The Halifax intramedullary nail helps us in managing intertrochanteric fractures, mainly in osteoporotic bone, effectively, with complications such as increased operating time, blood loss, Z and reverse Z effect, which is the most common complication seen in conventional cephalo-medullary intramedullary nail. This study will introduce the new tri-wire concept in the field of orthopedics
Dr. S. Naveen, Department of Orthopaedics, Government Stanley Medical College and Hospital, Chennai - 600001, Tamil Nadu, India. E-mail: dr.navy278@gmail.com
Introduction: Intertrochanteric fractures are common in elderly patients and can lead to significant malunion and varus deformities if untreated. While the dynamic hip screw has been the gold standard, there is a continuous effort to evaluate newer fixation devices. This study assesses the functional and radiological outcomes of intertrochanteric femur fractures treated with the Halifax nail, aiming to provide a contemporary comparison to existing methods.
Materials and Methods: This prospective study was conducted at our institution from January 2019 to December 2024. We included patients with intertrochanteric fractures, excluding those with open fractures, pathological fractures, pre-operative neurovascular deficits, or polytrauma with head injuries. All patients underwent surgery under spinal anesthesia on a fracture table. Closed reduction was attempted under C-arm guidance; if unsuccessful, open reduction was performed. The Halifax nail was inserted after a tensor fascia lata and gluteus medius split. This was followed by lag screw insertion with tri-wire guidance, end cap application, and distal locking.
Results: The study included 57 patients (31 male and 26 female). Fracture classifications were 11 AO type A1, 23 AO type A2, and 23 AO type A3. The average surgery duration was 65 min, with an average blood loss of about 200 mL. Patients achieved an average time to union of 11.7 weeks, and the functional outcome, measured by the average Harris Hip score, was 91.
Conclusion: The findings suggest that the Halifax nail provides favorable functional and radiological outcomes for intertrochanteric femur fractures. Its use resulted in good union rates and high patient function, indicating that it is a viable and effective treatment option. Further comparative studies are needed to confirm its role in orthopedic practice.
Keywords: Halifax, intramedullary nail, intertrochanteric fracture, tri-wire.
Intertrochanteric fractures are one of the most common fractures in elderly patients [1]. About 50% of all hip fractures caused by falls in the elderly are found to be intertrochanteric. The osteoporotic nature of bone quality in elderly people makes them more prone to sustaining intertrochanteric fractures [1,2]. These patients are limited to home ambulation, since most of them are elderly. If the fracture is not stabilized and patients are not mobilized early, it will end up in a poor recovery of functional independence [3,4,5]. Risk factors for intertrochanteric fractures include – elderly person >60 years, female gender, most commonly in the postmenopausal age group , Osteoporosis , low bone density, and reduced muscle mass [6,7,8,9].
An intertrochanteric fracture occurs through the metaphyseal region of the bone, which has excellent blood supply. If they are left untreated, they will go for malunion leading to varus deformity. Posteromedial fragmentation, lateral wall fracture, reverse oblique pattern, and failure of fracture reduction before internal fixation are the unstable characteristics of intertrochanteric fractures [10,11,12]. The dynamic hip screw (DHS) is a gold standard device used in the management of stable intertrochanteric fractures. In stable types of intertrochanteric fractures, DHS provides good results through controlled collapse of fracture fragments. When used in unstable fractures with lateral wall fracture and posteromedial comminution, it may result in varus collapse of the proximal fragment and medialization of the distal shaft fragment [13,14,15,16]. Intramedullary devices like proximal femoral nail (PFN), Gamma nail, Halifax nail prevent medialization of the distal shaft fragment and provide additional stability in unstable fractures. The patient can be started on early weight bearing and mobilization, and early union [12,17,18]. While the primary focus remains on the frequently encountered unstable intertrochanteric fractures in osteoporotic and elderly patients, this investigation also includes a comprehensive analysis of the Halifax nail’s efficacy across a broader spectrum of intertrochanteric fracture types and patient demographics, including younger individuals with less complex fractures, where its unique design may offer specific advantages.
This study aims to assess the functional and radiological outcomes of intertrochanteric femur fractures treated with Halifax nail at our institution/hospital between January 2019 and December 2024.
A prospective study of the management of intertrochanteric fractures by the Halifax nail was undertaken at our institution over a period of 5 years (January 2019 to December 2024). All participants provided written informed consent before enrollment in the study. The study was conducted in accordance with the ethical principles of the Declaration of Helsinki.
The study included 57 patients above 40 years of age, who presented to the trauma ward with a closed intertrochanteric fracture with any mode of injury.
Patients were excluded from the study if they presented with open intertrochanteric fractures, pathological fractures resulting from an underlying disease process, pre-existing neurovascular deficits on the ipsilateral fracture limb, polytrauma involving two or more severe injuries in at least two body regions, or concomitant head injury requiring prolonged initial stabilization.
Procedure for Halifax nailing
All patients were given spinal anesthesia (Sub-Arachnoid block), and the patient was positioned in a fracture table in the supine position, with the unaffected hip kept in an abducted position and the affected limb secured in a traction boot (Fig. 1a). The C-Arm was positioned in a way to change positions according to anteroposterior and lateral views. Closed reduction attempted under C Arm guidance. Once the status of reduction is achieved, the patient’s parts are painted and draped. If closed reduction was not achieved, we used a spike instrument through a small anterior incision to lift the proximal fragment (Fig. 1b). A 5 cm skin incision was made just above the tip of the greater trochanter. Subcutaneous tissue was dissected. The tensor fascia lata was cut. The gluteus medius was split along the line of fibers. The tip of the greater trochanter was identified. A bony entry was made using a cannulated bone awl at the tip of the greater trochanter (Fig. 1c). A guide wire was passed inside the cannulated bone awl, and the guide wire position was checked under C-arm guidance in anteroposterior and lateral views (Fig. 1d). Proximal reaming was done using a 16 mm reamer (Fig. 1e). Halifax nail was assembled and inserted and checked under C-arm guidance (Fig. 1f). A lateral cortex breaker was used to break the lateral cortex and used up to the neck level (Fig. 1g). The guide wire for a lag screw was passed at the center of the neck and head. Guide wire position was checked under C-arm guidance in both anteroposterior and lateral views (Fig. 1h). Reaming for lag screw was done (Fig. 1i). A lag screw of appropriate size was inserted up to the subchondral level. The lag screw was inserted in a way that 5 mm of its length was kept outside the lateral cortex (Fig. 1j). The set screw was applied from the top of the nail by a set screw introducer and fully tightened till it engages one of the grooves in the lag screw to prevent the “Z” and reverse “Z” effect. Moreover, the introducer was left along with the set screw. The tri-wire of size 5 mm, shorter than the lag screw, was inserted till it engages in the sub-chondral bone, and the position was checked under C-arm guidance (Fig. 1k). Now, using the set screw introducer, the fully tightened set screw was released 1/4th turn. This is to maximize the micro movements between the fracture fragments. The introducer was removed now. End cap was applied in the lateral end of the lag screw in a way to cover the outer prominence of tri-wire, to prevent the tri-wire pull out (Fig. 1l). Distal locking was applied mostly in the dynamic position using the sleeve (Fig. 1m). A head cap was applied over the top of the nail after removing the Jig to prevent bony overgrowth inside the nail top (Fig. 1n). Final position of nail was checked under C-arm guidance in both anteroposterior and lateral views (Fig. 1o). A thorough wound wash was given, and the wound was closed in layers. A sterile dressing was applied.
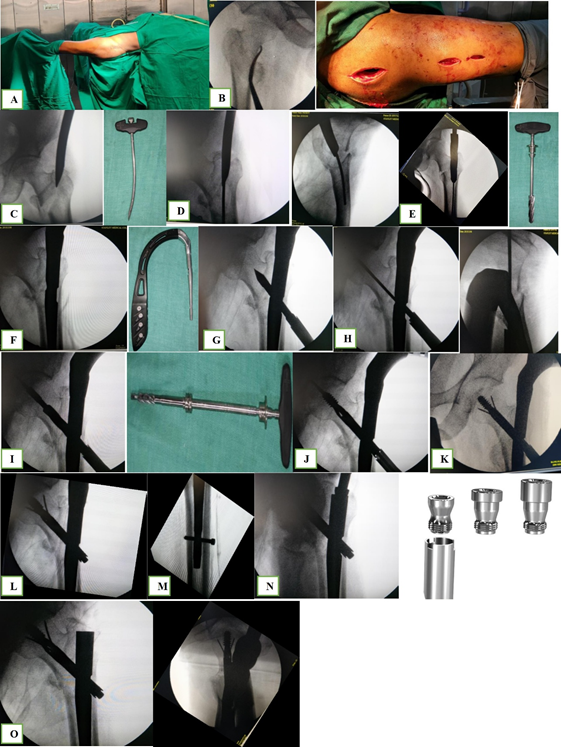
Figure 1: Intraoperative picture and Halifax nail instrumentation.
Post-operative protocol
All patients who underwent surgery were given intravenous (IV) antibiotics for 3 days. Limb elevation was advised to prevent edema. On post-operative day 1, knee and hip passive mobilization were started. Weight-bearing protocol was followed as per PFN or GAMA nail, like all stable intertrochanteric fractures with dynamic or static locking, were started on early weight bearing. Unstable intertrochanteric fracture with stable bone contact and fixation was started on early weight bearing. Unstable intertrochanteric fractures with poor bone contact or comminuted fractures were advised for delayed weight bearing for up to 6 weeks.
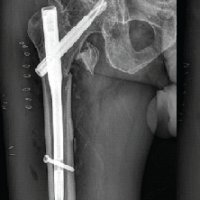
All patients were discharged on day 5 after the 2nd post-operative dressing. All patients were reviewed every 15 days for the first 2 months and monthly from the 2nd month to the 6th month. The union status was checked by every monthly radiograph of anteroposterior and lateral views of the affected hip and thigh. Modified Harris hip score was used for all patients at the 3rd and 6th months of follow-up to evaluate the functional outcome (Fig. 2).
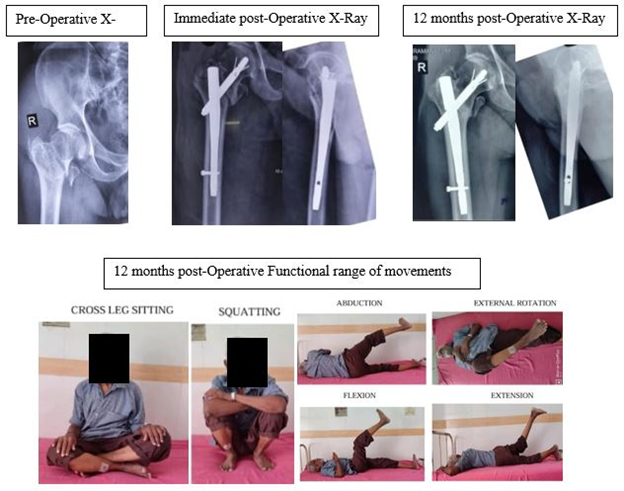
Figure 2: X-rays and post-operative functional movements.
In this study, out of 57 patients with intertrochanteric fractures treated with the Halifax nail, 31 (54%) were male patients, and 26 (46%) were female patients. Right-sided it was 38 (66%) and left-sided 19 (33%). Road traffic accident by mode of injury was 17 (29%), whereas self-fall where 40 (71%). Fracture according to AO type A1 were 11 (19.2%), A2 were 23 (40.3%), and A3 were 23 (40.3%). The average time interval between injury and fixation was 9.3 days. Out of 57 cases, 42 (73%) were operated on by closed reduction technique, whereas 15 (27%) by open reduction technique. The average duration of the procedure was 65 min (Chart 1), and the average blood loss was around 200 mL. Out of 57 cases, 9 (16%) patients achieved union at around 8–9 weeks, while 24 (42%) at 10–13 weeks, and 24 (42%) at 14–16 weeks (Chart 2).
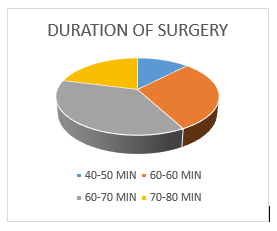
Chart 1: Duration taken for surgery.
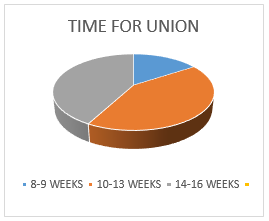
Chart 2: Time taken for fracture union.
Functional outcome by the Harris hip score at 3 months follow-up was found to be in the range of 62 (minimum) to 85 (maximum), with an average value of 79.63.
Harris hip score at 6-month intervals, ranging from a minimum of 78 to a maximum of 98, with an average of 91.42.
Out of 57 cases, in one case, we have encountered the breakage of the tri-wire at 12 weeks of follow-up. Since the fracture was not united, we have done an implant exit followed by Cemented Hemiarthroplasty. This could probably be due to the lag screw position not being in the center, and static distal locking was applied. In one case, we have encountered peri-implant fracture at the level of the distal locking site because of the sustained injury to the same hip by a fall, which our patient sustained at 15 weeks after the surgery. We have done the implant exit and planned for Long PFN subsequently. Superficial skin infection in one case, which subsided with IV antibiotics and wound dressing.
A major limitation of this study was the small sample size; however, our institution was the first in Tamil Nadu which use the Halifax nail for intertrochanteric fracture.
The future direction would be to study the outcome of the Halifax nail in a larger population.
Intertrochanteric fractures remain a significant concern in elderly populations, given their high incidence and the complexities associated with osteoporotic bone. Despite numerous treatment modalities and implants, a universal gold standard remains elusive due to the diverse nature of fracture patterns and bone quality. This discussion evaluates the performance of the Halifax nail in comparison to established implants like the DHS and PFN, considering biomechanical advantages and clinical outcomes, while also acknowledging the limitations of our study [1].
The DHS, an extramedullary load-bearing device, provides excellent results in stable fractures. However, its effectiveness in unstable fractures is questionable, largely due to its long lever arm. This extended lever arm can lead to increased stress on weight-bearing, potentially causing complications such as lag screw cutout, implant failure, varus collapse, and non-union [6].
In contrast, intramedullary devices such as the PFN and Halifax nail are load-sharing, offering superior biomechanical stability. This inherent stability allows for earlier weight-bearing and ambulation, crucial for elderly patients. The PFN is a time-tested and proven device for intertrochanteric fractures, yet it presents challenges such as anterior thigh pain and difficulty in inserting derotation screws, particularly when the femoral neck is short [7,8].
The Halifax nail addresses several limitations of conventional implants. Its shorter length is particularly advantageous for the Asian population, where the femoral curvature above the isthmus is often more pronounced. This reduced length minimizes stress on the anterior cortex, potentially mitigating anterior thigh pain and femoral shaft stress fractures, complications observed with longer nails. In our study, none of our patients reported anterior thigh pain, suggesting a reduced incidence of this complication with the HALIFAX nail [5,6,9].
A key innovation in the HALIFAX nail is the single 10.5 mm lag screw with a 1.8 mm tri-wire, inserted directly through the lag screw. This design overcomes the difficulty encountered with the PFN’s 8 mm lag screw and 6.2 mm derotation screw, especially in cases of short femoral necks [10]. The tri-wire is designed to provide enhanced rotational stability compared to conventional derotation screws in PFNs, due to its greater contact area and superior subchondral bone purchase, which is particularly beneficial in osteoporotic bone. Although the “Z” or “Reverse Z” effect, a known complication with some implants, was not observed in our 57 patients, we did encounter one instance of tri-wire breakage.
The conventional PFN has a length of 240 mm, whereas in the HALIFAX nail, it is about 180 mm. In the Asian population, the curvature of the femur is more above the level of the isthmus. Hence, a conventional PFN nail will cause more stress in the anterior cortex, which may lead to anterior thigh pain and femoral shaft stress fractures, which was already discussed by Tuladhar and Chang [11]. This complication is overcome in the HALIFAX nail by a short nail length of 180 mm. In our study, none of our patients reported anterior thigh pain. Hence, the incidence of anterior thigh pain is reduced.the average time of 12 weeks for gamma nail in the study conducted by Herrera et al. [12].
Regarding functional outcomes, our study reported that Harris Hip Scores were obtained for excellent results in 58% of patients and good results in 38%, with an average Harris hip score of 91.42. These outcomes are comparable to the study done by Shah et al. [4] study in which excellent results were obtained in 80% patients and good results were obtained in the remaining 20% with an average Harris hip score of 93.8 for gamma nail. While the Gamma nail results appear slightly superior in terms of excellent outcomes, our findings still demonstrate a high level of functional recovery with the HALIFAX nail.
The ability of intramedullary nails, such as the Gamma nail, to achieve stability and satisfactory union even in unstable fracture patterns without requiring anatomical reduction of comminuted posteromedial fragments is a significant advantage, as discussed by Halder [13].
Under the same workload, the GAMMA nail supported higher stress than PFN. This was reported by Seral et al. [10]. Tri-wire is strongly bonded and offers good resistance to rotational deforming forces in the distal tibia, as discussed by Halder et al. [14]. They have also mentioned that tri-wire provides a better locking option in the proximal humerus, which will preserve the function of rotator cuff muscles [14].
Despite the study spanning approximately 5 years, the follow-up period for individual patients was relatively taken, as per the union status of the corresponding patient. All the patients were followed up for a minimum period of 3 years.
Halifax nail provides excellent functional outcome and an unimpaired quality of life. Halifax nail reduces the duration of hospital stay with early weight bearing and rehabilitation, leading to a decrease in the incidence of complications like bed sores and deep vein thrombosis. It is a less invasive procedure with shorter duration of surgery and minimal blood loss with preservation of fracture hematoma, which will reduce the chances of post-operative infections. Halifax nail provided early consolidation of fractures with higher union rates and excellent functional outcome in our study. Use of the tri-wire concept is a novel modality in the treatment of intertrochanteric fractures. The efficacy of tri-wire has been proven in the proximal humerus and distal tibia fractures. In intertrochanteric fractures, tri-wire provides better rotational stability. The major limitation of this study was that there was no comparative group. Our study concludes that the HALIFAX nail can be the future in the management of intertrochanteric fractures.
In the current scenario, the majority of the intertrochanteric fractures are being treated with the cephalo-medullary nail system, such as PFN, PFN-A2, and TFN. Since this type of fracture is seen in elderly people, osteoporosis is one of the challenging issues for the operating surgeon, which is addressed through screw purchase as well as two screw concept to give rotational stability. This implant will have one neck screw with a tri-wire, which ensures both bone purchase and rotational stability.
References
- 1. Rockwood CA. Rockwood and Green’s Fractures in Adults. New York: Lippincott; 1991. [Google Scholar] [PubMed]
- 2. Lu Y, Uppal HS. Hip Fractures: Relevant Anatomy, Classification, and Biomechanics of Fracture and Fixation. Geriatr Orthop Surg Rehabil. 2019 Jul 3;10:2151459319859139. doi: 10.1177/2151459319859139. PMID: 31321116; PMCID: PMC6610445. [Google Scholar] [PubMed] [CrossRef]
- 3. Zhuang HF, Wang PW, Li YZ, Lin JK, Yao XD, Xu H. Analysis of related factors of brittle hip fracture in postmenopausal women with osteoporosis. Orthop Surg 2020;12:194-8. [Google Scholar] [PubMed]
- 4. Tan BY, Lau AC, Kwek EB. Morphology and fixation pitfalls of a highly unstable intertrochanteric fracture variant. J Orthop Surg (Hong Kong) 2015;23:142-5. [Google Scholar] [PubMed]
- 5. Kumar R, Singh RN, Singh BN. Comparative prospective study of proximal femoral nail and dynamic hip screw in treatment of intertrochanteric fracture femur. J Clin Orthop Trauma 2012;3:28-36. [Google Scholar] [PubMed]
- 6. Cotton FJ. Artificial impaction in hip fracture. JBJS 1911;2:680-6. [Google Scholar] [PubMed]
- 7. Bridle SH, Patel AD, Bircher M, Calvert PT. Fixation of intertrochanteric fractures of the femur. A randomised prospective comparison of the gamma nail and the dynamic hip screw. J Bone Joint Surg Br 1991;73:330-4. [Google Scholar] [PubMed]
- 8. Werner-Tutschku W, Lajtai G, Schmiedhuber G, Lang T, Pirkl C, Orthner E. Intra-and perioperative complications in the stabilization of per-and subtrochanteric femoral fractures by means of PFN. Unfallchirurg 2002;105:881-5. [Google Scholar] [PubMed]
- 9. Seral B, Garcia JM, Cegonino J, Doblare M, Seral F. Finite element study of intramedullary osteosynthesis in the treatment of trochanteric fractures of the hip: Gamma and PFN. Injury 2004;35:130-5. [Google Scholar] [PubMed]
- 10. Tuladhar R, Chang SM. Femoral intertrochanteric nails: The post-operative complications via radiographic study. IJSIT, 2020;9(5):232-239. [Google Scholar] [PubMed]
- 11. Herrera A, Domingo LJ, Calvo A, Martinez A, Cuenca J. A comparative study of trochanteric fractures treated with the Gamma nail or the proximal femoral nail. Int Orthop 2002;26:365-9. [Google Scholar] [PubMed]
- 12. Halder SC. The Gamma nail for peritrochanteric fractures. J Bone Joint Surg Br 1992;74:340-4. [Google Scholar] [PubMed]
- 13. Halder SC, Chapman JA, Choudhury G, Wallace WA. Retrograde fixation of fractures of the neck and shaft of the humerus with the ‘Halder humeral nail’. Injury 2001;32:695-703. [Google Scholar] [PubMed]
- 14. Kalhor M, Beck M, Huff TW, Ganz R. Capsular and pericapsular contributions to acetabular and femoral head perfusion. J Bone Joint Surg Am 2009;91:409-18. [Google Scholar] [PubMed]
- 15. Collin PG, D’Antoni AV, Loukas M, Oskouian RJ, Tubbs RS. Hip fractures in the elderly-a clinical anatomy review. Clin Anat 2017;30:89-97. [Google Scholar] [PubMed]
- 16. Miedel R, Ponzer S, Törnkvist H, Söderqvist A, Tidermark J. The standard Gamma nail or the Medoff sliding plate for unstable trochanteric and subtrochanteric fractures: A randomised, controlled trial. J Bone Joint Surg Br 2005;87:68-75. [Google Scholar] [PubMed]
- 17. Shah FY, Gul IA, Kotwal HA. Gamma nail in the management of intertrochanteric fractures of femur in adults. Int Surg J 2018;5:2487-92. [Google Scholar] [PubMed]