Arthroscopic fixation provides excellent visualization of the joint, helps achieve anatomical reduction, and allows simultaneous management of ligament and meniscal injuries. Poliotic limbs present unique anatomical and biomechanical challenges; however, with proper technique and adaptation, good functional outcomes are possible.
Dr. Rahul Kakran, Department of Orthopaedics, Yashoda Group of Hospitals, Nehru Nagar and Vasundhra, Ghaziabad, Uttar Pradesh, India. E-mail: rahul.kakran@yahoo.com
Introduction: Medial Hoffa fractures are exceptionally rare, especially when associated with intra-articular knee injuries (anterior cruciate ligament, medial collateral ligament, and meniscus tears). The discussed case highlights a single-stage fully arthroscopic fixation of a medial Hoffa fracture with associated ligament and meniscal injuries – representing a novel and effective, though challenging, treatment option. This is the first report of this kind in the literature.
Case Report: A 42-year-old male patient presented 5 days after an injury to the left knee after a slip and fall in the bathroom. The knee was swollen, unstable, and painful, and the patient was a known case of left poliotic lower limb.
Conclusion: This case represents the first documented instance of a fully arthroscopic fixation of a medial Hoffa fracture with simultaneous ligament and meniscal repair in a poliotic patient.
Keywords: Hoffa’s fracture, arthroscopic, polio.
Coronal plane fractures of the distal femoral condyle are labeled as Hoffa fractures. Albert Hoffa gave an initial account of these fractures in 1904. The distal fragment, owing to no muscle attachment, acts as a freely lying, large, intra-articular bone piece. This fragment is bathed in a pool of synovial fluid and is commonly a cause of non-union in conservatively managed and neglected fractures. Other complications include knee joint osteoarthritis and knee stiffness. Hence, early anatomical reduction and internal fixation remains the treatment of choice.
Arthroscopy-assisted reduction and internal fixation (ARIF) of these fractures is a novel technique with a minimally invasive procedure. This avoids large soft-tissue disruption and helps in early recovery with less morbidity. We hereby present a case of medial condyle Hoffa fracture, which was managed by ARIF.
Although these fractures usually occur in isolation, they may rarely combine with ligamentous or meniscal injuries, forming complex orthogonal injuries. Their rarity makes treatment challenging, especially in poliotic patients, where altered anatomy, bone strength, and soft tissues add further difficulty for the surgeon.
We present a review of the current literature and salient points for surgeons to learn this technique.
A 42-year-old male patient came to us 5 days after an injury to the left knee after a slip and fall in the bathroom. The knee was swollen, unstable, and painful.
The patient was a known case of left poliotic lower limb and could carry out his daily activity without any assistance (kalipers/hand on knee gait).
According to the patient, he was able to walk (pre-injury) almost normally with his ankle in equinus.
Radiographs (Fig. 1) and computed tomography scan (Fig. 2) of the knee revealed an undisplaced Hoffa fracture of the medial femoral condyle.

Figure 1: Pre-operative X-rays of the left knee showing an undisplaced medial femoral condyle Hoffa’s fracture.
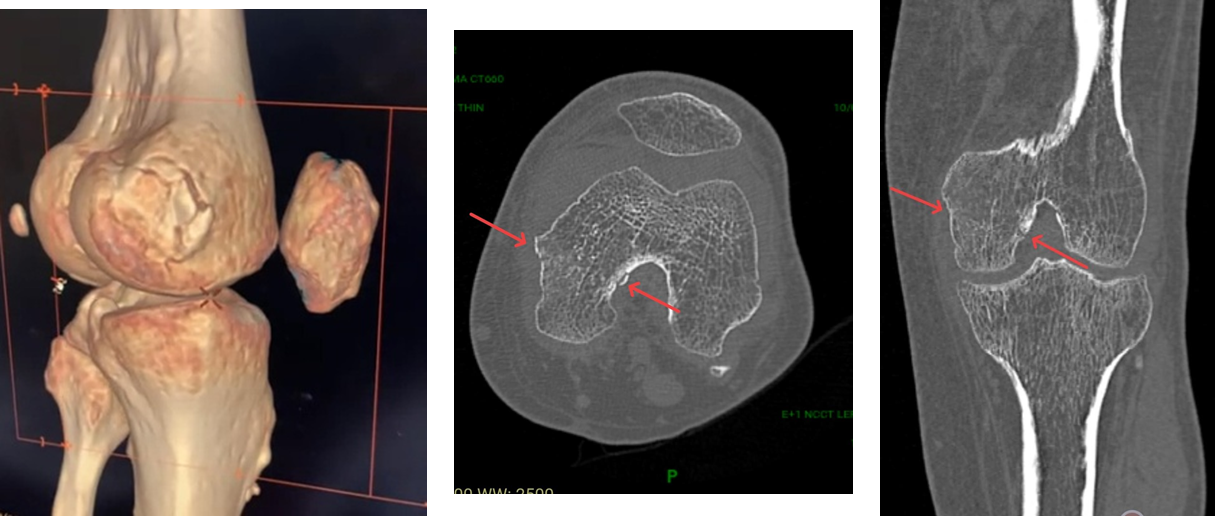
Figure 2: Non-contrast computed tomography scan left knee.
Magnetic resonance imaging (MRI) scan of the knee (Figs. 3 and 4) revealed a complete tear of the anterior cruciate ligament (ACL), the medial collateral ligament (MCL), and a tear of the anterior horn and part of the body of the lateral meniscus.
Henceforth, after due informed consent, the patient was planned for ARIF.
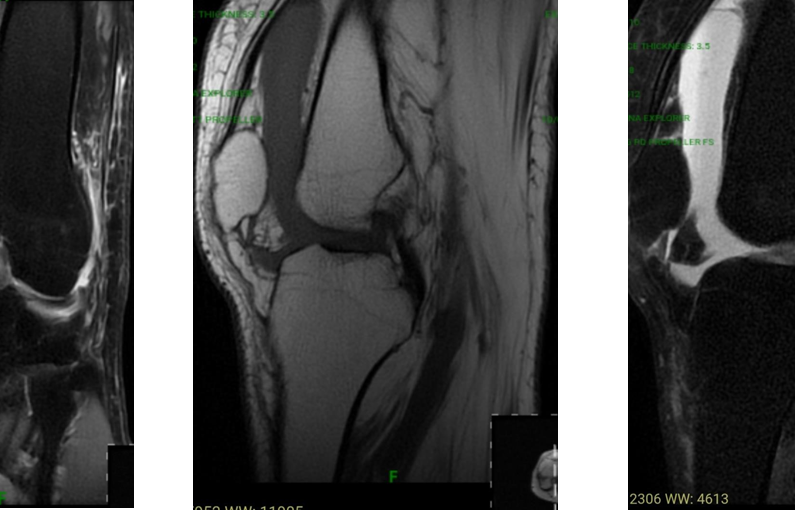
Figure 3: Magnetic resonance imaging scan left knee (showing Complete tear of ACL and MCL).
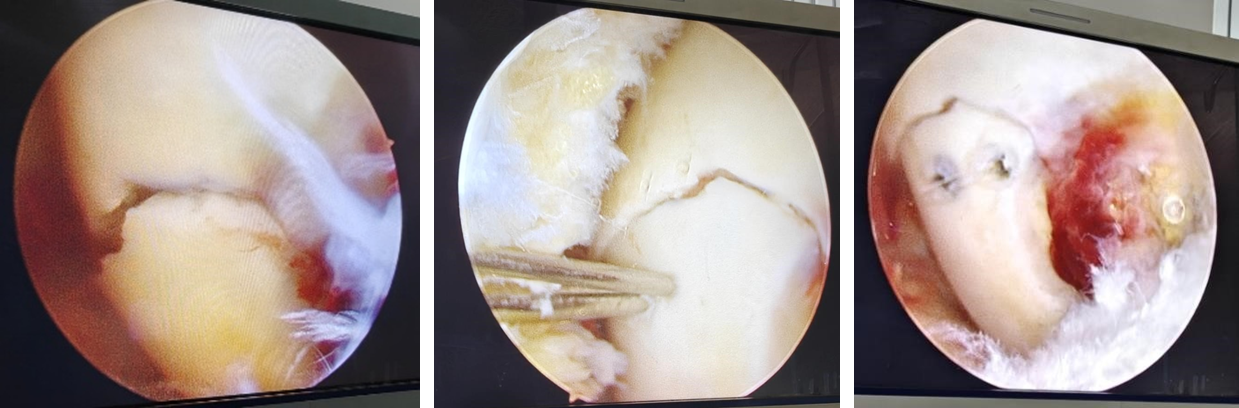
Figure 4: Intraoperative arthroscopic image showing medial Hoffa’s fracture – before and after fixation images.
Non-contrast computed tomography (NCCT) and MRI left knee
The NCCT left knee (Fig. 2) was suggestive of an undisplaced fracture of the medial femoral condyle (Hoffa’s fracture).
MRI left knee (Figs. 3 and 5) was suggestive of a near-complete ACL tear, a Grade II tear of the anterior horn of the lateral meniscus, and a tear of the medial collateral ligament.
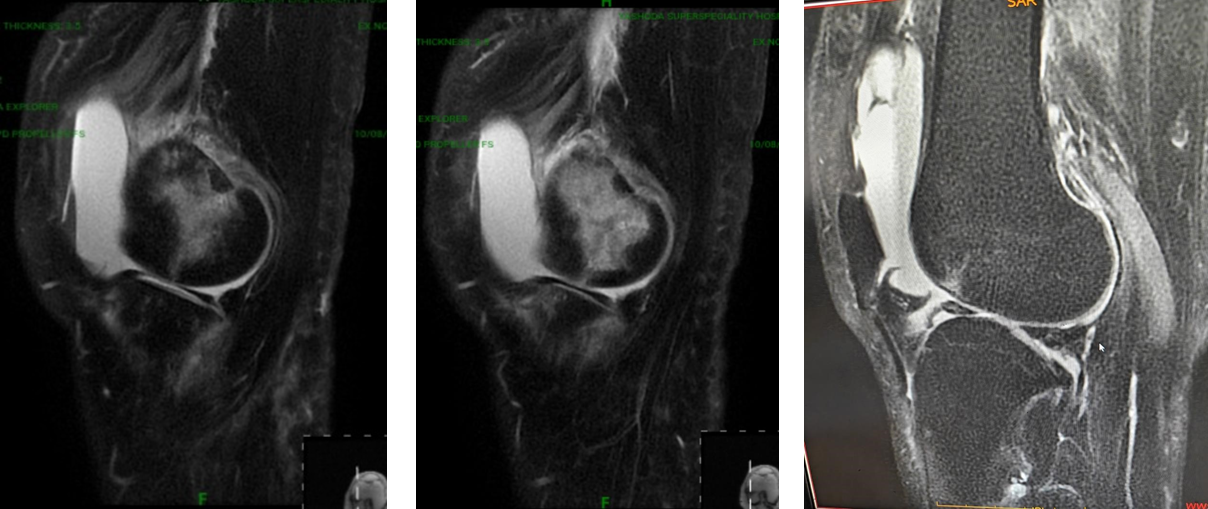
Figure 5: Magnetic resonance imaging scan left knee (Showing tear of anterior horn and part of body of lateral meniscus).
Procedure and findings
The patient was given spinal anesthesia and positioned supine with the leg on the table position. A tourniquet was applied to the upper thigh. Arthroscopy was performed through standard anteromedial and anterolateral portals. After washing off the hemarthrosis, diagnostic arthroscopy was initially performed.
A complete tear of the ACL and the anterior horn and part of the body of the lateral meniscus were found.
A large coronal fracture (undisplaced) was seen in the medial condyle (Fig. 4).
The fracture reduction was achieved with slight manipulation. Next, two guide wires were inserted just medial to the margin of the cartilage of the distal femur in an anteroposterior direction, perpendicular to the fracture site (Fig. 4).
The position and length of the guide wires were checked under Carm. Following this, anterior to posterior, two Herbert screws (AO Synthes) were inserted over the guide wires (Fig. 4).
The ACL graft was reconstructed using the opposite (healthy side) peroneus longus graft, which was fixed on the femoral side via an adjustable rigid loop and fixed on the tibial side via a Milagro advanced interference screw (Depuy).
The anterior horn and part of the body of the lateral meniscus were repaired using Prolene sutures (outside-in technique)
The torn MCL was repaired using anchor sutures. Intraoperative C-arm images were taken (Fig. 6).
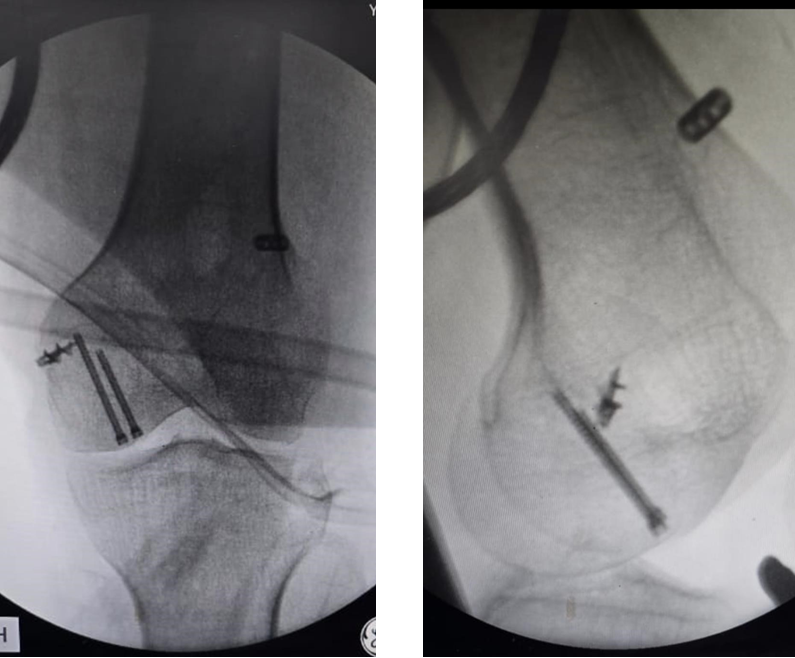
Figure 6: Intraoperative C-arm images.
Immediate post-operative clinical images of the patient and suture line are shown in Fig. 7.

Figure 7: Post-operative day 1 clinical images.
The patient was given a knee brace in the post-operative period for 2 weeks, following which knee range of motion (ROM) exercises were started on a hinged knee brace.
The Patient remained non-weight bearing for 6 weeks and then was allowed to bear weight partially for another 6 weeks.
Two months post-operative X-rays were suggestive of healing of the Hoffa’s fracture (Fig. 8).
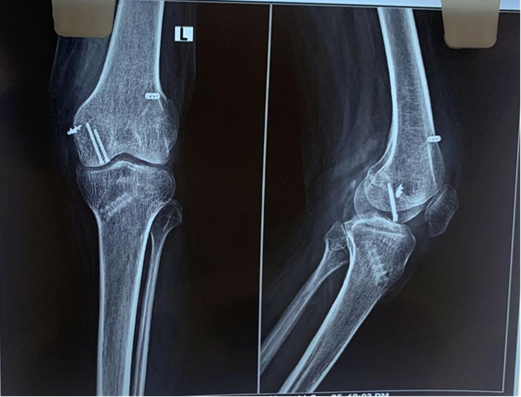
Figure 8: Two months post-operative X-rays.
At 4 months, the fracture was well united (Fig. 9) without any subsidence, so full weight bearing was allowed and the brace was discontinued.

Figure 9: Four months post-operative X-rays.
The patient had a ROM of 0–100 at the knee without any sign of infection (Fig. 10).

Figure 10: Four months post-operative clinical images.
Hoffa fractures are rare intra-articular coronal plane fractures of the distal femoral condyle, with lateral condyle involvement 3 times more common than medial (3:1) [1]. They may occur in isolation or in association with supracondylar intercondylar (AO/OTA 33C) femur fractures, emphasizing the importance of pre-operative CT scans to identify the coronal shear component that can be easily missed [2,3]. The exact mechanism of injury remains uncertain, though a shearing force on the posterior femoral condyle is most accepted.
Lewis et al.[4] proposed that axial loading of the lateral femoral condyle with the knee flexed beyond 90°, as seen in motorcycle accidents, results in such fractures. Physiological genu valgum predisposes the lateral condyle to injury. Hoffa fractures separate the patellofemoral from the tibiofemoral joint, making non-operative management unreliable due to high shear stress during movement.
Non-operative treatment yields poor results [5,6]. The treatment goal is anatomical reduction and rigid fixation for early mobilization and functional recovery [7,8,9,10]. Literature lacks a standardized fixation protocol or approach, and key orthopedic texts provide limited guidance [11,12].
Ostermann et al.[13] and Manfredini et al.[14] reported favorable long-term outcomes with rigid internal fixation, whereas non-operative cases had poor results.
Biomechanical studies indicate that 6.5-mm cancellous screws offer higher load-to-failure strength than 3.5-mm cortical screws [15]. Holmes et al.[16] recommended lag screws placed perpendicular to the fracture plane through a parapatellar approach to ensure anatomical reduction.
ARIF has been reported in a few cases [17,18,19,20,21]. Wallenbock and Ledinski [17] treated two Hoffa fractures arthroscopically with good early results, whereas McCarthy and Parker [18] noted advantages such as reduced soft-tissue dissection, blood loss, and operative time, despite limited compression. Ercin et al.[21] emphasized arthroscopy’s diagnostic and therapeutic role in identifying associated intra-articular injuries.
However, ARIF is technically demanding, and comminution or loose fragments from high-velocity trauma can complicate visualization. Small fragments may be excised, and larger ones fixed using Herbert screws. Surgeons should pre-consent patients for open reduction backup, and multidisciplinary planning (e.g., with plastic surgeons) may be necessary.
In conclusion, ARIF for Hoffa fractures, though challenging, offers significant advantages and is a promising minimally invasive option for well-selected patients. The presented case demonstrates a rare medial Hoffa fracture with associated ACL, MCL, and lateral meniscus injuries, successfully treated with a single-stage fully arthroscopic approach – the first of its kind reported.
The main mechanism of injury is high-energy direct impact or shear force to the posterior aspect of the femoral condyle for Hoffa’s fracture, hyperextension or pivoting injury for ACL tears, direct blow to the knee (valgus force) or twisting for MCL tears, and twisting injury for meniscus tears. Hence, this patient has a combination of all the mechanisms (valgus + rotation + shearing force), which makes this injury a severe and rare type of injury.
Together, this bony ligamentous injury makes it a complex orthogonal injury in a poliotic patient (never been documented in the world literature).
Medial Hoffa fractures are exceptionally rare, particularly when combined with ACL, MCL, and meniscal injuries. ARIF can be successfully used for such complex injuries, even in a poliotic limb, offering minimal soft-tissue trauma, faster recovery, and early rehabilitation.
This case represents the first documented instance of a fully arthroscopic fixation of a medial Hoffa fracture with simultaneous ligament and meniscal repair in a poliotic patient.
ARIF is a feasible and effective technique for managing complex intra-articular distal femoral fractures, including Hoffa fractures with associated soft-tissue injuries. Careful pre-operative planning, precise reduction, and arthroscopic expertise are essential for success. Even in challenging cases such as a poliotic limb with altered anatomy, satisfactory outcomes can be achieved with meticulous surgical execution and a staged rehabilitation protocol.
References
- 1. Flanagin BA, Cruz AI, Medvecky MJ. Hoffa fracture in a 14-year-old. Orthopedics 2011;34:138. [Google Scholar] [PubMed]
- 2. Afa H. Lehrbuch der Frakturen und Luxationen. Stuttgart: Verlag von Ferdinand Enke; 1904. p. 451. [Google Scholar] [PubMed]
- 3. Heuschen UA, Gohring U, Meeder PJ. Bilateral Hoffa fracture: A rarity. Aktuelle Traumatol 1994;24:83-6. [Google Scholar] [PubMed]
- 4. Lewis SL, Pozo JL, Muirhead-Allwood WF. Coronal fractures of the lateral femoral condyle. J Bone Joint Surg Br 1989;71:118-20. [Google Scholar] [PubMed]
- 5. Papadopoulos AX, Panagopoulos A, Karageorgos A, Tyllianakis M. Operative treatment of unilateral bicondylar Hoffa fractures. J Orthop Trauma 2004;18:119-22. [Google Scholar] [PubMed]
- 6. Zeebregts CJ, Zimmerman KW, Ten Duis HJ. Operative treatment of a unilateral bicondylar fracture of the femur. Acta Chir Belg 2000;100:1104-6. [Google Scholar] [PubMed]
- 7. Letenneur JL, Rogez JM, Lignon J, Bainvel JV. Hoffa’s fractures report of 20 cases (author’s transl). Ann Chir 1979;32:213-9. [Google Scholar] [PubMed]
- 8. Allman KH, Altehoefer C, Wildanger G, Gufler H, Uhl M, Seif el Nasr M, et al. Hoffa fracture – a radiologic diagnostic approach. J Belge Radiol 1996;79:201-2. [Google Scholar] [PubMed]
- 9. Ostermann PA, Neumann K, Ekkernkamp A, Muhr G. Long-term results of unicondylar fractures of the femur. J Orthop Trauma 1994;8:142-6. [Google Scholar] [PubMed]
- 10. Aratsu MH, Kokke MC, Duffy PJ, Korley RE, Buckley RE. Coronal plane partial articular fractures of the distal femoral condyle: Current concepts in management. Bone Joint J 2013;95-B:1165-71. [Google Scholar] [PubMed]
- 11. Muller ME, Allgower M, Schneider R. Manual of Internal Fixation. 3rd ed. New York, NY: Springer-Verlag; 1995. p. 549. [Google Scholar] [PubMed]
- 12. Schatzker J, Tile M. The Rationale of Operative Fracture Care. 2nd ed. Berlin: Springer-Verlag; 1996. p. 390-1. [Google Scholar] [PubMed]
- 13. P A Ostermann et al. Chirurg. Monocondylar fractures of the femur. Therapeutic strategy and clinical outcome. Oururg 1997;68:72-6 . [Google Scholar] [PubMed]
- 14. Manfredini M, Gildone A, Ferrante R. Unicondylar femoral fractures: Therapeutic strategy and longterm results. Acta Orthop Belg 2001;67:132-8. [Google Scholar] [PubMed]
- 15. Becker PL, Staford PR, Goulet R. Comparative Analysis for the Fixation of Coronal Distal Intraarticular Femur Fractures. In: Presented at the 67th Annual Meeting of the American Academy of Orthopaedic Surgeons; 2000. [Google Scholar] [PubMed]
- 16. Holmes SM, Bomback D, Baumgaertner MR. Coronal fractures of the femoral condyle. A brief report of five cases. J Orthop Trauma 2004;18:316-319. [Google Scholar] [PubMed]
- 17. Wallenbock E, Ledinski C. Indications and limits of arthroscopic management of intraarticular fractures of the knee joint. Aktuelle Traumatol 1993;23:97-101. [Google Scholar] [PubMed]
- 18. McCarthy JJ, Parker RD. Arthroscopic reduction and internal fixation of a displaced intraarticular lateral femoral condyle fracture of the knee. Arthroscopy 1996;12:224-7. [Google Scholar] [PubMed]
- 19. Stern RE. Arthroscopic reduction and internal fixation of a displaced intra-articular lateral femoral condyle fracture of the knee: case report. Arthroscopy 1996;12:760-1. [Google Scholar] [PubMed]
- 20. Demirel M, Dereboy F, Ozturk A, Turhan E. Arthroscopically assisted intra-articular lateral femoral condyle fracture surgery. Arthroscopy 2006;22:690.e1-4. [Google Scholar] [PubMed]
- 21. Ercin E, Bilgili MG, Basaran SH, Baca E, Kural C, Avkan MC. Arthroscopic treatment of medial femoral condylar coronal fractures and nonunions. Arthrosc Tech 2013;2:e413-5. [Google Scholar] [PubMed]