Ultrasound imaging should be considered routinely for the diagnosis and effective management of entrapment neuropathies, along with electrodiagnostic studies, and a population-specific dataset could be more beneficial for this purpose.
Dr. Amit Kumar, Department of Orthopaedics, All India Institute of Medical Sciences, Kalyani, West Bengal, India. E-mail: amitdr87@gmail.com
Introduction: Ultrasound (US) examinations of the ulnar nerve and measurement of cross-sectional area (CSA) are now used to diagnose cases of ulnar neuropathy. However, the CSA values vary across the population. The present study was planned to prepare a preliminary dataset of ulnar CSA among the symptomatic ulnar neuropathy patients diagnosed by electrodiagnostic studies at our institute and compare the values with those of healthy volunteers.
Materials and Methods: A hospital-based case–control study was conducted, which included 20 diseased upper limbs diagnosed with ulnar neuropathy and 40 non-neuropathic upper limbs as controls. They all underwent an US examination of the ulnar nerve in both upper limbs. The demographic data, nerve CSA at five predetermined locations, swelling and flattening ratios were compared and analyzed.
Results: The mean values of ulnar CSA at the medial epicondyle, 5 cm proximal and distal to it, at mid-forearm, and at the wrist were 11.5 ± 2.38 mm2, 7.43 ± 1.47 mm2, 6.17 ± 1.42 mm2, 5.78 ± 2.53 mm2, and 4.67 ± 2.3 mm2, respectively, in ulnar neuropathy patients. All the values were statistically significantly higher in cases than in controls. The swelling and flattening ratios were statistically significantly higher in ulnar neuropathy cases than in controls.
Conclusion: This study presents a data set of ulnar nerve CSA and some other parameters for the ulnar neuropathy patients and the normative values of ulnar nerve CSA in healthy subjects for the population of West Bengal (Eastern India). This data might be helpful for the diagnosis and management of ulnar neuropathy in this region.
Keywords: Ulnar nerve, medial epicondyle, forearm, wrist, ultrasound, measurement.
Ulnar neuropathy is a disorder of the ulnar nerve resulting in muscular weakness of the forearm and hand muscles and sensory alteration along its distribution [1,2]. The ulnar neuropathy is the second most common type of peripheral neuropathy, preceded by the median neuropathy at the carpal tunnel [1,3,4,5]. A common site of ulnar entrapment is at the cubital tunnel around the elbow; however, the focal compression or injury might occur at the wrist, forearm, or axilla [1,4,5]. With suggestive clinical features and physical examination findings, the electrodiagnostic assessment has been regarded as the gold standard for diagnosing entrapment neuropathy [3,6]. However, in an electrodiagnostic study, there is a practical difficulty in measuring curvilinear distances across the elbow, elevated temperature sensitivity of the nerve, and the discrepancy between nerve and skin distance in individuals with a high body mass index (BMI), leading to limited sensitivity and specificity. Moreover, this test might be unable to detect neuropathy in the early stages, and is often unable to localize the site of the lesion if axonal loss is present [6,7]
Figuring out the altered structural pathology often becomes helpful for definitive diagnosis of this condition and planning related surgery. Therefore, radiological investigations, including magnetic resonance imaging (MRI) or ultrasound (US), are indicated to localize the entrapment site and find any structural pathology causing compression for further confirmation and definitive diagnosis. The US is a non-invasive, quick, cost-effective, and easy-to-perform investigation that effectively identifies structural neuromuscular pathologies, including ulnar neuropathy. Previous studies yielded US’s high sensitivity and specificity, if combined with nerve conduction study, ranging from 80% to 95% in diagnosing ulnar neuropathy based on larger nerve diameter/cross-sectional area (CSA) [1,3,5,8]. Studies have proved that the nerve CSA measured by MRI and US is equivalent [9].
Various studies have reported a wide range of ulnar nerve CSA for the healthy population, including people with different age groups, gender, BMI, and ethnicity. Other studies provided some positive association of ulnar CSA with different parameters, including age, BMI, gender, ethnicity, etc. [9,10,11,12,13]; others found a negative association with age [13]; ultimately showing an inconsistent association. Higher CSAs have been observed in the Western population compared to the Asian population. All these indicate the importance of preparing population-specific data for radiologic diagnosis of ulnar neuropathy. The present study was planned to accumulate baseline data on ulnar nerve CSA among patients diagnosed with ulnar neuropathy and comparable healthy controls in a hospital-based population of West Bengal.
This observational and case–control study was conducted among the hospital-based population at our tertiary care institute. After obtaining ethical approval, the CSA of the ulnar nerve was recorded at predetermined sites for both diseased (cases) and non-diseased upper limbs (controls). A convenience sampling of 20 consecutive upper limbs diagnosed with ulnar neuropathy over a 1-year study period (April 2024-April 2025) was recruited as cases. The cases were recruited after applying the inclusion and exclusion criteria. The patients aged 18–60 years, with signs and symptoms suggestive of ulnar neuropathy persisting for 3 weeks or more, and finally diagnosed as a case of ulnar entrapment neuropathy by electrodiagnostic study, were included in the study. Patients with any metal implants in the affected limb, or cases that were caused by cervical myelopathy, plexopathy, radiculopathy, Hansen’s disease, or Amyloidosis, were excluded from this study. The age and gender matched controls, devoid of pain, discomfort, or weakness in the ulnar nerve territory, were recruited from the healthy volunteers accompanying the patient.
One experienced radiologist, blinded to cases and controls, assessed all the patients to reduce observer and inter-observer bias. The US was done after taking appropriate consent from both cases and controls. The measurements of ulnar nerve CSA were taken at the following predetermined sites: At the level of the medial epicondyle (ME), 5 cm proximal and distal to ME, and at the midpoint of the forearm and at the wrist at the entry to the Guyon’s canal. These measurements were taken in both upper limbs of all cases and controls following standard protocol [1]. The measurements were taken by linear-array transducer probes (5–12 MHz) by tracing the nerve boundary represented by the inner margin of the outer hyperechoic rim surrounding the hypoechogenic nerve [14] (Fig. 1).
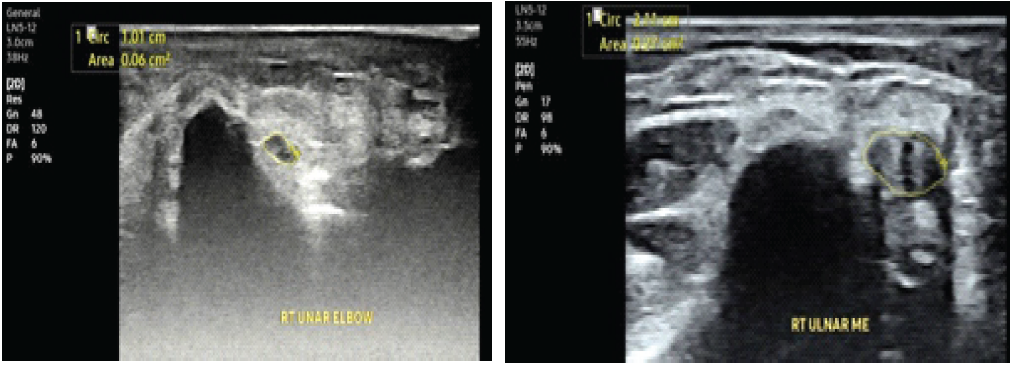
Figure 1: Ultrasound image of normal (upper image) versus thickened and hypoechoic ulnar nerve (lower image) at retro-condylar groove at the level of Medial Epicondyle.
Some indirect measurements of the ulnar nerve, the swelling ratio around the elbow, and the flattening ratio of the nerve were calculated in the following way [15]-
- Proximal swelling ratio at ME = CSAmax at ME/CSAmax at 5 cm proximal to ME
- Distal swelling ratio = CSAmax at ME/CSAmax at 5 cm distal to ME
- Flattening ratio CSAmax of ulnar nerve/CSAmin of ulnar nerve.
Statistical calculation
The data obtained from cases and controls were recorded in Microsoft Excel (Microsoft Corporation, Redmond, WA, USA) and were analyzed using Microsoft Excel 2024 and online software (MedCalc statistical software, 2025). Continuous variables were expressed as mean ± standard deviation, and categorical variables as n (%). Statistical significance was estimated using Student t-tests. P < 0.05 was considered to be statistically significant.
This study included 20 neuropathic limbs from 18 subjects, diagnosed by clinical features and electrodiagnostic parameters. The bilateral presentation of ulnar neuropathy was found in two patients; in others, the presentation was unilateral. Twenty healthy subjects, comparable to cases and without any features of ulnar neuropathy, were included as controls. The age range was 18 to 68 years in both cases and controls, with the majority falling within the 40–55-year age group. A total of 40 upper limbs without ulnar neuropathy were included in the control group. The ulnar neuropathy was more commonly seen in males. The professions were miscellaneous and comparable among cases and controls (Table 1).
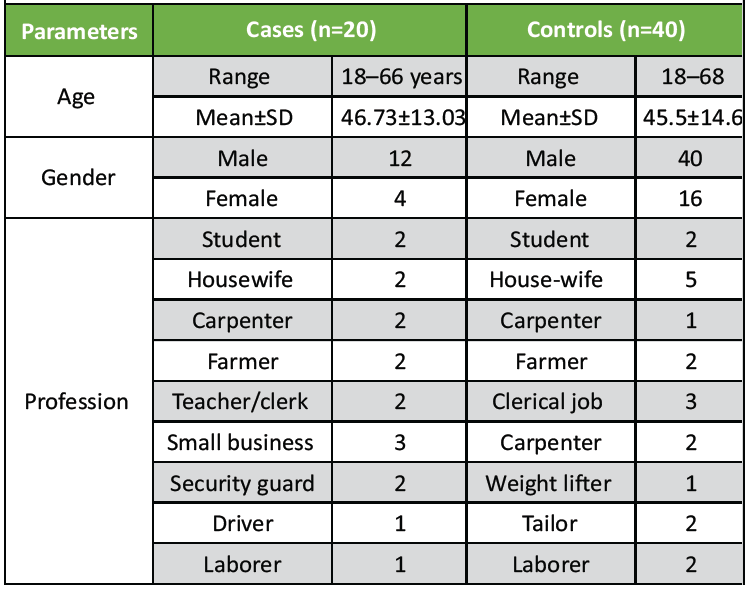
Table 1: Demographic details of cases and controls
The most standard presenting feature was weakness in grip (60%), followed by tingling-numbness and pain (50%). The 50% cases were traumatic in origin. In most cases, the US showed a bulky, hypo-echoic nerve (75%). In three cases, it showed post-traumatic neuroma, mostly around ME. In two cases, the dislocation of the nerve from the condylar groove was the cause of the symptoms (Table 2). In the majority of cases, the bulky and hypoechoic area of the ulnar nerve was noted at the level of ME (60%); however, the nerve enlargement was noted at mid-forearm in two cases; at wrist in two instances; enlargement of a nerve segment in two instances; and at proximal and distal to the ME in one case each (Table 2).
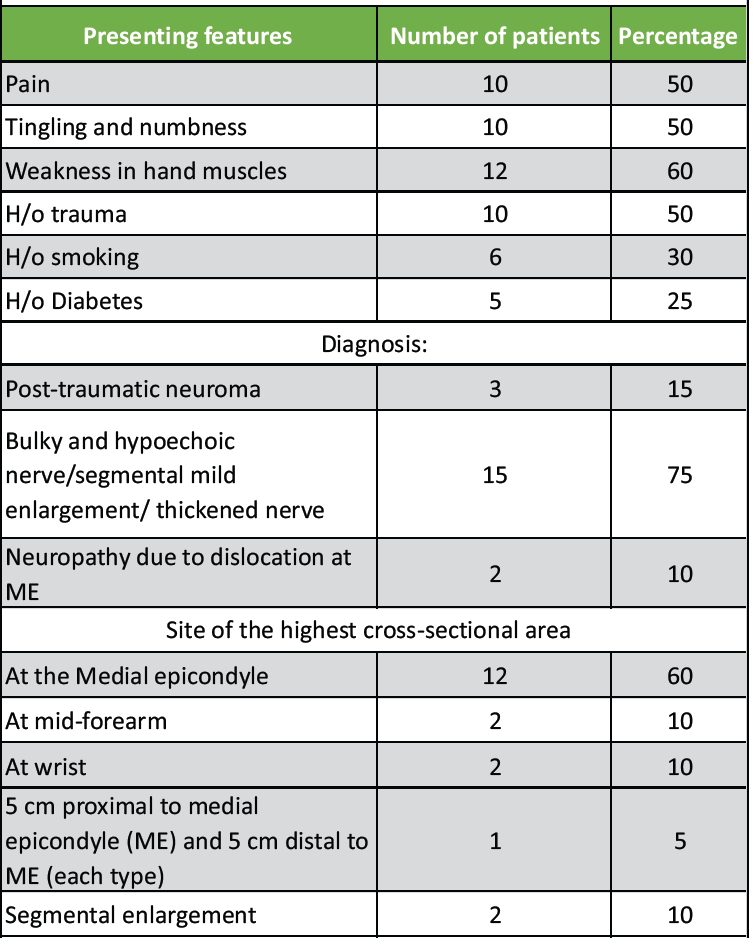
Table 2: Clinical features of cases (n=20)
It was seen that the mean diameter of the ulnar CSA in limbs diagnosed with ulnar neuropathy was 11.33 mm² at the elbow and 4.67 mm² at the wrist level. In control limbs, the measurements were 5.02 mm2 and 3.36 mm2, respectively. It was statistically significantly higher in cases of ulnar neuropathy than in the controls (P > 0.05). The ulnar CSA was measured at five predetermined places in diseased and control upper limbs (Fig. 2).
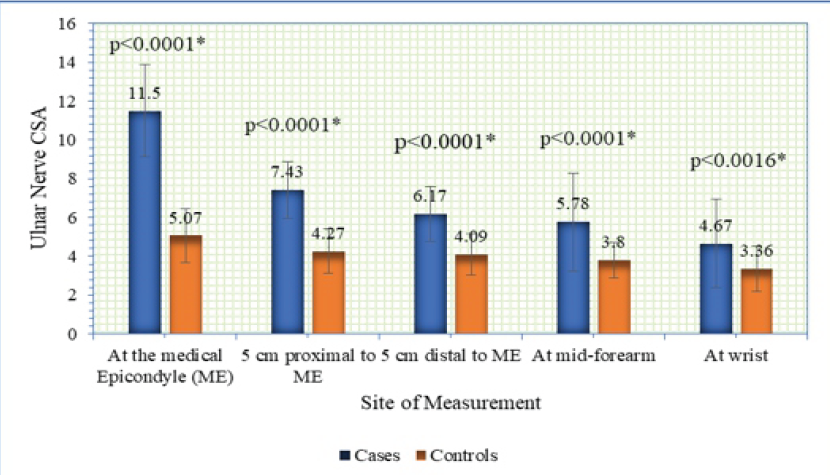
Figure 2: Comparison of cross-sectional area of the ulnar nerve at various labels among cases and controls.
The highest CSA along the course of an individual nerve was also calculated in the diseased upper limbs (n = 20) and the control upper limbs (n = 40). Among the cases and controls, the highest CSA of the ulnar nerve was observed at ME in the majority, followed by the mid-forearm and wrist. The healthy subjects’ CSA values were compared across genders (Fig. 3).
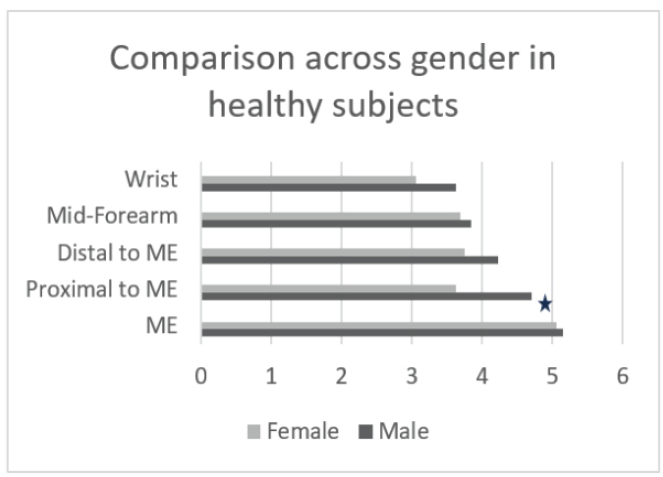
Figure 3: Comparison across gender: Cross-sectional area at various levels across controls.
All the values were higher among males, but statistical significance could not be observed in most values, except in the case of CSA at 5 cm proximal to the ME. Due to the minimal number of cases and an even smaller number of female patients, the values could not be compared across genders among ulnar neuropathy cases.
The indirect measurements of ulnar nerve CSA were done by calculating the swelling ratio around the ME and flattening ratio. The swelling ratios in cases were statistically significantly higher than those in controls. The flattening ratio was also statistically significantly higher among cases than controls (Table 3).
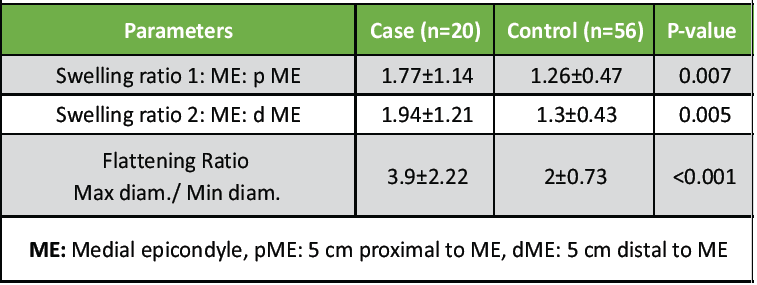
Table 3: Comparison of indirect parameters across cases and controls
This study presented the mean CSA values of the ulnar nerve obtained by US examination at multiple predetermined sites along the course of the ulnar nerve of both upper limbs. The values were collected in the ulnar neuropathy patients and an age- and gender-matched control population without any features of ulnar neuropathy.
Diverse causes of ulnar neuropathy have been mentioned, which include trauma, compression, arthritis, synovitis, abnormal musculoskeletal structures, ganglia or other mass lesions, use of repetitive tools, and often idiopathic causes [1,2,3,6,16]. Prolonged compression leads to ischemia and endoneural edema, an increase in perineural thickness, changes in myelination, and other effects, all of which contribute to focal enlargement [6,7,17]. This becomes evident in MRI or high-resolution US by measuring the nerve CSA.
Terayama et al. conducted a study where the same CSA was measured by both US and MRI, and no significant difference was observed among the procedures [9]. The US, being a non-invasive, brief, and low-cost investigation, is more commonly undertaken.
In the present study, the highest CSA was observed at the level of the ME in both diseased (cases) and healthy (control) upper limbs. The values were 11.5 ± 2.38 mm2 among cases and 5.07 ± 1.4 mm2 among controls. The lowest value was observed at the wrist level in both diseased and healthy upper limbs, with values of 4.67 ± 2.3 mm² and 3.36 ± 1.15 mm², respectively. All the values were statistically significantly higher in cases than controls at all five measurement locations.
Similar findings were observed in most previous research [5,7,18]; however, the mean values differed across various studies (Table 4). The CSA value was highest at the level of ME in the present study; in previous studies, the highest CSA was found at the same level and the value were higher that 10 mm2 in all cases of ulnar neuropathy; in two instances the mean value was higher than the present study [7,18], and in one study, the mean value was lower than the present study [5]- all values were close to each other (Table 4).
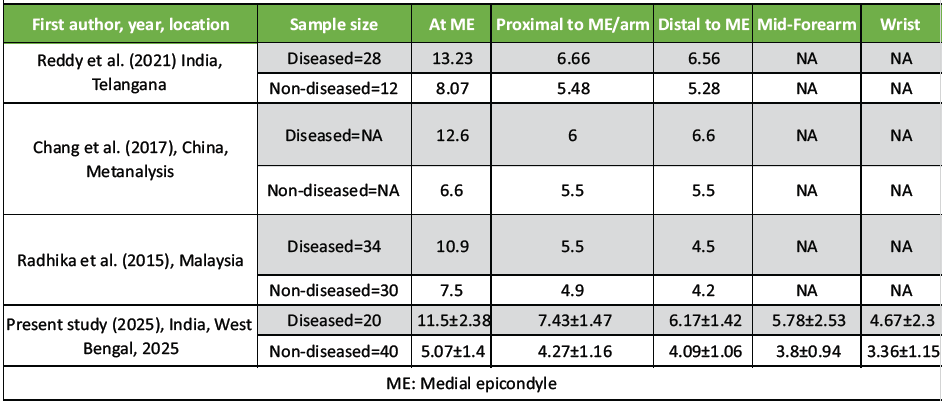
Table 4: Comparison of the parameters across various studies
The normative values of ulnar nerve CSA around ME differ across the various populations in healthy subjects, with generally higher values for the Australian, Canadian, and European populations than the South Asian population; however, it varies among the Asian population as well [5,13,15,19,20,21,22,23]. The ulnar nerve CSA values at the wrist are very limited in the literature. Bathala et al. [11] reported ulnar CSA 3.6 ± 0.49 mm2 in healthy subjects, which is very close to our study – 3.36 ± 1.15 mm2.
Although differences in ethnicity, age, and BMI across various populations could be the probable causes of differences in ulnar CSA values, other factors, such as the non-uniformity of the measurement sites, non-uniformity of measurement postures of the patient, and use of different US probes, might have also contributed to these other values. The proximal to ME measurement site varied from 1 cm to 5 cm proximal to ME [5,9]; flexed versus extended forearms were used in some studies [24]; US probes ranging from 3 to 18 MHz [5,7,14] were used in various studies.
Based on the CSA values obtained by healthy subjects, most researchers suggested a cut-off value of 10 mm2 to diagnose ulnar neuropathy cases; however, 7.5 mm2 was suggested by Chiou et al., 9.27 mm2 was suggested by Radhika et al., and 11 mm2 was suggested by Terayama et al. [5,9,25]. Volpe et al. suggested grading the severity of ulnar neuropathy based on CSA values; however, Reddy et al. denied the correlation between the severity of ulnar neuropathy and ulnar CSA values in their study population [5,23]. Uniformity in the procedure is essential to determine the specific cut-off values across the population. From the present study, it is recommended that the ulnar CSA measuring >7.5 mm2 at ME and >4.5 mm2 at the wrist in the extended upper limb and elbow, as the cut-off value to diagnose the ulnar neuropathy in symptomatic patients using 5–12 MHz US probes.
In the present study, the swelling and flattening ratios were statistically significantly higher in cases than controls, which has been consistent with a previous study [15]. The swelling ratio >1.5 and flattening ratio >3.5 might be considered for diagnosing ulnar neuropathy in symptomatic patients.
In the present study, most cases (90%) were seen in the age range of 40–55 years. Therefore, healthy subjects of a similar age group were compared, and no age-related alteration of nerve CSA could be appreciated. In some previous studies, higher ulnar CSA was observed in the increasing age group [10,22]. In contrast, another researcher found a negative correlation between ulnar CSA in the cubital tunnel and increasing age [13]. In the present study, a higher prevalence of ulnar neuropathy was observed in males, consistent with some studies [3,26]. Although a higher prevalence of ulnar neuropathy is supposed to be seen in a specific professional group, that is, cyclists, laborers, etc., who repeatedly use the same hand tools [1], the present study observed this condition in different professions, including homemakers and retired personnel.
The most familiar presenting complaint was weakness or difficulty in grip (60%), followed by tingling-numbness-pain (50%). Some previous studies were consistent with this finding [26] while others reported predominant sensory symptoms [27].
In the present study, we found 10% cases with dislocation of the ulnar nerve at the ulnar groove; similarly, this ulnar instability has been considered an essential factor for ulnar neuropathy in a previous study [28]. In the present study, segmental nerve enlargement was noted in two cases, which was also reported in an earlier study [29].
Limitation
The primary limitation of this pilot study is the small number of cases and a single-center-based population. Another limitation is the lack of longitudinal follow-up, as this is a cross-sectional study. The ulnar CSA was not compared to age, BMI, or other factors. Still, this is the first study of this kind in West Bengal, and further studies based on this data might help in the diagnosis and treatment planning of ulnar neuropathy patients in this region.
The present study provided a normative data set of the Ulnar nerve CSA at five predetermined anatomical locations along the course of the ulnar nerve. It offered a set of values for the ulnar neuropathy patients as well. It recommends a cut-off value of > 7.5 mm2 at the level of the ME of the elbow, along with a swelling ratio >1.5 and a flattening ratio >3.5 for the diagnosis of ulnar peripheral neuropathy at the elbow among the symptomatic patients in the population of Eastern India.
The present study provides a baseline Ultrasound dataset for the ulnar nerve CSA for healthy subjects and recommends a cut-off value for diagnosing ulnar entrapment neuropathy for the population of West Bengal.
References
- 1. 1 Preston DC, Shapiro BE. Clinical Disorders. Electromyography and Neuromuscular Disorders: Clinical-Electrophysiologic-Ultrasound Correlations. 4th ed. Amsterdam: Elsevier; 2021. p. 372-3. [Google Scholar] [PubMed]
- 2. 2 Landau ME, Campbell WW. Clinical features and electrodiagnosis of ulnar neuropathies. Phys Med Rehabil Clin N Am 2013;24:49-66. [Google Scholar] [PubMed]
- 3. 3 Pelosi L, Tse DM, Mulroy E, Chancellor AM, Boland MR. Ulnar neuropathy with abnormal non-localizing electrophysiology: Clinical, electrophysiological, and ultrasound findings. Clin Neurophysiol 2018;129:2155-61. [Google Scholar] [PubMed]
- 4. 4 Cha SM, Shin HD. Features of the ulnar nerve predicting postoperative prognosis in idiopathic cubital tunnel syndrome: Three distinct features of the ulnar nerve. Ann Plast Surg 2020;85:50-5. [Google Scholar] [PubMed]
- 5. 5 Radhika S, Lee YL, Low SF, Fazalina MF, Sharifah Majedah IA, et al. Role of high resolution ultrasound in ulnar nerve neuropathy. Med J Malaysia 2015;70:158-61. [Google Scholar] [PubMed]
- 6. 6 Schmid AB, Fundaun J, Tampin B. Entrapment neuropathies: A contemporary approach to pathophysiology, clinical assessment, and management. Pain Rep 2020;5:e829. [Google Scholar] [PubMed]
- 7. Reddy YM, Murthy JM, Suresh L, Jaiswal SK, Pidaparthi L, Kiran ES. Diagnosis and severity evaluation of ulnar neuropathy at the elbow by ultrasonography: A Case-control study. J Med Ultrasound 2022;30:189-95. [Google Scholar] [PubMed]
- 8. Kurihara Y, Hanayama K, Furukawa T, Masakado Y, Toyokura M. Relationship between clinical severity and cross-sectional area of ultrasonographic examinations in ulnar neuropathy at the elbow. Prog Rehabil Med 2023;8:23-25. [Google Scholar] [PubMed]
- 9. .Terayama Y, Uchiyama S, Ueda K, Iwakura N, Ikegami S, Kato Y, et al. Optimal measurement level and ulnar nerve cross-sectional area cutoff threshold for identifying ulnar neuropathy at the elbow by MRI and ultrasonography. J Hand Surg Am 2018;43:529-36. [Google Scholar] [PubMed]
- 10. Cartwright MS, Mayans DR, Gillson NA, Griffin LP, Walker FO. Nerve cross-sectional area in extremes of age. Muscle Nerve 2013;47:890-893. [Google Scholar] [PubMed]
- 11. Bathala L, Kumar P, Kumar K, Visser LH. Ultrasonographic cross-sectional area normal values of the ulnar nerve along its course in the arm with electrophysiological correlations in 100 Asian subjects. Muscle Nerve 2013;47:673-6. [Google Scholar] [PubMed]
- 12. Boers N, Martin E, Mazur M, Krijgh DD, Vlak MH, Ruiter GC, et al. Sonographic normal values for the cross-sectional area of the ulnar nerve: A systematic review and meta-analysis. J Ultrasound 2023;26:81-8. [Google Scholar] [PubMed]
- 13. Hsieh PC, Chang KH, Wu YR, Ro LS, Chu CC, Lyu RK, et al. Cross-sectional area reference values for sonography of peripheral nerves in Taiwanese adults. Front Neurol 2021;12:722403. [Google Scholar] [PubMed]
- 14. Fisse AL, Katsanos AH, Gold R, Pitarokoili K, Krogias C. Cross-sectional area reference values for peripheral nerve ultrasound in adults: A systematic review and meta-analysis-part I: Upper extremity nerves. Eur J Neurol 2021;28:1684-91. [Google Scholar] [PubMed]
- 15. Chen IJ, Chang KV, Wu WT, Ozcakar L. Ultrasound parameters other than the direct measurement of ulnar nerve size for diagnosing cubital tunnel syndrome: A systemic review and meta-analysis. Arch Phys Med Rehabil 2019;100:1114-30. [Google Scholar] [PubMed]
- 16. Murata K, Shih JT, Tsai TM. Causes of ulnar tunnel syndrome: A retrospective study of 31 subjects. J Hand Surg 2003;28:647-51. [Google Scholar] [PubMed]
- 17. Thoirs K, Scutter S, Wilkinson M. The ulnar nerve at the elbow: An anatomic, sonographic, and histologic comparison. J Diagn Med Sonogr 2003;19:16-23. [Google Scholar] [PubMed]
- 18. Chang KV, Wu WT, Han DS, Ozcakar L. Ulnar nerve cross-sectional area for diagnosing cubital tunnel syndrome: A meta-analysis of ultrasonographic measurements. Arch Phys Med Rehabil 2018;99:743-57. [Google Scholar] [PubMed]
- 19. Letissier H, Dardenne G, Saraux A, Le Nen D, Borotikar B, Jousse-Joulin S. Ultrasound ulnar nerve measurement in a healthy population. Rheumatol Ther 2021;8:457-66. [Google Scholar] [PubMed]
- 20. Niu J, Li Y, Zhang L, Ding Q, Cui L, Liu M. Cross-sectional area reference values for sonography of nerves in the upper extremities. Muscle Nerve 2020;61:338-46. [Google Scholar] [PubMed]
- 21. Qrimli M, Ebadi H, Breiner A, Siddiqui H, Alabdali M, Abraham A, et al. Reference values for ultrasonograpy of peripheral nerves. Muscle Nerve 2016;5:538-44. [Google Scholar] [PubMed]
- 22. Sugimoto T, Ochi K, Hosomi N, Mukai T, Ueno H, Takahashi T, et al. Ultrasonographic reference sizes of the median and ulnar nerves and the cervical nerve roots in healthy Japanese adults. Ultrasound Med Biol 2013;39:1560-70. [Google Scholar] [PubMed]
- 23. Volpe A, Rossato G, Bottanelli M, Marchetta A, Caramaschi P, Bambara LM, et al. Ultrasound evaluation of ulnar neuropathy at the elbow: Correlation with electrophysiological studies. Rheumatology (Oxford) 2009;48:1098-101. [Google Scholar] [PubMed]
- 24. Prasetyo M, Rahardja RR, Yanuar A, Prihartono J, Setiawan SI. Ultrasonography evaluation of the normal ulnar nerve in adults: Comparison of the cross-sectional area at elbow extension and flexion. Eur J Radiol Open 2021;8:100331. [Google Scholar] [PubMed]
- 25. Chiou HJ, Chou YH, Cheng SP, Hsu CC, Chan RC, Tiu CM, et al. Cubital tunnel syndrome: Diagnosis by high‐resolution ultrasonography. J Ultrasound Med 1998;17:643-8. [Google Scholar] [PubMed]
- 26. Batool M, Bano S, Shamim F, Numan A. Frequency of ulnar neuropathy, etiologies and electrodiagnostic correlation with clinical severity. J Pak Soc Intern Med 2023;4:130-4. [Google Scholar] [PubMed]
- 27. Yadav RL. A retrospective study of electrodiagnostically evaluated ulnar neuropathies with special guidelines for ulnar neuropathies at the elbow. Beni-Suef Univ J Basic Appl Sci 2022;11:31. [Google Scholar] [PubMed]
- 28. Ahamadli N, Akgun K, Terlemez R, Misirlioglu TO, Palamer D. Ultrasonographic evaluation of ulnar nerve morphology in patients with ulnar nerve instability. Muscle Nerve 2042;69:543-7. [Google Scholar] [PubMed]
- 29. Podnar S. Length of affected nerve segment in ulnar neuropathies at the elbow. Clin Neurophysiol 2022;133:104-10. [Google Scholar] [PubMed]









