Addition of circumferential fiber augmentation (CFA) to bucket-handle discoid lateral meniscus repairs increases fixation strength and prevents re-tearing, ensuring excellent outcomes.
Dr. Abbas Bhatia, Department of Orthopaedics, Murup Hospital, 243, 3•15-daero, Masanhappo-gu - 51264, Changwon, South Korea. E-mail: drabbasbhatia@gmail.com.
Introduction: Bucket-handle tears of the lateral meniscus (LM) are uncommon in young athletes and are particularly challenging when associated with a discoid meniscus. Restoration of meniscal hoop tension is critical for functional recovery and to prevent reinjury. This case describes the application of the circumferential fiber augmentation (CFA) technique, initially reported by Kodama et al. (2024), for the repair of a bucket-handle tear in a discoid LM.
Case Report: A 20-year-old male sustained an acute twisting injury while playing soccer, resulting in a locked knee. Magnetic resonance imaging (MRI) revealed a displaced bucket-handle tear of a discoid LM. He underwent an all-inside meniscus repair using fiber-wire sutures combined with CFA using fibertape and transtibial pullout fixation with a knotless suture anchor.
Outcome: At 6-month follow-up, the patient achieved a full range of motion with the Lysholm 95, IKDC 92, and KOOS-Pain 90. MRI confirmed complete meniscal healing without extrusion or signal alteration.
Conclusion: Application of CFA in bucket-handle meniscus repair may enhance fixation strength and prevent recurrent tearing in active young patients, especially in discoid variants. This represents an evolution in biological and mechanical augmentation for complex meniscal injuries.
Keywords: Circumferential fiber augmentation, bucket handle tear, discoid lateral meniscus.
Meniscal bucket-handle tears represent approximately 10% of all meniscal injuries and commonly occur in young, active individuals following twisting or pivoting trauma [1,2]. Lateral meniscus (LM) tears, particularly in discoid variants, pose additional challenges due to abnormal morphology and increased risk of recurrence [3,4]. The bucket-handle tear causes mechanical locking and requires prompt surgical reduction and repair to restore knee kinematics.
Conventional inside-out or all-inside repairs restore stability but may not reconstitute native hoop tension. Loss of circumferential fiber integrity contributes to persistent meniscal extrusion and subsequent degenerative changes [5]. Circumferential fiber augmentation (CFA), described by Kita et al. and Kodama et al., involves reinforcement of the circumferential collagen network using high-strength fibertape sutures [6,7,8]. This biomechanical approach has shown superior tensile strength and reduced extrusion rates in root and radial tear cases. To the best of our knowledge, the use of CFA for a bucket-handle LM tear in a discoid meniscus has not been previously reported. This report presents a unique case of a young athlete successfully treated with meniscus repair combined with CFA, with excellent functional outcomes.
A 20-year-old male football player presented to the emergency department with acute right knee flexion deformity and locking after a twisting injury during play. Clinical examination revealed lateral joint-line tenderness, limited flexion, and inability to extend the knee fully. Lachman test and pivot shift tests were negative. Plain radiographs showed no fracture or dislocation. Magnetic resonance imaging (MRI) demonstrated a displaced bucket-handle tear of a discoid LM, with the classic double-posterior cruciate ligament sign and minimal chondral change (Fig. 1c-e).
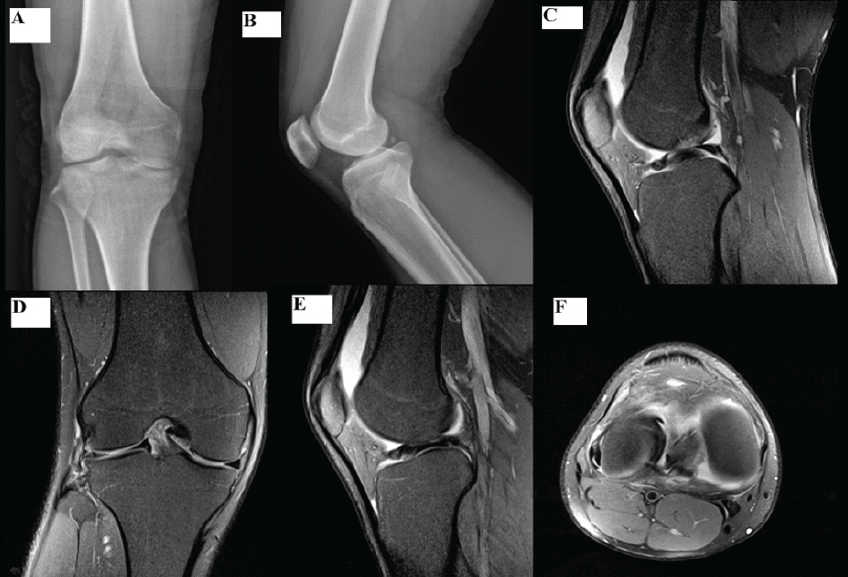
Figure 1: Pre-operative imaging of the right knee. (a) Anteroposterior radiograph showing flexion deformity due to meniscal locking. (b) Lateral radiograph of the knee. (c) Sagittal T2-weighted magnetic resonance imaging (MRI) showing the “double posterior cruciate ligament” sign (d) Coronal T2-weighted MRI showing a flipped meniscal fragment within the intercondylar notch. (e) Axial MRI showing a displaced meniscal fragment within the intercondylar notch, producing a characteristic double-layer (split-meniscus) appearance (f).
The patient was counselled for arthroscopic meniscus repair. Under spinal anesthesia and standard anterolateral and anteromedial portals, diagnostic arthroscopy was performed, confirming a displaced bucket-handle tear involving the body and posterior horn of the discoid LM (Fig. 2a and b). The meniscal fragment was reduced and stabilized with an arthroscopic probe.
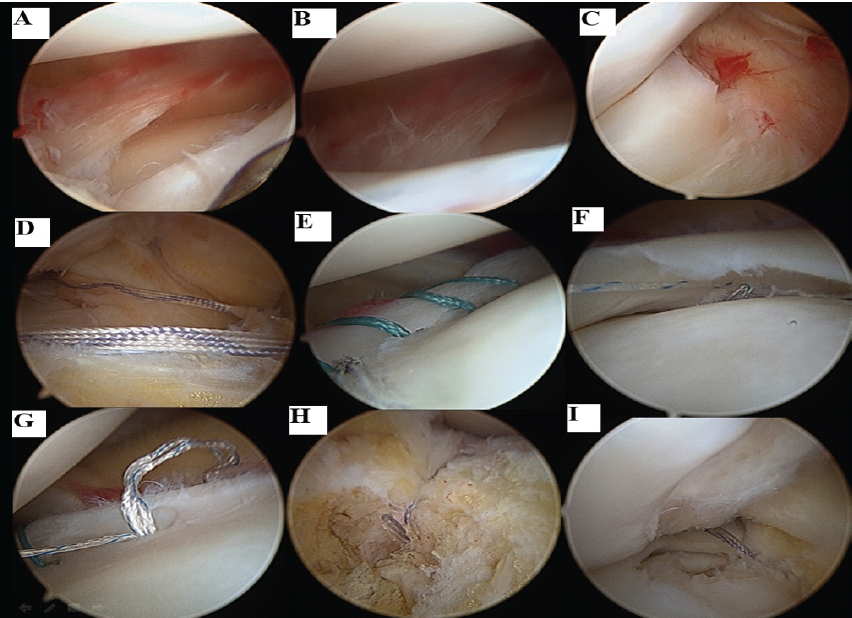
Figure 2: Intraoperative arthroscopic views. (a and b) Bucket-handle tear of the discoid lateral meniscus. (c) Flipped meniscal fragment within the intercondylar notch. (d) Passage of fiber tape for circumferential fiber augmentation (CFA). (e) Placement of inside-out sutures for the body of the lateral meniscus. (f and g) All-inside repair of the posterior horn of the lateral meniscus. (h) Anterior fixation of the fiber tape using a knotless suture anchor. (i) The Final view after CFA shows the posterior end of the fiber tape fixation and the complete repair construct.
The repair sequence started with the CFA technique (Fig. 3): A spinal needle was passed from the anterior horn to the body of the LM. The high-strength fibertape was then shuttled through the spinal needle and retrieved. A lateral incision was created. The spinal needle was then passed again from the body of the LM to the posterior horn/root region through this incision, and the fibertape was passed similarly to complete the circumferential loop (Fig. 2d). A transtibial tunnel was drilled using a guide jig, and the posterior thread of the fibertape was retrieved through this tunnel.
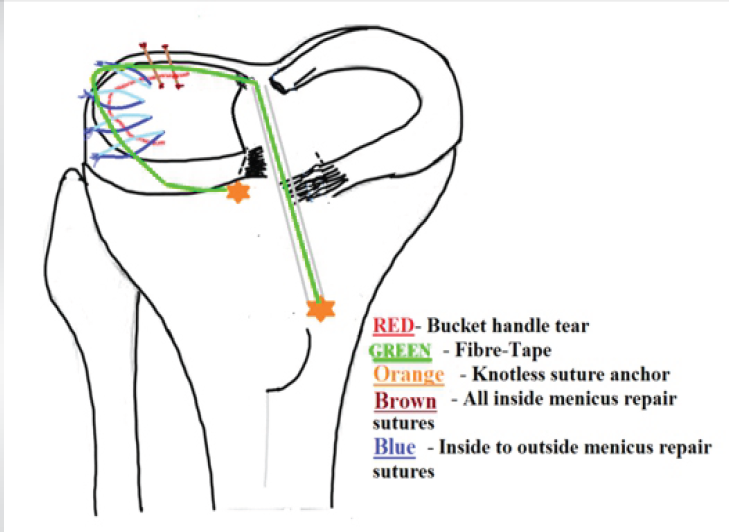
Figure 3: Schematic diagram showing circumferential fiber augmentation (CFA) in a discoid lateral meniscus bucket-handle tear. The fiber tape for CFA is first passed through the substance of the meniscus from anterior to posterior. Four inside-out suture wires are then passed through the body of the lateral meniscus, and the posterior horn is secured using two all-inside meniscal sutures. Following completion of the primary meniscal repair, the CFA construct is fixed anteriorly with a knotless suture anchor and posteriorly through a tibial tunnel drilled medial to the lateral meniscus posterior root. The posterior end of the fiber tape is retrieved through the tunnel, tensioned appropriately, and secured over the anteromedial tibial cortex. Finally, the four inside-out sutures are secured to complete the repair.
Next, the primary repair threads were passed: four inside-out fiber-wire sutures were meticulously placed across the tear in the body of the LM (Fig. 2e). Subsequently, the posterior horn segment was secured using two all-inside sutures (Fig. 2f and g).
With all threads in place, the fixation steps began. First, the CFA was secured to restore meniscal hoop tension: A knotless suture anchor was placed on the tibial plateau just anterior to the anterior horn of the LM to fix the anterior end of the fibertape (Fig. 2h). The fibertape was then tensioned under arthroscopic visualization, and the posterior thread exiting the transtibial tunnel was secured with a second knotless suture anchor placed in the anteromedial tibial cortex (Fig. 2i). Finally, the four inside-out sutures were tied over the posteromedial and anteromedial capsule, ensuring anatomical reduction and secure compression of the main body tear. Intraoperative probing confirmed stable fixation without displacement. No meniscal trimming was performed; this preservation was crucial for construct stability, given the scant lateral tissue remaining due to the peripheral tear pattern.
Postoperatively, the knee was immobilized in extension for 1 week, followed by a progressive range of motion up to 90° for 4 weeks. Partial weight bearing began at 6 weeks and full weight bearing at 8–10 weeks. At 6 months, the patient demonstrated a full range of motion without pain or effusion. The Lysholm score was 95, IKDC 92, and KOOS-Pain 90. Follow-up MRI showed an intact, healed meniscus with no residual tear or extrusion (Fig. 4). The patient resumed light football training after 5 months.
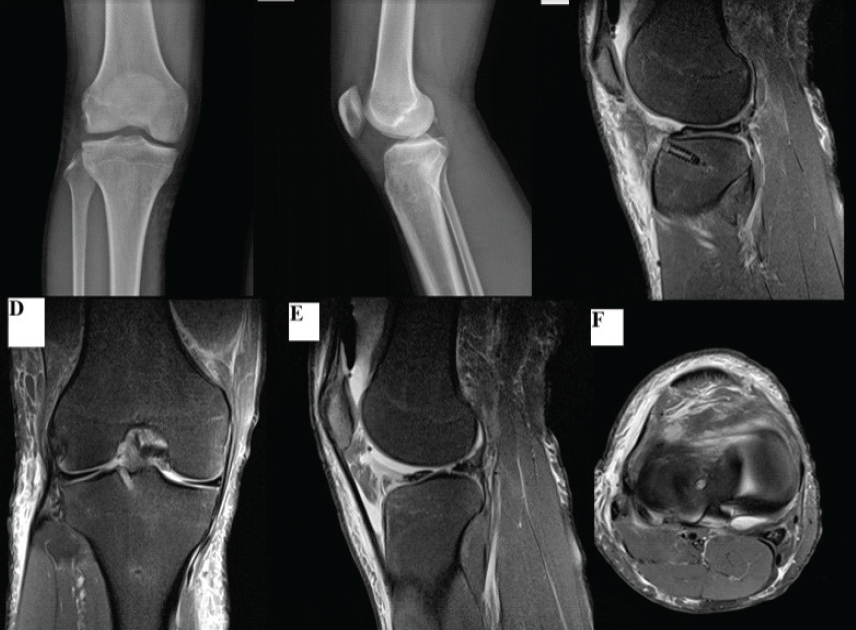
Figure 4: Post-operative imaging of the right knee following circumferential fiber augmentation (CFA) repair of a bucket-handle tear in the discoid lateral meniscus. (a) Anteroposterior knee radiograph showing restoration of joint space and correction of flexion deformity. (b) Lateral knee radiograph demonstrating maintained reduction of the meniscus. (c) Sagittal T2-weighted magnetic resonance imaging (MRI) showing anatomical reduction of the meniscus with resolution of the “double posterior cruciate ligament” sign. (d) Coronal T2-weighted MRI confirming a stable meniscal contour without a displaced fragment. (e) Sagittal T2-weighted MRI showing continuity of the repaired discoid meniscus with preserved thickness. (f) Axial MRI demonstrating a well-seated meniscus without a displaced fragment or double-layer appearance.
Bucket-handle tears of the LM in young athletes require stable anatomic repair to preserve meniscal function and prevent degenerative arthritis. The discoid LM is structurally prone to instability and retear due to its collagen arrangement pattern and thickness [3]. In the present case, the combined meniscus repair and CFA technique provided anatomic reduction and biomechanical reinforcement (Fig. 3). The fibertape acts as an external circumferential scaffold that restores hoop tension and distributes load evenly across the repaired segment [6,8]. This hybrid construct potentially reduces suture pullout and retear risk, critical for athletes returning to high-demand sports. Previous studies have highlighted that standard suture repairs may not completely restore hoop stress, particularly in root or radial tears [5,9]. Kita et al. first demonstrated the biomechanical superiority of CFA in reducing extrusion and improving fixation stiffness [6]. Kodama et al. modified this technique for medial meniscus posterior root tears with transtibial pullout repair, showing improved meniscal reduction and durability [8]. Although not previously applied to bucket-handle tears, the underlying principle of augmenting circumferential tension remains relevant. In our case, this reinforcement prevented gapping during motion and enabled early rehabilitation. CFA uses ultra-high-molecular-weight polyethylene fibertape, which has greater tensile capacity than traditional sutures, reducing the risk of tissue cutout [7,10]. Adding a transtibial anchor provides stable fixation without bulky knots within the joint. Biomechanical studies confirm that augmented constructs maintain stability beyond 30–40 N of traction, sufficient for early range of motion protocols [8,11]. In contrast, conventional sutures often fail at 15–20 N, leading to micro-failure and recurrent extrusion. Our post-operative MRI confirmed complete meniscus healing with restoration of native contour, supporting these findings (Fig. 4). The clinical implication of this case lies in the feasibility of extending CFA beyond root or radial tears to include complex bucket-handle patterns. In athletes, the higher functional load and higher reinjury risk warrant stronger repair constructs. This approach may particularly benefit discoid menisci, which experience greater shear stress during flexion-extension cycles. Limitations include a single case and short-term follow-up, but the results encourage further evaluation of CFA-assisted meniscus repairs in larger series.
Bucket-handle meniscus repair combined with CFA provides robust fixation and restoration of hoop tension. This technique may reduce recurrence and facilitate earlier rehabilitation in young athletes with discoid meniscus morphology. Further biomechanical and clinical comparative studies are needed to validate long-term efficacy.
Bucket-handle meniscus repair combined with CFA offers robust fixation and restores meniscal hoop tension. This hybrid construct may reduce the risk of recurrence and facilitate earlier rehabilitation in young athletes, particularly those with discoid meniscus morphology.
References
- 1. Bedi A, Kelly N, Baad M, Fox AJ, Ma Y, Warren RF, et al. Dynamic contact mechanics of radial tears of the lateral meniscus: Implications for treatment. Arthroscopy 2012;28:372-81. [Google Scholar] [PubMed]
- 2. Bin SI, Kim JM, Shin SJ. Radial tears of the posterior horn of the medial meniscus. Arthroscopy 2004;20:373-8. [Google Scholar] [PubMed]
- 3. Ahn JH, Lee SH, Yoo JC. Arthroscopic all-inside repair of bucket-handle tears in the discoid lateral meniscus. Arthroscopy 2008;24:1345-50. [Google Scholar] [PubMed]
- 4. Song JG, Lee BS, Lee CC. Results of meniscal all-inside repair for discoid lateral meniscus tears. Knee Surg Sports Traumatol Arthrosc 2022;30:1945-53. [Google Scholar] [PubMed]
- 5. Kawada K, Furumatsu T, Tamura M, Xue H, Higashihara N, Kintaka K, et al. Medial joint space narrowing progresses after pullout repair of medial meniscus posterior root tear. Int Orthop 2023;47:2401-7. [Google Scholar] [PubMed]
- 6. Kita K, Kusano M, Tsujii A, Ohori T, Tanaka Y, Nakamura N, et al. Meniscal circumferential fiber augmentation: A biomechanical arthroscopic meniscal repair technique. Arthrosc Tech 2023;12:e1673-8. [Google Scholar] [PubMed]
- 7. Furumatsu T, Miyazawa S, Kodama Y, Kamatsuki Y, Okazaki Y, Hiranaka T, et al. Clinical outcomes of medial meniscus posterior root repair: A midterm follow-up study. Knee 2022;38:141-7. [Google Scholar] [PubMed]
- 8. Kodama Y, Masuda S, Yokomizo D, Ohmori T, Tanaka M. Circumferential fiber augmentation technique combined with transtibial pullout repair. Arthrosc Tech 2024;13:103132. [Google Scholar] [PubMed]
- 9. Bhatia S, LaPrade CM, Ellman MB, LaPrade RF. Meniscal root tears: Significance, diagnosis, and treatment. Am J Sports Med 2014;42:3016-30. [Google Scholar] [PubMed]
- 10. Boksh K, Haque A, Sharma A, Divall P, Singh H. Use of suture tapes versus conventional sutures for arthroscopic rotator cuff repairs: A systematic review and meta-analysis. Am J Sports Med 2022;50:264-72. [Google Scholar] [PubMed]
- 11. Moon HK, Cho SH, Kim SH. Simultaneous meniscus root repair and high tibial osteotomy: Outcomes and extrusion control. Am J Sports Med 2023;51:2152-60. [Google Scholar] [PubMed]
- 12. Park DY, Yin XY, Chung JY, Jin YJ, Kwon HJ, Lee GB, et al. Circumferential rim augmentation suture around the perimeniscal capsule decreases meniscal extrusion and progression of osteoarthritis in rabbit meniscus root tear model. Am J Sports Med 2022;50:689-98. [Google Scholar] [PubMed]