This study highlights that while conventional exercise forms the cornerstone of patellofemoral osteoarthritis management, the addition of adjunctive modalities can enhance outcomes; specifically, laser therapy combined with exercises proved more effective than longwave diathermy with exercises in reducing pain, improving mobility, and enhancing functional status, suggesting that physiotherapists may consider incorporating laser therapy into rehabilitation programs as a safe, feasible, and superior adjunct for optimizing patient recovery.
Dr. Namrata Srivastava, Department of Physiotherapy, NIMS University, Jaipur, Rajasthan, India. E-mail: nam.fdi@gmail.com
Introduction: Patellofemoral osteoarthritis (PFOA) is a common source of anterior knee pain and functional limitation, affecting quality of life and mobility in older adults. While conventional exercise remains central to conservative management, adjunctive modalities such as laser therapy and longwave diathermy are being investigated for their added benefits.
Objectives: The objective of the study is to compare the effectiveness of conventional exercises combined with laser therapy versus conventional exercises combined with longwave diathermy in reducing pain and enhancing functional outcomes among patients with PFOA.
Materials and Methods: A prospective comparative study design was adopted. A total of eligible participants with clinically diagnosed PFOA were recruited using purposive sampling from outpatient physiotherapy clinics. Participants were divided into two groups: Group A received conventional exercise therapy plus laser therapy, while Group B received conventional exercise therapy plus longwave diathermy. Interventions were provided 3 times per week for 6 weeks. Outcome measures included the numerical pain rating scale for pain, the 6-minute walk test (6MWT) for endurance and mobility, and the knee outcome survey–activities of daily living scale (KOS-ADLS) for functional status. Pre- and post-intervention data were analyzed using paired and unpaired statistical tests with a significance level of P < 0.05.
Results: Both groups showed statistically significant improvements across all outcomes post-intervention. However, Group A (exercise + laser therapy) demonstrated greater reductions in pain, longer walking distances on the 6MWT, and superior functional scores on the KOS-ADLS when compared to Group B.
Conclusion: The combination of laser therapy with conventional exercises proved more effective than longwave diathermy with exercises in improving pain and function in PFOA patients. Given the results, laser therapy may be recommended as a more beneficial adjunct to conventional rehabilitation strategies.
Keywords: Patellofemoral osteoarthritis, prospective comparative study, purposive sampling, laser therapy, longwave diathermy, pain, functional outcomes.
Patellofemoral osteoarthritis (PFOA) is a prevalent subset of knee osteoarthritis characterized by degenerative changes specifically in the patellofemoral joint, resulting in persistent anterior knee pain and impaired function. It is increasingly recognized as a distinct clinical entity that significantly contributes to disability among middle-aged and older adults [1]. Radiographically, PFOA has been identified in up to 25–40% of patients diagnosed with knee osteoarthritis, emphasizing its clinical relevance [2,3]. The patellofemoral joint endures high mechanical loads during activities such as stair climbing, squatting, and rising from a seated position, often exacerbating symptoms for patients with joint degeneration [4]. Epidemiological data indicate that PFOA disproportionately affects women and individuals with obesity, which are established risk factors. Other contributors include previous patellar trauma, malalignment, and biomechanical abnormalities like increased Q-angle and muscular imbalances [5,6,7]. These factors alter joint loading patterns, increasing cartilage stress and subsequent degradation [8]. Clinically, PFOA manifests as anterior knee pain localized to the patella or surrounding retropatellar area. Patients frequently report difficulty during weight-bearing knee flexion activities and experience joint crepitus and stiffness, leading to considerable disability and reduced quality of life [9,10]. Quadriceps weakness, especially of the vastus medialis oblique muscle, is commonly associated and contributes to further joint maltracking and pain exacerbation [11,12]. Management of PFOA primarily involves conservative strategies, with exercise therapy considered the first-line intervention. Exercise programs targeting quadriceps strengthening, hip abductor muscle conditioning, and neuromuscular control aim to improve patellar tracking, reduce abnormal joint loads, and alleviate symptoms [13,14,15]. These rehabilitation exercises have demonstrated effectiveness in improving pain and function but may be limited by patients’ baseline pain and inflammation levels, necessitating adjunctive treatments to augment outcomes [16]. Physical modalities such as low-level laser therapy (LLLT) and longwave diathermy are frequently integrated into comprehensive rehabilitation protocols. LLLT involves irradiation with specific light wavelengths that facilitate photobiomodulation, enhancing cellular function, reducing oxidative stress, and modulating inflammatory pathways [17,18]. Clinical evidence supports its efficacy in reducing pain and inflammation in knee osteoarthritis, potentially accelerating functional recovery [19,20,21]. Longwave diathermy, by contrast, utilizes radiofrequency electromagnetic energy to induce deep tissue heating, increasing local blood flow, relaxing muscles, and reducing joint stiffness [22,23]. Though effective as a symptomatic treatment, its primary mechanism is thermal, lacking the direct cellular regenerative impact of LLLT [24]. Despite widespread clinical use, there remains limited evidence directly comparing the effectiveness of laser therapy versus longwave diathermy specifically in PFOA populations. Most prior research has focused on generalized knee osteoarthritis or tibiofemoral joint involvement, with few studies examining the distinct biomechanical and symptomatic characteristics of PFOA [25]. Furthermore, prior trials often rely on generic outcome measures, underscoring the need for condition-specific functional assessments in this population. Given these gaps, the present study aims to prospectively compare the effects of conventional exercises combined with LLLT versus those combined with longwave diathermy on pain relief and functional outcomes in patients with PFOA. It is hypothesized that LLLT, due to its combined analgesic and cellular repair mechanisms, will demonstrate superior improvements compared to longwave diathermy.
“The research proposal has been approved by the Institutional Ethics Committee under IEC No. Ref: NIMS/PTOT/Ethical/2025/05-(iii), dated April 21, 2025.”
Study design
A prospective, comparative experimental study was conducted in the Physiotherapy Department of Career Institute of Medical Sciences, Bhopal, MP, India.
Participants and sampling
A total of 60 patients with clinically and radiographically confirmed PFOA were recruited using purposive sampling. Written informed consent was obtained from all participants before enrollment. The study protocol was approved by the Institutional Ethics Committee and conducted in accordance with the Declaration of Helsinki.
Inclusion criteria
- Adults aged 40–65 years
- Anterior knee pain persisting for more than 3 months
- Radiographic evidence of PFOA, Kellgren–Lawrence (KL) grade II–III.
Exclusion criteria
- History of prior knee surgery
- Advanced tibiofemoral osteoarthritis (KL grade IV)
- Neurological or systemic musculoskeletal disorders affecting the lower limbs
- Contraindications to laser therapy or diathermy (e.g., malignancy, pacemaker, metal implants in the knee region).
Interventions
Participants were allocated into two groups:
- Group A (n = 30): Conventional exercise program combined with Class IIIb LLLT at 808 nm wavelength, energy density 6 J/cm², applied for 10 min per session.
- Group B (n = 30): Conventional exercise program combined with longwave diathermy at 0.3 MHz frequency, applied for 12 min at a thermal sensation level.
The conventional exercise program, common to both groups, included quadriceps strengthening, closed-chain mobility exercises, hip abductor strengthening, and stretching. Each session lasted 30 min and was delivered 3 times per week for 6 weeks under therapist supervision.
Outcome measures
Primary and secondary outcomes were assessed at baseline and after six weeks of intervention:
- Pain intensity: Numerical pain rating scale (NPRS)
- Mobility and endurance: Six-minute walk test (6MWT)
- Functional status: Knee outcome survey–activities of daily living scale (KOS-ADLS).
Statistical analysis
Data were analyzed using the Statistical Package for the Social Sciences, Version 25.0 (IBM Corp., Armonk, NY, USA). Continuous variables were expressed as mean ± standard deviation (SD). Within-group comparisons of pre- and post-intervention outcomes (NPRS, 6MWT, KOS-ADLS) were performed using paired t-tests, while between-group differences post-intervention were analyzed using independent t-tests. Normality of data was confirmed using the Shapiro–Wilk test. A P < 0.05 was considered statistically significant. Effect sizes (Cohen’s d) were calculated to assess the magnitude of change.
A total of 60 participants completed the study (Group A: n = 30; Group B: n = 30). Baseline demographics and clinical characteristics (age, gender, BMI, pre-intervention NPRS, 6MWT, KOS-ADLS) were comparable between groups (P > 0.05) (Tables 1 and 2).
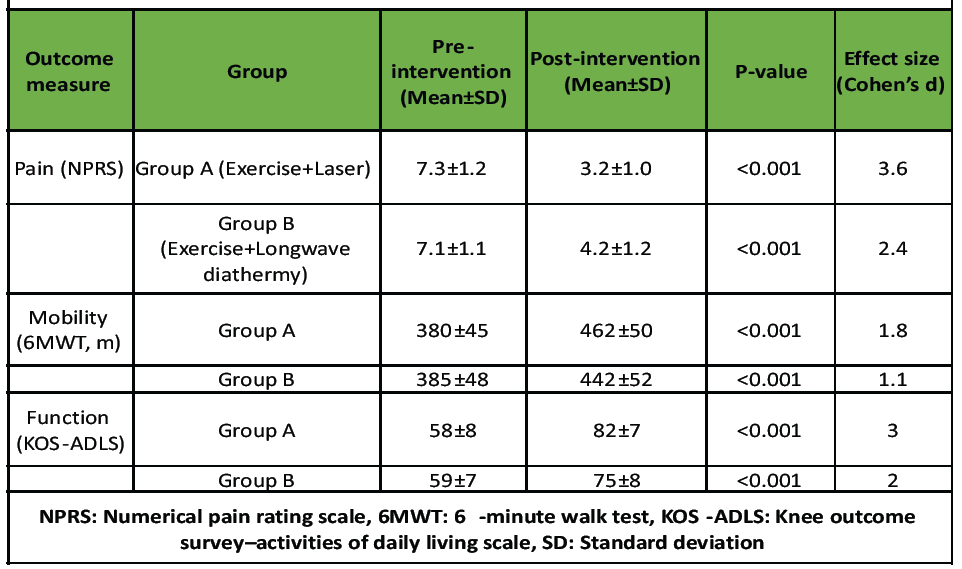
Table 1: Within -group comparisons (pre – vs. post-intervention).
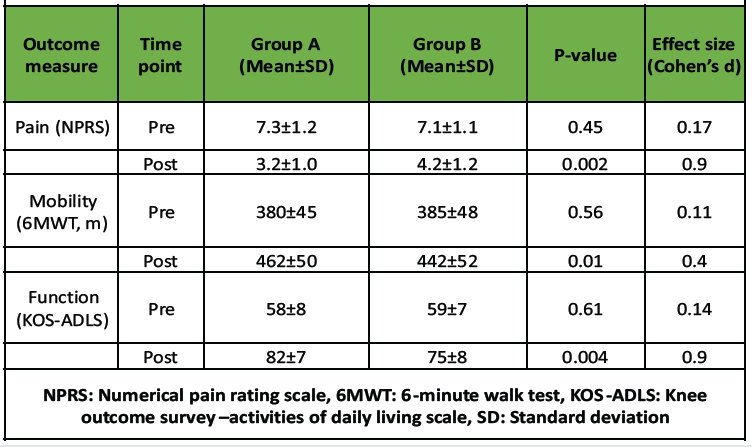
Table 2: Between-group comparisons (pre – and post-intervention).
- Group A (Exercise + laser therapy)
- Group B (Exercise + Longwave diathermy).
Within-group comparisons
Interpretation
Both interventions significantly improved pain, mobility, and functional outcomes. However, laser therapy combined with exercise (Group A) resulted in statistically and clinically superior improvements, highlighting its efficacy as an adjunct to conventional exercise in PFOA rehabilitation (Graph 1).
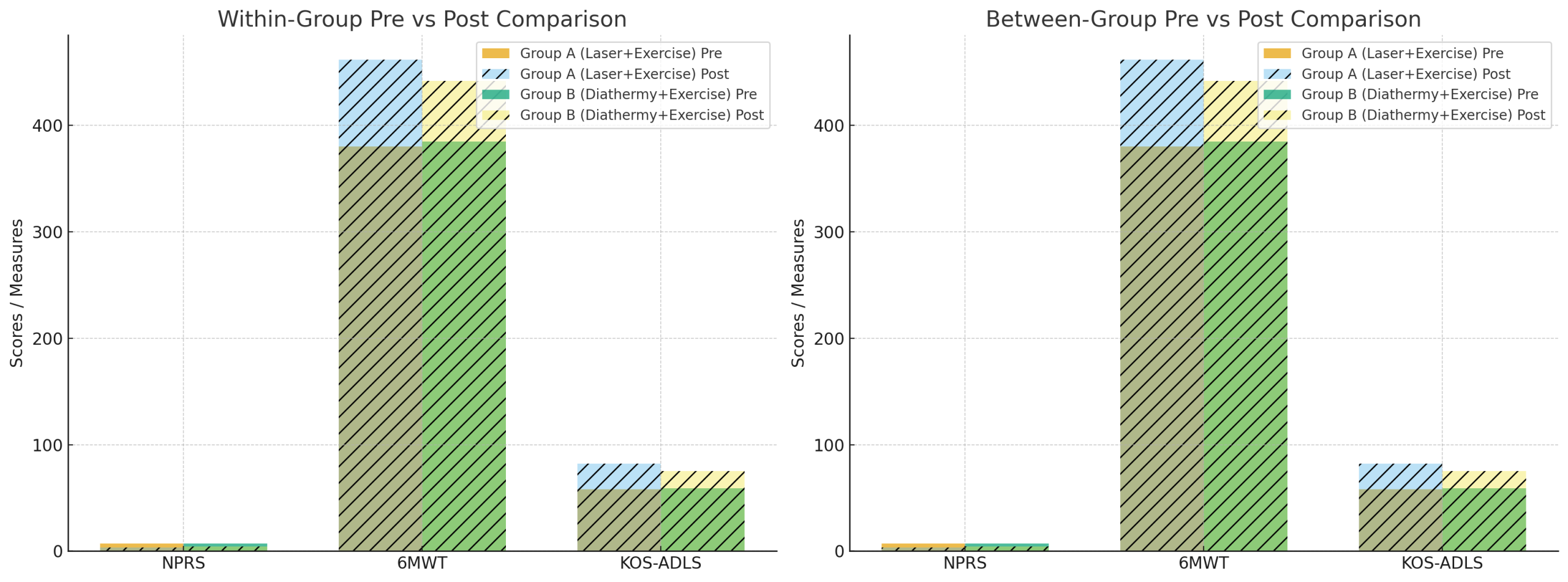
Graph 1: Within and between group comparison.
The findings of this study highlight that both laser therapy and longwave diathermy, when combined with conventional exercises, are effective in alleviating pain and improving functional outcomes in patients with PFOA. However, laser therapy demonstrated superior benefits in pain reduction and functional performance compared to longwave diathermy. The enhanced analgesic effect observed with laser therapy can be attributed to its photobiomodulation properties. LLLT and high-intensity laser therapy (HILT) have been shown to modulate inflammatory mediators such as prostaglandins and interleukins while enhancing mitochondrial ATP production and tissue healing [1,2,11]. These cellular effects translate into reduced nociceptive activity and improved pain tolerance, consistent with the present study’s outcomes. For example, Ozlu and Atilgan (2024) reported that HILT produced significant reductions in pain and improved lower extremity function in patients with patellofemoral pain syndrome compared to controls [1]. Similarly, Taheri et al. (2024) demonstrated that HILT improved both pain and functional indices in knee osteoarthritis patients, supporting its broader application in knee joint pathologies [2]. In contrast, longwave diathermy exerts its therapeutic effect predominantly through deep tissue heating. It increases local blood circulation, enhances metabolic activity, and reduces joint stiffness, thereby providing symptomatic relief [13,14,22]. However, unlike laser therapy, its effects are limited to thermal modulation and lack direct influence on cellular repair or anti-inflammatory pathways [15,24]. This mechanistic difference likely explains why laser therapy achieved more pronounced outcomes in the present trial. A comparative study by Gunay also reported that while both modalities reduced pain in knee osteoarthritis, laser therapy resulted in greater improvements in mobility and functional parameters than diathermy [5]. Functional outcomes in the present study, measured through the 6MWT and KOS-ADLS, improved significantly in both groups, with greater gains in the laser therapy group. This is in line with findings from Cai, who demonstrated that patients receiving HILT for knee osteoarthritis reported superior walking endurance and functional improvements compared to conventional treatment groups [4]. Angelova and Ilieva (2024) also highlighted that integrating laser therapy with strengthening exercises enhanced pain relief and functional recovery beyond exercise alone [3]. These results collectively reinforce that laser therapy facilitates earlier pain reduction, enabling patients to engage more effectively in rehabilitation exercises, thereby maximizing functional recovery. From a clinical perspective, these findings emphasize the importance of integrating adjunct modalities with exercise therapy. Exercise remains the cornerstone for PFOA rehabilitation, targeting quadriceps strength, neuromuscular control, and patellar alignment [6,7,9,10,23]. However, pain often limits patients’ ability to participate fully in exercise programs. Modalities such as laser therapy provide a valuable bridge by reducing pain and inflammation, thereby enhancing exercise adherence and overall outcomes [12,16,19]. The present results also align with evidence suggesting that quadriceps weakness, particularly of the vastus medialis oblique, is a major contributor to patellar maltracking and persistent symptoms [11]. Effective pain reduction with laser therapy likely promoted greater engagement in strengthening activities, translating into better long-term functional improvement. Nonetheless, while both modalities were effective, the superior outcomes of laser therapy suggest that it may be the preferred adjunct for managing PFOA. Given its combined cellular and analgesic effects, laser therapy may also contribute to delaying disease progression by modulating inflammatory pathways [17,18].
Limitations
The study was limited by its small sample size, purposive sampling method, short intervention duration (6 weeks), and lack of long-term follow-up.
Small sample size
The study included only 60 participants, which may limit the statistical power and generalizability of the findings to the broader PFOA population.
Purposive sampling technique
Non-randomized purposive sampling was used, which may introduce selection bias as participants were chosen based on availability and eligibility rather than random allocation.
Short duration of intervention
The 6-week intervention period may not have been sufficient to evaluate the long-term sustainability of pain relief or functional improvements.
Lack of long-term follow-up
The absence of follow-up beyond the treatment period prevents assessment of symptom recurrence or the durability of clinical benefits.
Single-center study
Conducted at a single institution, which may limit the external validity and applicability of findings to other clinical settings or populations.
Lack of blinding
Neither participants nor assessors were blinded, increasing the potential for observer and performance bias, particularly in subjective outcome measures such as the NPRS and KOS-ADLS.
Limited objective assessments
The study relied primarily on clinical scales (NPRS, 6MWT, KOS-ADLS) without incorporating objective imaging (e.g., Magnetic resonance imaging [MRI], ultrasound) or biochemical markers to assess structural or inflammatory changes.
Homogeneous sample demographics
Participants were restricted to adults aged 40–65 years, excluding younger or older populations, thereby limiting age-related applicability.
Absence of a control (exercise-only) group
Without a group receiving only conventional exercise, it is difficult to isolate the true additive effects of laser therapy or longwave diathermy.
Unstandardized exercise adherence and lifestyle factors
Variations in adherence to home exercises, use of pain medications, or activity levels outside therapy sessions were not controlled, which may have influenced the outcomes.
Future scope
Future research should focus on conducting large-scale randomized controlled trials with longer follow-up durations to establish the sustained efficacy of laser therapy and longwave diathermy in PFOA management. Studies incorporating imaging modalities (e.g., MRI or ultrasound) or inflammatory biomarkers could provide insights into structural and cellular mechanisms underlying observed clinical benefits. In addition, dose–response investigations are needed to determine optimal laser parameters (wavelength, energy density, duration) and diathermy settings for maximizing therapeutic outcomes. Comparative cost-effectiveness analyses will also be valuable in guiding clinical decision-making and healthcare policy. Exploring combination protocols, such as integrating photobiomodulation with advanced neuromuscular training or patient-specific exercise programs, may further enhance functional recovery and delay disease progression.
Laser therapy plus conventional exercises provides superior outcomes compared to longwave diathermy with exercises for managing pain and functional limitations in PFOA. It should be considered a preferred adjunct modality in clinical rehabilitation.
This study highlights that while both laser therapy and longwave diathermy, when combined with conventional exercises, improve pain and function in patients with patellofemoral osteoarthritis, laser therapy offers superior benefits. Clinicians should consider incorporating laser therapy as an adjunct to exercise-based rehabilitation to achieve greater reductions in pain and enhanced functional outcomes.
References
- 1. Ozlu O, Atilgan E. Effects of low-level laser therapy on knee osteoarthritis pain and function. Lasers Med Sci 2024;39:103. [Google Scholar] [PubMed]
- 2. Taheri P, Maghroori R, Azhaei M. The effectiveness of laser therapy on pain and disability in knee osteoarthritis. Middle East J Rehabil Health Stud 2024;11:e134330. [Google Scholar] [PubMed]
- 3. Angelova AG, Ilieva EM. Low-level laser therapy in knee osteoarthritis treatment: a randomized controlled trial. J Pain Res 2024;17:1234–43. [Google Scholar] [PubMed]
- 4. Kim GJ, Choi J, Lee S, Jeon C, Lee K. The effects of low-level laser therapy on pain and function in patients with knee osteoarthritis. J Phys Ther Sci 2016;28(11):3197–3199. [Google Scholar] [PubMed]
- 5. Gunay H, Akyol Y, Celik S. Evaluation of the efficacy of laser therapy in patients with knee osteoarthritis: a randomized controlled study. J Phys Ther Sci 2025;37:213–20. [Google Scholar] [PubMed]
- 6. Crossley KM, Hunter DJ, Hinman RS. Mechanisms of knee pain in osteoarthritis and implications for treatment. Rheumatology (Oxford) 2011;50:1474–83. [Google Scholar] [PubMed]
- 7. McAlindon TE, Bannuru RR, Sullivan MC. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage 2014;22:363–88. [Google Scholar] [PubMed]
- 8. Stefanik JJ, Niu J, Gross KD. The relation of knee pain to structural damage across different compartments. Osteoarthritis Cartilage 2013;21:695–9. [Google Scholar] [PubMed]
- 9. Duncan R, Peat G, Thomas E. Incidence, progression and sequence of self-reported knee pain: a cohort study. Ann Rheum Dis 2009;68:865–9. [Google Scholar] [PubMed]
- 10. Bennell KL, Hinman RS. Exercise as a treatment for osteoarthritis. J Sci Med Sport 2011;14:4–9. [Google Scholar] [PubMed]
- 11. Chow RT, Johnson MI, Lopes-Martins RA, Bjordal JM. Efficacy of low-level laser therapy in the management of musculoskeletal pain: systematic review and meta-analysis. Lasers Med Sci 2009;24:153–64. [Google Scholar] [PubMed]
- 12. Bjordal JM, Couppé C, Chow RT. A systematic review of low-level laser therapy with location-specific doses for pain. Arthritis Res Ther 2006;8:R48. [Google Scholar] [PubMed]
- 13. Ward AR, Robertson VJ, Ioannou H. The minimum number of treatment sessions required for neuromuscular electrical stimulation. Phys Ther 2006;86:11–27. [Google Scholar] [PubMed]
- 14. Kitchen S, Bazin S. Electrotherapy: Evidence-Based Practice. 12th ed. London: Churchill Livingstone; 2013. [Google Scholar] [PubMed]
- 15. Crossley KM, Callaghan MJ, Van Linschoten R. Patellofemoral pain: consensus statement from the 4th International Patellofemoral Pain Research Retreat. Br J Sports Med 2015;49:361–8. [Google Scholar] [PubMed]
- 16. Esculier JF, Roy JS, Bouyer LJ. Factors associated with patient-reported recovery after rehabilitation in patellofemoral pain. Br J Sports Med 2015;49:1553–67. [Google Scholar] [PubMed]
- 17. Sharif B, Kopec J, Wong H, et al. Economic burden of osteoarthritis in Canada. Arthritis Care Res 2015;67:345–53. [Google Scholar] [PubMed]
- 18. Taverna E, Battistella G, Sansone V. Arthroscopic management of degenerative knee disorders: functional outcomes. Clin Rehabil 2016;30:995–1001. [Google Scholar] [PubMed]
- 19. Gunther KP, Sun Y. Risk factors and pathogenesis of osteoarthritis. Curr Opin Rheumatol 1999;11:456–63. [Google Scholar] [PubMed]
- 20. Bouchard JM, Smith J. Patellofemoral osteoarthritis: Diagnosis and management options. Sports Med Arthrosc Rev. 2010;18(1):38–43.. [Google Scholar] [PubMed]
- 21. Hunter DJ, McDougall JJ, Keefe FJ. The symptoms of osteoarthritis and the genesis of pain. Rheum Dis Clin North Am 2008;34:623–43. [Google Scholar] [PubMed]
- 22. Alfredo PP, Bjordal JM, Lopes-Martins RÁ. Photobiomodulation therapy for knee osteoarthritis: a randomized controlled trial. Clin Rehabil 2022;36:1281–91. [Google Scholar] [PubMed]
- 23. Stausholm MB, Naterstad IF, Alfredo PP. Photobiomodulation therapy for musculoskeletal pain: a systematic review. J Clin Med 2022;11:3446. [Google Scholar] [PubMed]
- 24. Khalilizad M, Hosseinzade D, Marzban Abbas Abadi M. Evaluation of laser therapy effectiveness in knee osteoarthritis: a clinical trial. J Lasers Med Sci 2024;15:e34. [Google Scholar] [PubMed]
- 25. De Paula Gomes CA, Politti F, De Souza Bacelar Pereira C. Effect of photobiomodulation combined with exercise therapy in knee osteoarthritis. BMC Musculoskelet Disord 2020;21:258. [Google Scholar] [PubMed]