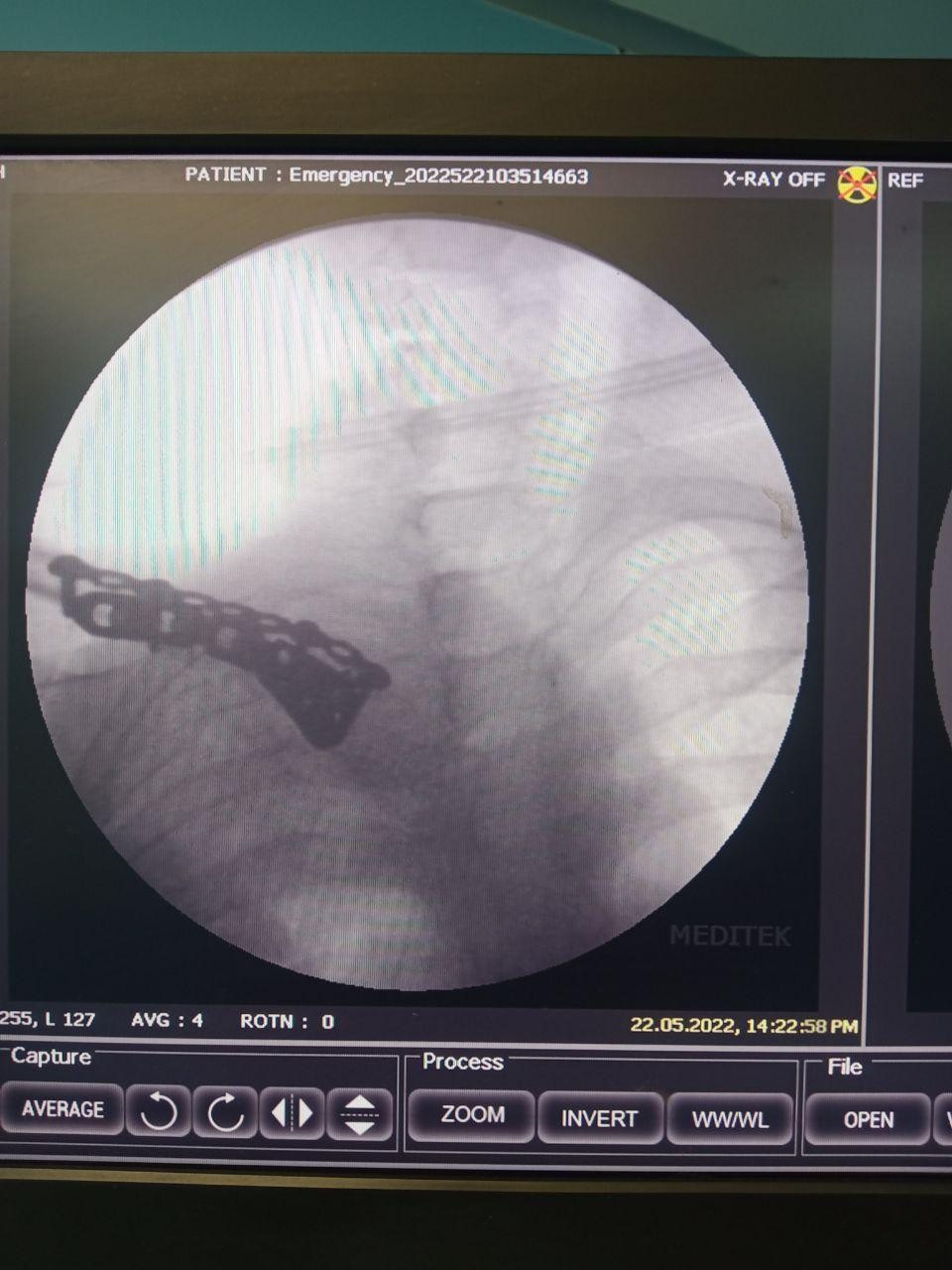
Figure 4: Intraoperative fluoroscopy (C-arm) image confirming stable fixation with dual plating.
Surgery was tolerated well, with blood loss of approximately 200 ccs; the wound was washed and closed in layer, 48 h IV antibiotic (cefuroxime) was given, and shifted to an oral antibiotic (cefuroxime axetil) for five more days.
Post-operative rehabilitation
Two weeks of immobilization in a sling were recommended to the patient, and the suture was removed on post-operative day 14th. The sling was removed intermittently and mobilized to achieve the shoulder range of movement.
Outcome
At 12 months follow-up, the X-ray (Fig. 5a and b) showed union with the implant in situ; there was no evidence of implant breakage. At the 12-month functional range of movement, good internal rotation is 80, and external rotation is 90. Abduction ranges from 100 to 110 clinical images (Fig. 6a and b). The pre-operative Constant-Murley score was 34, indicating severe impairment. Post-operatively, this score improved significantly to 85, reflecting good functional recovery. Without any pain, there was hardware prominence. However, the fracture was united, and the function of the shoulder was good, with a good functional range of movement. The patient could return to his previous activity level and perform his daily activities without limitations. The patient was informed about the option of implant removal should the symptoms persist or worsen.

Figure 5: a) Postoperative X-ray at 12 months showing union of the fracture with implants in situ. b) Lateral X-ray confirming union and absence of hardware failure.
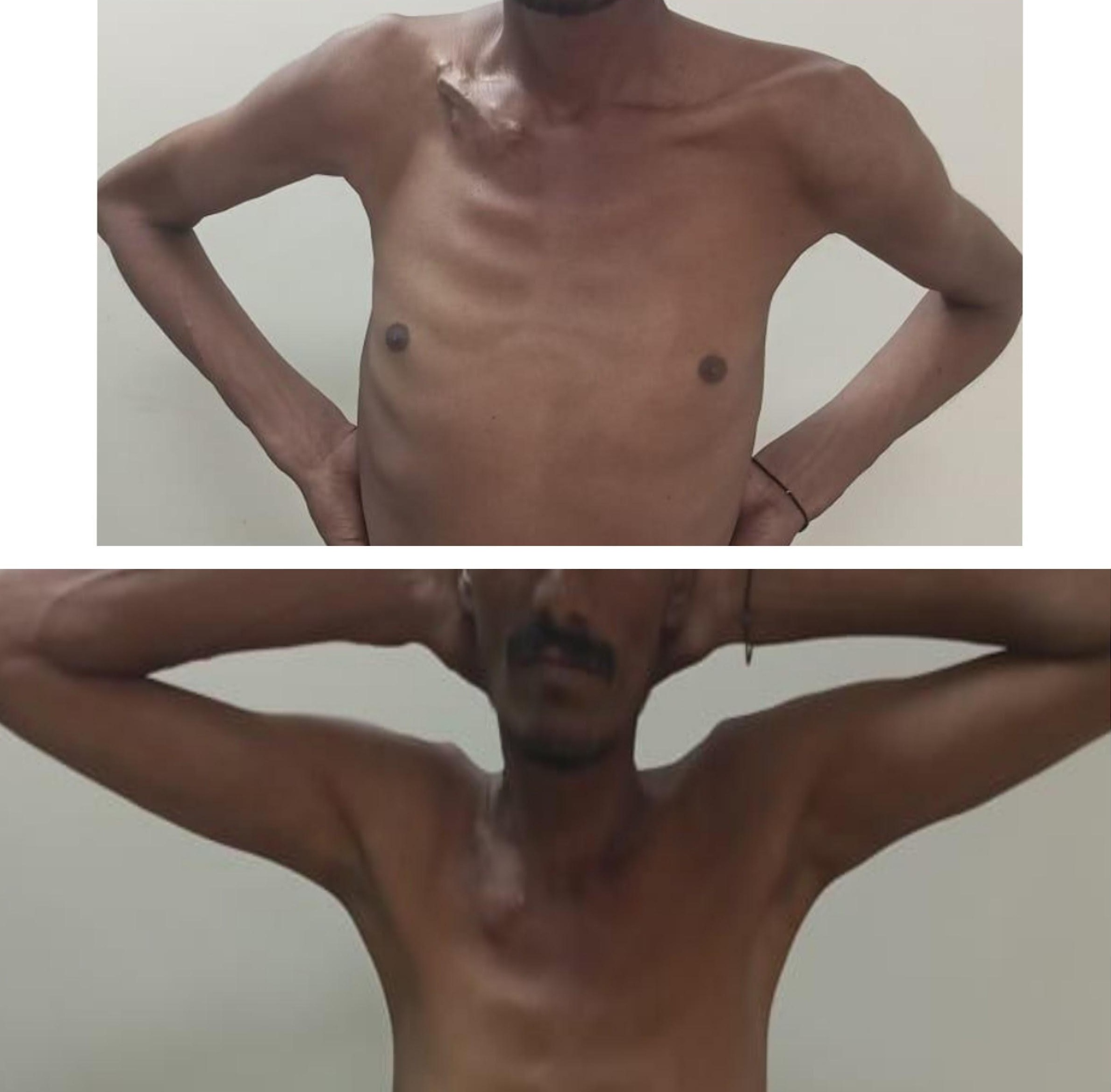
Figure 6: (a) Clinical image at 12 months demonstrating good shoulder abduction. (b) Clinical image showing full internal and external rotation without pain.
Non-union in medial end clavicle fractures is a significant clinical issue due to the complex biomechanics and limited blood supply at the fracture site. The fragment’s small size and the SC joint’s constant motion contribute to the difficulty in achieving union with conservative management alone. Chronic alcoholism further exacerbates these challenges, impairing the body’s ability to heal effectively [3]. Although our patient achieved successful union, it is important to acknowledge that chronic alcoholism is a known risk factor for delayed or impaired fracture healing. Thus, the reproducibility of these results across diverse patient populations with different comorbidities may vary. Because the option of revision surgery is limited due to the small medial fragment, if case fixation fails, the next option will be the excision of the medial fragment with stabilization of the SC joint by ethibond of the tendon autograft. Soft tissue reconstruction of the SC joint with resection of the medial end of the clavicle is the commonly used treatment for chronic SC instability [8,9].
Traditional fixation methods, such as Kirschner wires, intramedullary fixation, and single-plate fixation, often fall short in cases with small or comminuted fragments due to inadequate stabilization and the risk of hardware failure [5,10,11]. In contrast, the dual plating technique provides robust stabilization by engaging two planes of the clavicle, thereby distributing the biomechanical forces more effectively and minimizing the risk of implant failure. A comparison of dual plating with other modalities is presented in Table 1.
The literature suggests that dual plating significantly improves union rates and functional outcomes compared to other modalities, particularly in challenging cases involving small fragments. This is corroborated by studies, such as Bastian and Itamura, which report similar success with dual plating in recalcitrant cases of medial clavicle non-union [12]. Biomechanical analysis has shown higher torsional and bending stiffness, which are critical for the healing process of clavicle fracture. Dual orthogonal plating constructs were significantly stiffer and had a higher load to failure compared to traditional superior plating [13]. The improvement in the Constant-Murley score from 34 pre-operatively to 85 post-operatively highlights the efficacy of dual plating in restoring shoulder function. Similarly, the marked improvement in range of motion (ROM) further underscores the benefits of this technique in non-union, where functional impairment has been prolonged. Compared to single plating and other methods, dual plating offers superior functional recovery, as evidenced by the higher post-operative functional scores in our case and similar cases reported in the literature. Our study lacks a direct comparative group against these established techniques, which limits the strength of conclusions regarding superiority of dual plating. Incorporating patient-reported outcome measures and advanced imaging, such as CT for follow-up in future studies would enhance the accuracy of functional and radiological assessment and avoid underestimating subtle complications or residual functional deficits. The most significant complication observed was implant prominence under the skin, particularly with the superior plate. This is a known issue with dual plating, particularly in patients with thin, soft tissue coverage. While the discomfort was mild in our patient and implant removal was not required, the potential for a second surgery remains an important consideration in the overall risk–benefit evaluation of this method. The dual plating technique appears to have a low overall complication rate compared to other methods, with most issues being minor and manageable. The follow-up duration in this report was 12 months, which, while sufficient to establish union and functional recovery, is relatively short to comment on long-term outcomes. Longer-term studies are warranted to fully validate the durability of this approach. Finally, it must be emphasized that this case was treated in a tertiary referral center with adequate surgical expertise. The reproducibility of outcomes may vary in centers with limited experience in clavicular non-union surgery, potentially affecting safety and results.Medial end clavicle fractures pose significant challenges in management, mainly when non-union occurs. The dual plating technique offers a robust solution for achieving stable fixation, particularly in cases involving small or comminuted fragments. This case demonstrates that dual plating can significantly improve functional outcomes, as evidenced by the marked improvement in Constant-Murley scores and ROM. While implant prominence remains a concern, it is a manageable complication, and the overall benefits of this technique appear to outweigh the risks. Future research with larger cohorts, longer follow-up, and comparative studies against other modalities is needed to establish the definitive role of dual plating in medial end clavicle non-union.
This case report highlights the effectiveness of dual plating in managing symptomatic non-union of the medial end of the clavicle, particularly in cases with small distal fragments. This approach is especially valuable in patients with high functional demands and those at risk of hardware failure with traditional single-plating methods.
References
- 1. Neer CS 2nd. Fractures of the clavicle. In: Rockwood CA Jr., Matsen FA 3rd, editors. The Shoulder. Philadelphia, PA: WB Saunders; 1990. p. 365-412. [Google Scholar] [PubMed]
- 2. Lazarus MD. Fractures of the clavicle. In: Bucholz RW, Heckman JD, Court-Brown CM, editors. Rockwood and Green’s Fractures in Adults. 6th ed. Philadelphia, PA: Lippincott Williams &Wilkins; 2006. p. 1216-21. [Google Scholar] [PubMed]
- 3. Wijdicks FJ, Van der Meijden OA, Millett PJ, Verleisdonk EJ, Houwert RM. A systematic review of the complications of plate fixation of clavicle fractures. Arch Orthop Trauma Surg 2012;132:617-25. [Google Scholar] [PubMed]
- 4. Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomised clinical trial. J Bone Joint Surg Am 2007;89:1-10. [Google Scholar] [PubMed]
- 5. Khan LA, Bradnock TJ, Scott C, Robinson CM. Fractures of the clavicle. J Bone Joint Surg Am 2009;91:447-60. [Google Scholar] [PubMed]
- 6. Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br 1997;79:537-9. [Google Scholar] [PubMed]
- 7. VanBeek C, Boselli KJ, Cadet ER, Ahmad CS, Levine WN. Prevalence of complications of open reduction and internal fixation of clavicle fractures. J Shoulder Elbow Surg 2011;20:86-91. [Google Scholar] [PubMed]
- 8. Renfree KJ, Wright TW. Anatomy and biomechanics of the acromioclavicular and sternoclavicular joints. Clin Sports Med 2003;22:219-37. [Google Scholar] [PubMed]
- 9. Thompson JD, von Schroeder HP. Recurrent sternoclavicular joint instability: Reconstruction with gracilis tendon autograft. J Shoulder Elbow Surg 1999;8:286-8. [Google Scholar] [PubMed]
- 10. Zlowodzki M, Zelle BA, Cole PA, Jeray K, McKee MD. Treatment of acute midshaft clavicle fractures: A systematic review of 2144 fractures. J Orthop Trauma 2005;19:504-7. [Google Scholar] [PubMed]
- 11. Robinson CM, Court-Brown CM, McQueen MM, Wakefield AE. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am 2004;86:1359-65. [Google Scholar] [PubMed]
- 12. Bastian S, Itamura J. Treatment of recalcitrant medial clavicle non-union with novel dual plating technique. Ann Case Rep 201;7:1-5. [Google Scholar] [PubMed]
- 13. Boyce GN, Philpott AJ, Ackland DC, Ek ET. Single versus dual orthogonal plating for comminuted midshaft clavicle fractures: A biomechanics study. J Orthop Surg Res 2020;15:248. [Google Scholar] [PubMed]