The rarity of bilateral discoid medial menisci in a middle-aged adult and the contrasting management strategies – surgical for symptomatic knee and conservative for asymptomatic knee – highlight the importance of individualized treatment planning.
Dr. Hsain-Chung Shen, Department of Orthopedic Surgery, Tri-Service General Hospital, National Defense Medical University, No. 325, Sec. 2, Cheng-Kung Road, Neihu, Taipei, Taiwan. E-mail: doc20231@gmail.com
Introduction: Discoid medial meniscus is rare; bilateral involvement in adults is exceptionally uncommon.
Case Report: A 52-year-old male presented with symptomatic right knee and asymptomatic left knee; magnetic resonance imaging (MRI) revealed bilateral discoid medial menisci (BDMM), with a complex tear involving the posterior horn on the right side. The right knee underwent arthroscopic saucerization of the central discoid element and partial medial meniscectomy of the posterior horn, followed by all-inside repair, whereas the left knee was managed conservatively. At the 12-month follow-up, clinical outcomes were excellent.
Conclusion: Early MRI and individualized treatment strategies are critical in adult BDMM to optimize outcomes and preserve joint function.
Keywords: Bilateral discoid medial menisci, adult, meniscal repair, saucerization, conservative management.
Discoid meniscus is an uncommon cause of internal derangement of the knee. Since Murdoch reported the first case of bilateral discoid medial menisci (BDMM) in 1956 [1], the condition has remained extremely rare, with an estimated incidence of approximately 0.012%. A literature review over the past decade identified 17 published reports describing 40 cases. The majority of reported BDMM cases occur in pediatric and adolescent populations, with adult presentations being exceptionally uncommon, Here, we describe a rare case of BDMM in a man in his 50s – highlighting not only its rarity but also the contrasting management strategies applied to each knee.
A 52-year-old male presented with right knee medial pain for 3 months, exacerbated by stair climbing and squatting, associated with popping and locking sensations. On physical examination, the range of motion (ROM) of the right knee is mildly limited by pain during flexion, medial joint line tenderness, and a positive McMurray test for the posterior horn of the medial meniscus. Gross effusion is noted, with aspiration yielding 40 cc of serous fluid containing chondral debris. Radiographs and scanography reveal no significant mechanical axis deviation, and the knee appears grossly normal on imaging. He denies any recent trauma but has a history of an old femoral fracture treated with surgical fixation and subsequent implant removal (Fig. 1).

Figure 1: Full-length frontal radiographs of both lower extremities show no significant mechanical axis deviation.
Magnetic resonance imaging (MRI) of the right knee demonstrates a medial discoid meniscus with increased thickness and abnormal morphology. A horizontal tear is identified, characterized by a linear hyperintense signal extending parallel to the tibial plateau. In addition, a complex tear involves the posterior horn, with irregular signal changes extending to the articular surface on T2-weighted images (Fig. 2).
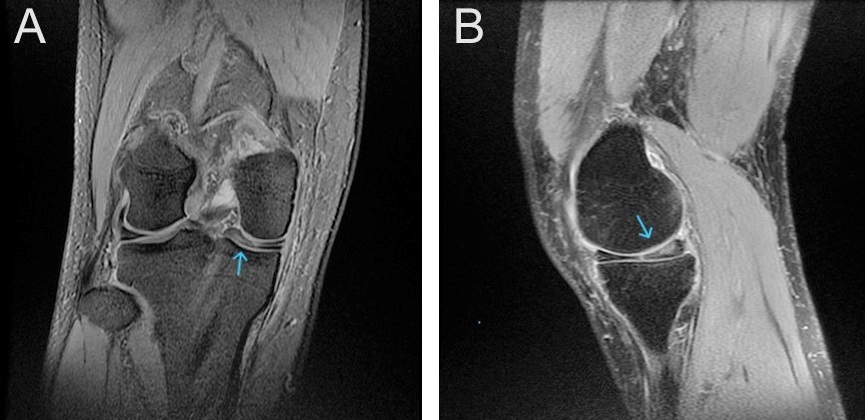
Figure 2: Coronal (a) and sagittal (b) T2-weighted magnetic resonance imaging of the right knee showing a discoid medial meniscus with complex posterior horn tear (arrow).
The patient underwent right knee arthroscopy under spinal anesthesia, with the finding of an incomplete type medial discoid meniscus and a complex tear of the posterior horn. Saucerization of the central discoid element and partial medial meniscectomy of the posterior horn were performed. Two all-inside sutures with a non-absorbable stitch were thus applied to repair the complex tear of the posterior horn (Fig. 3).
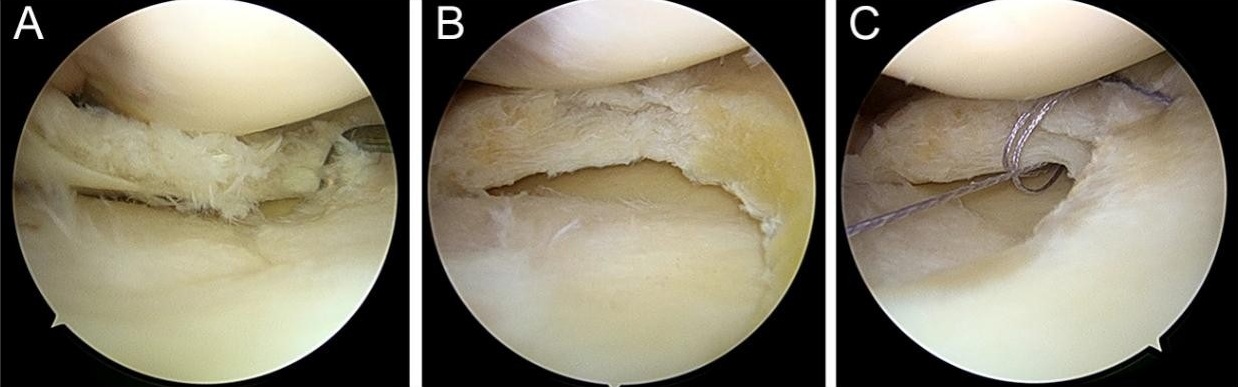
Figure 3: Arthroscopic findings of right knee: (a) incomplete-type discoid medial meniscus with complex posterior horn tear. (b) Partial meniscectomy with saucerization. (c) All-inside sutures repairing radial and horizontal tears.
A probe was used to assess the repair’s tightness and stability. Post-operative management included partial weight-bearing with crutches, a full extension brace for 2 weeks, and initiation of isometric quadriceps exercises on the 1st day. Knee flexion to 90° was allowed at 3 weeks, with full ROM and progressive strengthening after 6 weeks. Return to sports occurred at 3 months. MRI of the contralateral knee revealed a discoid medial meniscus with mild degeneration signals and minimal symptoms, which were managed conservatively (Fig. 4).
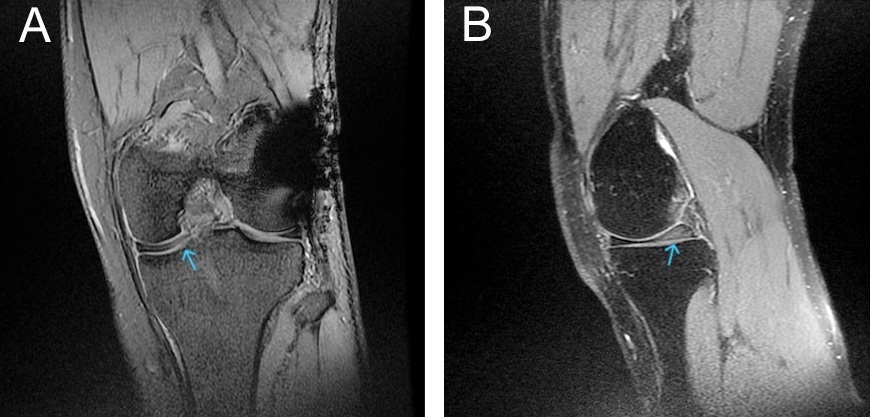
Figure 4: Coronal (a) and sagittal (b) T2-weighted magnetic resonance imaging of the left knee showing an incomplete medial discoid meniscus with intrasubstance degeneration signals (arrow).
At 12 months, the patient had full ROM, negative meniscal tests, Lysholm score of 94, International Knee Documentation Committee score of 89, and no recurrent symptoms in either knee.
Reports of BDMM remain exceptionally rare, and their true prevalence is difficult to determine, as many cases are asymptomatic and undiagnosed [4]. Patients typically present with non-specific knee pain, sometimes accompanied by mechanical symptoms such as snapping, locking, or effusion [5,6]. Joint line tenderness and a positive McMurray test are key clinical indicators [7]. Comparative studies show clear age-related differences in meniscal morphology, tear patterns, and stability. In pediatric and adolescent patients, MRI typically reveals complete-type morphology characterized by increased meniscal width and thickness relative to the tibial plateau, along with minimal secondary bony change [5,6,8]. Deficient peripheral attachments are common, predisposing to rim laxity and making horizontal cleavage or posterior-horn intrasubstance tears frequent findings [9,10,11]. Anderson et al. [5] analyzed 22 knees in patients aged 18 years or younger with a medial discoid meniscus. Among these, 12 knees (approximately 55%) displayed complete morphology. Meniscal tears were identified in 13 knees (approximately 59%), with horizontal cleavage being the most common configuration. Evidence of instability was observed in 5 menisci (23%), including three associated with posterior horn tears and two with peripheral rim insufficiency. Another pediatric series involving five knees reported that 75% had meniscal tears, predominantly horizontal cleavage patterns [6]. By contrast, in adults and middle-aged individuals, discoid menisci are more often of the incomplete type, with relatively narrower morphology. Tear patterns in this population more commonly include radial and oblique orientations, whereas degenerative or complex lesions are prevalent due to cumulative loading and microtrauma, leading to diminished tissue resilience [9,10,12]. In our case, MRI and arthroscopy confirmed an incomplete-type medial discoid meniscus with a complex posterior horn tear, consistent with adult patterns. Due to BDMM’s rarity, standardized treatment guidelines are lacking. Management must consider patient age, tissue healing potential, and degenerative changes. In children and adolescents, the primary objective is to preserve meniscal tissue and prevent early-onset osteoarthritis. Arthroscopic partial meniscectomy, commonly known as saucerization, is frequently employed to reshape the meniscus and remove unstable tissue. When peripheral detachment is present, meniscal repair may be performed to restore stability and maintain meniscal function [5,13,14]. Suzuki et al. reported favorable outcomes in a pediatric patient with symptomatic bilateral complete discoid medial menisci, demonstrating the effectiveness of arthroscopic partial meniscectomy with or without peripheral suture repair over a 5-year follow-up period [15]. In middle-aged individuals, conservative management is preferred for asymptomatic or minimally symptomatic knees, as in our patient’s left knee. Symptomatic patients may undergo partial meniscectomy; however, over-resection is discouraged due to the risk of early osteoarthritis [2,3,16]. Current consensus emphasizes meniscal preservation, recommending repair whenever feasible to restore native biomechanics and reduce degenerative progression. Advances in arthroscopic techniques, particularly all-inside and hybrid suture devices, have broadened the indications for repair, allowing treatment even in complex or horizontal tear patterns. Recent evidence in adults over 45 years shows that arthroscopic repair of degenerative medial meniscus tears yields favorable clinical outcomes with low clinical failure rates, despite incomplete MRI healing in some cases [7,17]. In our patient, the right knee showed an unstable posterior horn with a horizontal tear. A limited partial meniscectomy combined with all-inside repair was performed, achieving restored stability and preserved meniscal contour at 1-year follow-up. These findings support current trends favoring preservation, even in complex tear patterns traditionally thought to have poor healing potential. Overall, our case highlights that treatment for BDMM should be individualized: Preserving the meniscus in younger patients to prevent future degeneration, while adopting a conservative or minimally invasive approach in adults to maintain remaining joint function. The contrasting strategies in our patient’s two knees illustrate this age- and condition-dependent decision-making.
A discoid medial meniscus is uncommon, and bilateral involvement in adults is exceptionally rare. This case underscores the need to recognize BDMM in older patients and illustrates how differing knee pathology justifies distinct management strategies: Arthroscopic repair for symptomatic knees and conservative observation for asymptomatic knees. Early MRI is essential for diagnosis, pre-operative planning, and detection of contralateral asymptomatic lesions. Preservation-oriented arthroscopy remains the cornerstone for symptomatic knees, whereas conservative management is safe and effective for asymptomatic knees. Timely recognition and tailored treatment optimize long-term joint function and prevent degeneration.
We report a rare adult case of BDMM. Symptomatic knees benefit from limited meniscal reshaping and repair, whereas asymptomatic knees may be managed conservatively, achieving excellent outcomes when monitored.
References
- 1. Murdoch G. Congenital discoid medial semilunar cartilage. J Bone Joint Surg Br 1956;38-B:564-6. [Google Scholar] [PubMed]
- 2. Song IS, Kim JB, Lee JK, Park BS. Discoid medial Meniscus tear, with a literature review of treatments. Knee Surg Relat Res 2017;29:237-42. [Google Scholar] [PubMed]
- 3. Yang X, Shao D. Bilateral discoid medial Meniscus: Two case reports. Medicine (Baltimore) 2019;98:e15182. [Google Scholar] [PubMed]
- 4. Kini SG, Walker P, Bruce W. Bilateral symptomatic discoid medial meniscus of the knee: A case report and review of literature. Arch Trauma Res 2015;4:e27115. [Google Scholar] [PubMed]
- 5. Anderson KG, Carsen S, Stinson Z, Kushare I, Finlayson CJ, Nault ML, et al. Medial discoid meniscus in children: A multicenter case series of clinical features and operative results. Am J Sports Med 2023;51:1171-6. [Google Scholar] [PubMed]
- 6. Accadbled F, Sygacz O, Rassi J, Herdea A. Pediatric medial discoid meniscus: Case series and postoperative outcomes. Children (Basel) 2025;12:646. [Google Scholar] [PubMed]
- 7. Ogawa H, Matsumoto K, Sengoku M, Yoshioka H, Akiyama H. Arthroscopic repair of horizontal cleavage meniscus tears provides good clinical outcomes in spite of poor meniscus healing. Knee Surg Sports Traumatol Arthrosc 2020;28:3474-80. [Google Scholar] [PubMed]
- 8. Hashimoto Y, Nishino K, Kinoshita T, Iida K, Hiroaki N. Age-based comparison of meniscal dimensions between an asymptomatic complete discoid lateral meniscus and normal meniscus: MRI evaluation. Arch Orthop Trauma Surg 2024;144:791-8. [Google Scholar] [PubMed]
- 9. Silverstein RS, McKay SD, Coello P, Pupa L, Latz K, Craig Kemper W, et al. Relationship between age and pathology with treatment of pediatric and adolescent discoid lateral meniscus: A report from the SCORE multicenter database. Am J Sports Med 2023;51:3493-501. [Google Scholar] [PubMed]
- 10. Saavedra M, Sepúlveda M, Jesús Tuca M, Birrer E. Discoid meniscus: Current concepts. EFORT Open Rev 2020;5:371-9. [Google Scholar] [PubMed]
- 11. Ammann N, Kaelin R, Ammann E, Rutz E, Studer K, Valdarrabano V, et al. Meniscal rim instability has a high prevalence and a variable location. Arch Orthop Trauma Surg 2023;143:6113-6. [Google Scholar] [PubMed]
- 12. Patel H, Skalski MR, Patel DB, White EA, Tomasian A, Gross JS, et al. Illustrative review of knee meniscal tear patterns, repair and replacement options, and imaging evaluation. Clin Imaging 2021;69:4-16. [Google Scholar] [PubMed]
- 13. Iorio R, Viglietta E, Mazza D, Redler A, Pagnotta SM, Ferretti A. Saucerization and suture of symptomatic bilateral medial discoid meniscus in a 13 years old male football player: A case report and literature review. Orthop Rev (Pavia) 2022;14:33699. [Google Scholar] [PubMed]
- 14. Sevillano-Perez E, Espejo-Reina A, Espejo-Reina MJ. Symptomatic bilateral torn discoid medial meniscus treated with saucerization and suture. Case Rep Orthop 2016:2016:8487194. [Google Scholar] [PubMed]
- 15. Suzuki Y, Kondo E, Kaibara T, Matsuoka M, Hishimura R, Iwasaki K, et al. Symptomatic bilateral complete discoid medial menisci of the knee in a child: A case report. Jt Dis Relat Surg 2023;34:455-62. [Google Scholar] [PubMed]
- 16. Yamasaki S, Hashimoto Y, Takigami J, Terai S, Takahashi S, Nakamura H. Risk factors associated with knee joint degeneration after arthroscopic reshaping for juvenile discoid lateral meniscus. Am J Sports Med 2017;45:570-7. [Google Scholar] [PubMed]
- 17. Zhu S, Li X, Lu Z, Koh JL, Wang C, Wang P, et al. Arthroscopic repair of degenerative medial meniscus tears in patients aged over 45 years Resulted in favorable clinical outcomes and low clinical failure rates at a minimum 2-year follow-up. Knee Surg Sports Traumatol Arthrosc 2023;31:1815-23. [Google Scholar] [PubMed]