Vascularized fibula graft augmented fixation is an effective technique in managing complex periprosthetic fractures of the humerus in the elderly osteoporotic population.
Dr. Anand Kumaroth Somasundaram, Senior Consultant, Department of Orthopaedics, Caritas Hospital and Institute of Health Sciences, Kottayam, Kerala, India. E-mail: anandsvkas@gmail.com
Introduction: Periprosthetic humeral fractures are rare but serious complications following shoulder arthroplasty, especially in elderly patients with osteoporosis. These fractures pose a significant management challenge due to compromised bone quality and the presence of prosthetic components. Salvage procedures such as vascularized fibular grafting offer a biologically and mechanically favorable option in complex cases with failed internal fixation.
Case Report: We present the case of an 80-year-old female with systemic hypertension and osteoporosis, who sustained a periprosthetic fracture of the right humerus, which was categorized under the Wright and Cofield classification as Type B. She was initially treated with internal fixation of the fracture, and 3 weeks later, presented with implant failure following a trivial trauma. After initial stabilization and medical optimization, she underwent open reduction and internal fixation of the right humerus with vascularized fibular grafting harvested from the opposite leg. Medical management of osteoporosis was also initiated in the post-operative period. At 3 months follow-up, she had clinical and radiological healing of the fracture, restoration of full shoulder range of motion, and activities of daily living. This case highlights the complexity of managing periprosthetic humeral fractures in osteoporotic patients. Standard fixation techniques are often inadequate due to poor bone stock and fraught with high failure rates. Vascularized fibular grafting, though more commonly used in long bone non-unions, can provide durable fixation and enhance osteogenesis in selected cases.
Conclusion: Vascularized fibular grafting is an effective option in managing failed fixation of periprosthetic fractures in severely osteoporotic patients. A multidisciplinary approach and individualized surgical planning are crucial for optimal outcomes.
Keywords: Periprosthetic fracture, vascularized fibular graft, Osteoporosis.
An uncommon complication of all types of arthroplasties is a periprosthetic fracture [1,2]. Although they are less frequent in shoulder arthroplasties, they nonetheless provide a challenge in patient care. Total shoulder arthroplasty (TSA) and reverse TSA (RTSA) have become mainstay treatment options for various shoulder pathologies, including osteoarthritis, rotator cuff arthropathy, massive rotator cuff tear, and certain proximal humeral fractures [3,4]. Periprosthetic fractures develop in relation to prosthetic implants, usually in the TSA components. The incidence of periprosthetic fracture is reported as 0.6–3% of patients with TSA [5]. TSA and reverse shoulder arthroplasty (RSA) have revolutionized the treatment of complex shoulder pathologies, including osteoarthritis, massive rotator cuff tears, and proximal humerus fractures [6,7]. RSA, in particular, is often chosen for rotator cuff-deficient shoulders. However, in elderly patients with poor bone quality, RSA may be associated with increased risk of complications such as early loosening, scapular notching, instability, or infection [7,8,9]. Although post-operative periprosthetic humeral fractures are rare, they are becoming more common as the population ages and these procedures become more common . The most common location of the fracture is the humerus. Periprosthetic humeral fractures most often occur intraoperativokely but can also develop postoperatively, especially in osteoporotic bone. The Wright and Cofield classification is commonly used to categorize these fractures based on the location in relation to the humeral stem. Hamada classification further guides the assessment of fixation failures in the presence of prosthetic components [10]. Periprosthetic fractures often present surgeons with difficult management decisions and, in cases of surgical management, technical challenges. The reported incidence of periprosthetic humeral fractures following shoulder arthroplasty varies greatly (1.2–19.4%) [5-8]. Management options vary from conservative treatment to revision arthroplasty or surgical fixation [6]. options such as vascularized fibular grafts traditionally used in long bone non-unions may offer superior mechanical stability and biological integration.
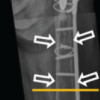
An 80-year-old female patient with a known history of systemic hypertension and severe osteoporosis presented to the emergency room (ER) with a history of a fall and was diagnosed to have a periprosthetic fracture of the right humerus (Figure 1) and an extrarticular fracture of the left distal radius.
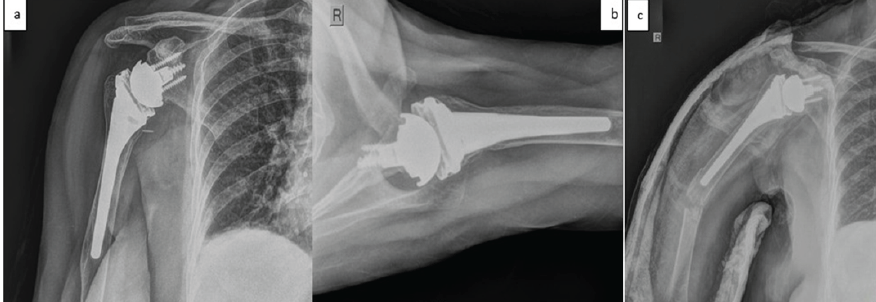
Figure 1: Anteroposterior and lateral radiographs showing well-functioning reverse total shoulder arthroplasty [R] and well-fixed uncemented prosthesis with severe osteopenia (a and b). Anteroposterior radiograph showing periprosthetic fracture, Wright and Cofield classification Type B with stable prosthesis (c).
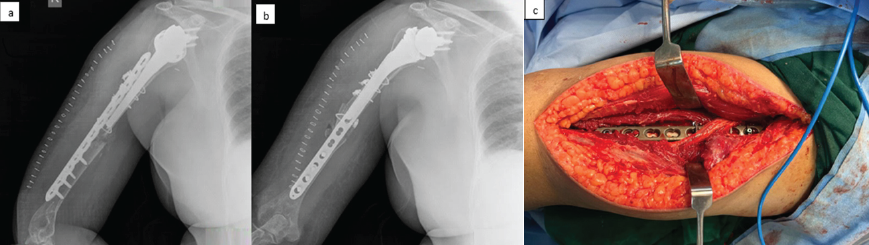
Figure 2: Anteroposterior and lateral radiographs showing well-fixed periprosthetic fracture utilizing 4.5 mm locking compression plates and cable system with cortico-cancellous bone graft interposed at fracture site (a and b). Clinical image taken during surgery showing periprosthetic fracture fixation with isolated intact radial nerve via posterior approach (c).
A standard open reduction and internal fixation was utilized to treat the contralateral distal radius fracture. Three weeks later patient presented with a history of a trivial trauma (twisting injury while applying an arm sling) and, on evaluation, was diagnosed to have a displaced fracture with a failed implant (Figure 3a,b).
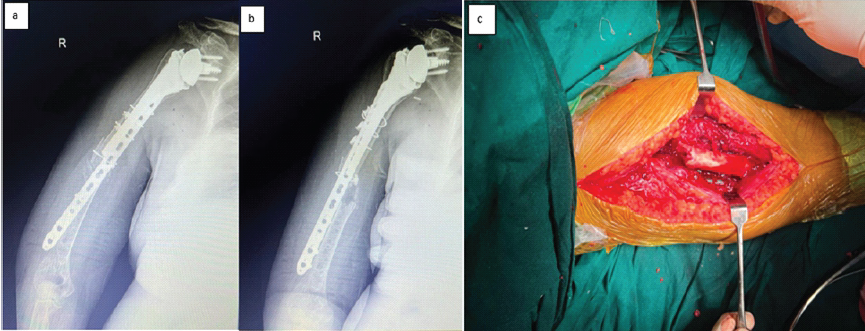
Figure 3: Anteroposterior and lateral radiographs showing failed osteosynthesis of the periprosthetic fracture with pulled-out implant from the distal fragment and displaced fracture (a and b). Intra-operative clinical photograph showing failed osteosynthesis of the periprosthetic fracture with pulled out implant via an extended anterolateral approach (c).
The patient was admitted for further evaluation and surgical management. Upon clinical examination at the time of admission, the patient was alert, oriented, and afebrile, with stable vital signs. Local examination of the right upper limb revealed tenderness and a well-healed surgical scar with radiographic evidence of periprosthetic fracture and implant failure. Given the complexity of the case, she was initially managed with immobilization using splintage, along with standard analgesics and supportive medical care. After thorough preoperative counseling, including expected outcomes and the importance of post-operative physiotherapy and follow-up, informed consent was obtained from the patient and her family. A combined orthopedic and vascular surgical procedure was planned.
Surgical technique
The patient was positioned supine with a side arm table. An extended anterolateral approach combined with a medial incision for additional exposure of the brachial vasculature was chosen after discussion with the vascular surgeon so as to enable safe and effective vascular anastomosis between the brachial vessels and the peroneal vessels of the graft. The implant (locking compression plate [LCP] 4.5 mm) was found to be completely backed out (Figure 3 c) from the distal fragment with stripping of all four locking screws. The radial nerve was completely isolated from the plate, protected, and a safe exit of the entire implant was carried out. A 10 cm segment of fibula with an associated vascular pedicle was selected, shaped appropriately, and interposed in the gap between reduced proximal and distal fragments in such a way that good contact is made between the host bone and the graft. The remaining portion of the fibula was split longitudinally and used on either side of the construct to augment the fixation. Finally, a 4.5 mm LCP was used along with an encirclage wire system to complete the procedure. The case was handed over to the vascular surgeon to complete the microvascular anastomosis. Good blood flow in the graft was observed post-anastomosis. Fluoroscopy images showed near anatomical reduction of the fracture with a well-placed fibula graft (Figure 4a, b) with excellent contact all over.
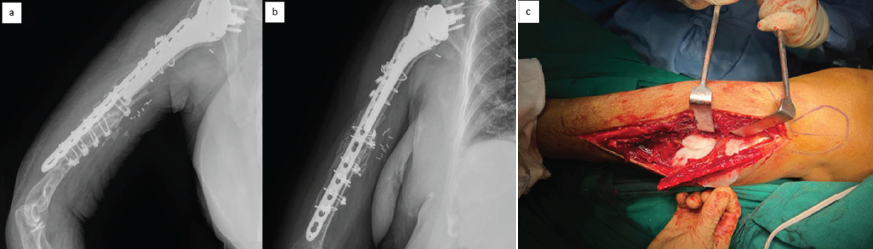
Figure 4: Anteroposterior and lateral radiographs at 3 months showing well-healed internal fixation of periprosthetic fracture with implants in situ, showing well-taken vascularized fibula graft (a and b). Intra-operative clinical image showing harvest of vascularized fibula graft from [L] leg (c) (Figure 4C).
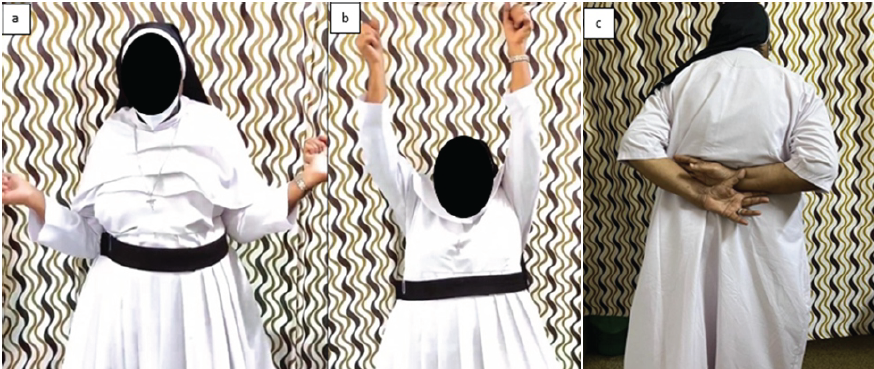
Figure 5: Clinical images of the patient at 3 months from surgery showing a good range of movements and return to activities of daily living (a, b, c).
Post-operative periprosthetic humeral fractures are much rarer than intra-operative fractures. Similar to how the Vancouver method is applied to the classification of periprosthetic proximal femoral fractures, the fractures can be categorized according to their anatomy and implant stability. The categorization is somewhat different from the intra-operative periprosthetic fracture classification. The tuberosities are the site of type A post-operative periprosthetic humeral fractures. Fractures of type B happen at the stem. Subtypes B1 spiral fractures with a stable implant, B2 short oblique fractures at the tip of the stem with a stable implant, and B3 fractures around the stem with an unstable implant are the three categories into which these can be divided. Type C fractures happen far from the stem’s tip [10]. Our case demonstrates the distinctive function of vascularized fibular grafting as a rescue technique in an elderly osteoporotic patient experiencing fixation failure after a periprosthetic fracture following RTSA. The choice to use a vascularized fibular graft was influenced by the patient’s compromised bone quality and the previous construct’s mechanical instability, highlighting the increasing agreement in the literature supporting biological enhancement in complicated revisions. Studies have indicated that non-vascularized bone grafts frequently fail in patients with osteoporosis because of inadequate integration and insufficient blood supply, especially in revision situations. On the other hand, vascularized fibular grafts offer strong structural support and osteogenic ability with proven efficacy in long bone non-unions, especially in cases of failed fixation or infection [2-8]. Our case reflects these findings, highlighting its usefulness in periprosthetic fractures where internal fixation by itself is inadequate. The failure of fracture fixation in the context of RSA has been insufficiently reported. Another study highlighted that RTSA, although beneficial for rotator cuff arthropathy, tends to experience complications in osteoporotic individuals, particularly when facing further trauma [8-10]. Our case adds support to this, as the initial fixation did not succeed even with correct surgical technique, indicating that mechanical devices by themselves might be inadequate in hosts with severe osteoporosis. With the increasing rates of shoulder arthroplasty in the older population, upcoming research needs to emphasize prospective assessment of vascularized grafting techniques in upper limb periprosthetic fractures to create standardized guidelines and to enhance the surgical criteria. Alternative approaches, such as vascularized bone grafts, ought to be included in the surgical toolkit for specific situations.
This case highlights the challenges of managing periprosthetic fractures in osteoporotic patients with a history of multiple orthopedic interventions. The multidisciplinary approach, timely surgical intervention, and structured post-operative care, including physiotherapy and medication, were critical in ensuring a stable recovery.
In elderly osteoporotic patients with complex periprosthetic humeral fractures and failed prior fixation, a vascularized fibular graft provides both biological and mechanical superiority. This technique offers a viable salvage option, promoting rapid union and restoring function where conventional methods are prone to failure. A successful outcome hinges on a multidisciplinary surgical approach and aggressive postoperative medical and rehabilitative management.
References
- 1. McGraw P, Kumar A. Periprosthetic fractures of the femur after total knee arthroplasty. J Orthop Traumatol 2010;11:135-41. [Google Scholar] [PubMed]
- 2. Luzzi A, Lakra A, Murtaugh T, Shah RP, Cooper HJ, Geller JA. The effect of periprosthetic fractures following total hip and knee arthroplasty on long-term functional outcomes and quality of life. Arthroplast Today 2024;29:101418. [Google Scholar] [PubMed]
- 3. Ellman H. Diagnosis and treatment of incomplete rotator cuff tears. Clin Orthop Relat Res 1990;254:64-74. [Google Scholar] [PubMed]
- 4. Clifford AL, Hurley E, Anakwenze O, Klifto CS. Rotator cuff arthropathy: A comprehensive review. J Hand Surg Glob Online 2024;6:458-62. [Google Scholar] [PubMed]
- 5. Shoulder Periprosthetic Fracture-Shoulder and Elbow-Orthobullets. Available from: https://www.orthobullets.com/shoulder-and-elbow/422742/shoulder-periprosthetic-fracture [Last accessed on 2025 May 26]. [Google Scholar] [PubMed]
- 6. Frank JK, Siegert P, Plachel F, Heuberer PR, Huber S, Schanda JE. The evolution of reverse total shoulder arthroplasty-from the first steps to novel implant designs and surgical techniques. J Clin Med 2022;11:1512. [Google Scholar] [PubMed]
- 7. Kelly BJ, Myeroff CM. Reverse shoulder arthroplasty for proximal humerus fracture. Curr Rev Musculoskelet Med 2020;13:186-99. [Google Scholar] [PubMed]
- 8. Shah SS, Gaal BT, Roche AM, Namdari S, Grawe BM, Lawler M, et al. The modern reverse shoulder arthroplasty and an updated systematic review for each complication: Part I. JSES Int 2020;4:929-43. [Google Scholar] [PubMed]
- 9. Nabergoj M, Denard PJ, Collin P, Trebše R, Lädermann A. Mechanical complications and fractures after reverse shoulder arthroplasty related to different design types and their rates: Part I. EFORT Open Rev 2021;6:1097-108. [Google Scholar] [PubMed]
- 10. Khan WS, Longo UG, Ahrens PM, Denaro V, Maffulli N. A systematic review of the reverse shoulder replacement in rotator cuff arthropathy, rotator cuff tears, and rheumatoid arthritis. Sports Med Arthrosc Rev 2011;19:366-79. [Google Scholar] [PubMed]