Minimally invasive spinopelvic posterior fixation and an internal anterior fixator is effective for the treatment of stabilization of pelvic fractures in patients with diffuse idiopathic skeletal hyperostosis, especially in patients who are in poor general health.
Dr. Takeshi Sasagawa, Department of Orthopedics Surgery, Toyama Prefectural Central Hospital, Toyama City, Japan. E-mail: sasagawawagasasa@yahoo.co.jp
Introduction: Spinal fractures related to diffuse idiopathic skeletal hyperostosis (DISH) are almost always caused by a long lever arm, so treatment of the fractures requires stabilization of long segments of the spine. Treatment of unstable sacral fractures in DISH patients with ankylosis of the sacroiliac joints requires a treatment strategy that includes a consideration of the condition of the spine. This article is the first report of an unstable sacral fracture in a patient with DISH.
Case Report: A 95-year-old male fell and presented with severe low back pain. An X-ray and computed tomography showed unstable pelvic fracture (AO type C2) and ankylosis of the lumbar spine due to DISH. We performed minimally invasive spinopelvic posterior fixation and internal anterior fixation (INFIX) for stabilization of the pelvic fracture. Initially, due to the long lever arm created from the lumbar spine to the pelvis, we performed L2-iliac posterior stabilization while the patient was in a prone position. After that, we performed INFIX to stabilize the anterior pelvis while the patient was positioned supine. The postoperative clinical course of the patient was uneventful and bony fusion was achieved as seen on X-ray obtained 1 year postoperatively.
Conclusion: This patient was ankylosed from spine to pelvis due to DISH and sacroiliac joint ankylosis and sustained bilateral sacral fractures which dissociated the sacrum from the rest of the pelvis. Therefore, this fracture required spinopelvic fixation from the ankylosing spine to the pelvis. Because this patient was so elderly and in poor general health, we performed minimally invasive spinopelvic posterior fixation using percutaneous pedicle screws. We considered that many screw insertions that would equivalently stabilize the spine several segments above and below the fracture would be needed to stabilize the sacral fractures in this patient with DISH. In this case, we stabilized the unstable right pelvis, in a patient with a stable left side, using INFIX. Although osteoporosis is frequently associated with DISH, bony fusion was achieved in this case. This demonstrates that this procedure is sufficient fixation for an unstable sacral fracture in patients with DISH.
Keywords: Unstable sacral fracture, diffuse idiopathic skeletal hyperostosis, minimally invasive spinopelvic posterior fixation, an internal anterior fixator.
Unstable sacral fractures are severe injuries with high mortality and morbidity [1]. Although hospital records show mortality after high-energy pelvic fractures in elderly patients is higher than that in younger adults, mortality within the 1st year after discharge is low and does not differ between groups [2]. Thus, it is important to stabilize the unstable pelvis to control damage and facilitate nursing care during the acute phase of healing, especially in elderly patients. Therefore, unstable pelvic fractures in elderly patients require minimally invasive surgery, especially when the patient is in poor general condition.
Spinal fractures in patients with diffuse idiopathic skeletal hyperostosis (DISH) are not uncommon. Spinal fractures related to DISH are almost always caused by a long lever arm, so treatment of the fractures requires stabilization of long segments of the spine [3,4,5]. The frequency of ankylosis of the sacroiliac joints of patients with DISH is higher compared with non-DISH patients [6]. Treatment of unstable sacral fractures in DISH patients with ankylosis of the sacroiliac joints requires a treatment strategy that includes a consideration of the condition of the spine. This article is the first report of an unstable sacral fracture in a patient with DISH.
A 95-year-old male fell from the 2nd floor and presented with severe low back pain. An X-ray showed a pelvic fracture and ankylosis of the lumbar spine due to DISH (Fig. 1a, b). Computed tomography (CT) showed an unstable pelvic injury (AO type C2) with unstable sacral and pubic fractures on the right side, a stable sacral fracture on the left side, and bilateral ankylosis of the sacroiliac joints (Fig. 1c). 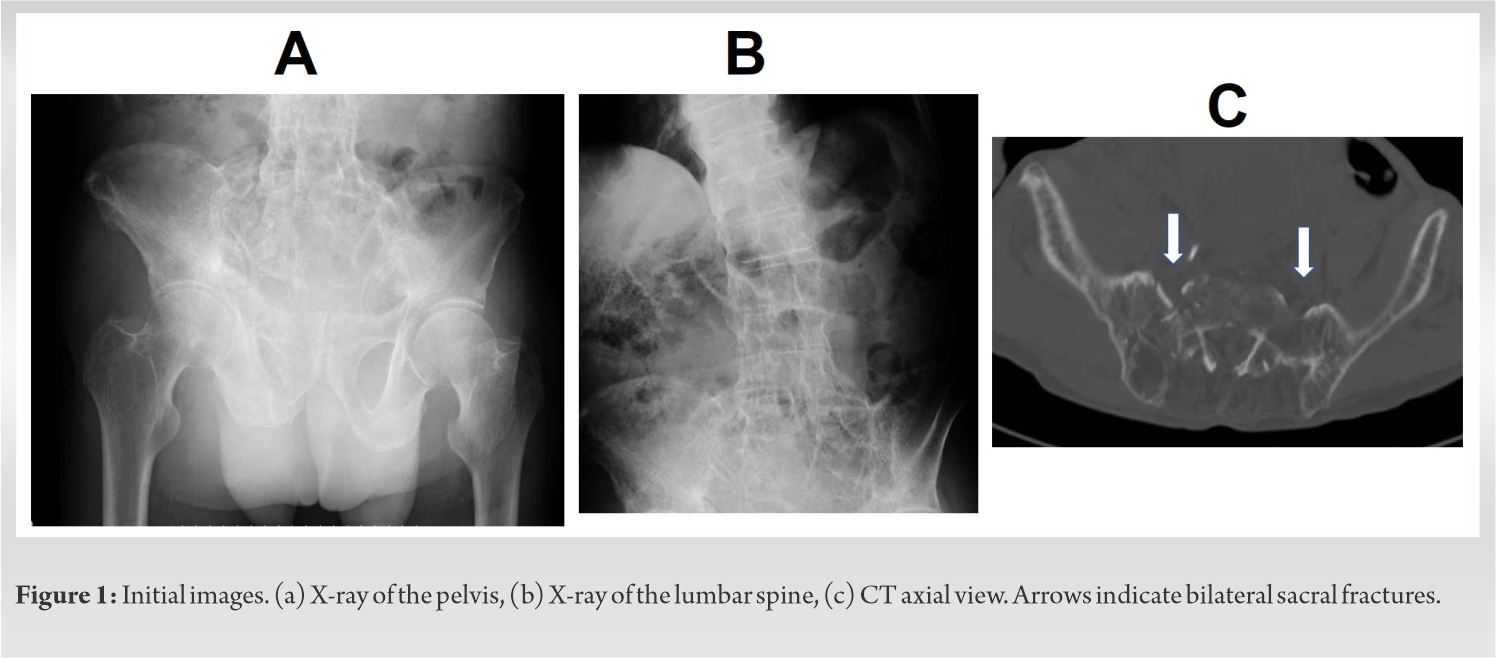 This patient also sustained a cerebral subarachnoid haemorrhage accompanied by a moderate consciousness disorder. Because of hypovolemic shock due to active bleeding from the common iliac arteries bilaterally, as detected on contrast-enhanced CT, and an unstable fracture, transcatheter arterial embolization, and external fixation of the pelvis were performed on the day of the injury (Fig. 2).
This patient also sustained a cerebral subarachnoid haemorrhage accompanied by a moderate consciousness disorder. Because of hypovolemic shock due to active bleeding from the common iliac arteries bilaterally, as detected on contrast-enhanced CT, and an unstable fracture, transcatheter arterial embolization, and external fixation of the pelvis were performed on the day of the injury (Fig. 2).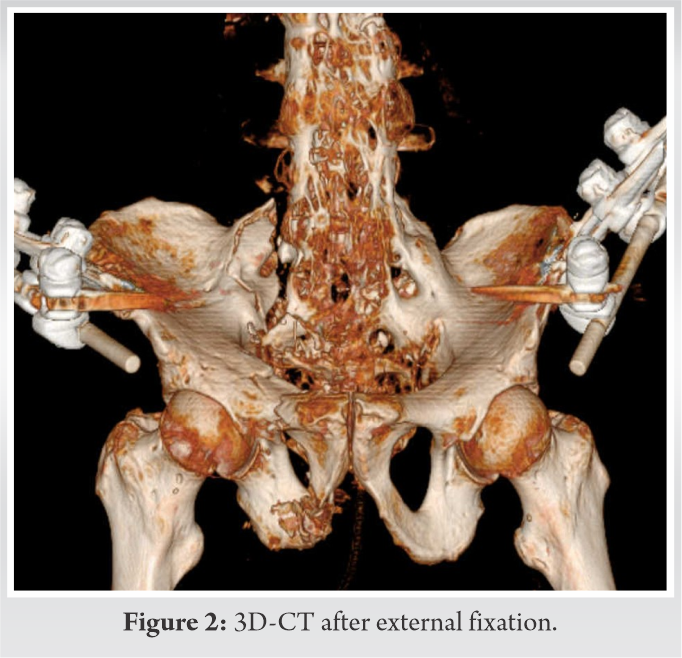
Eight days later, we performed minimally invasive spinopelvic posterior fixation and internal anterior fixation (INFIX) for stabilization of the pelvic fracture. Initially, due to the long lever arm created from the lumbar spine to the pelvis, we performed L2-iliac posterior stabilization while the patient was in a prone position. Once percutaneous pedicle screws (PPS) (6 × 50 mm) were inserted from L2 to L4 through 6 small incisions, and 2 iliac screws (7 × 50 mm cranially, 7.5 × 80 mm caudally) were inserted bilaterally through bilateral 5 cm skin incisions, we connected the screws using 5.5 mm titanium rods into the paravertebral muscles. After that, we performed INFIX to stabilize the anterior pelvis while the patient was positioned supine. A longitudinal 5 cm incision was made centred over the anterior inferior iliac spine. Care was taken to protect the lateral femoral cutaneous nerve, which was retracted laterally. Polyaxial screws (7.5 × 80 mm) were introduced along a path between the anterior inferior iliac spine and the ipsilateral posterior superior iliac spine. Once screws were inserted, 5.5 mm titanium rods were cut and shaped, considering the size and abdominal shape of the patient so as not to compress abdominal organs (Fig. 3).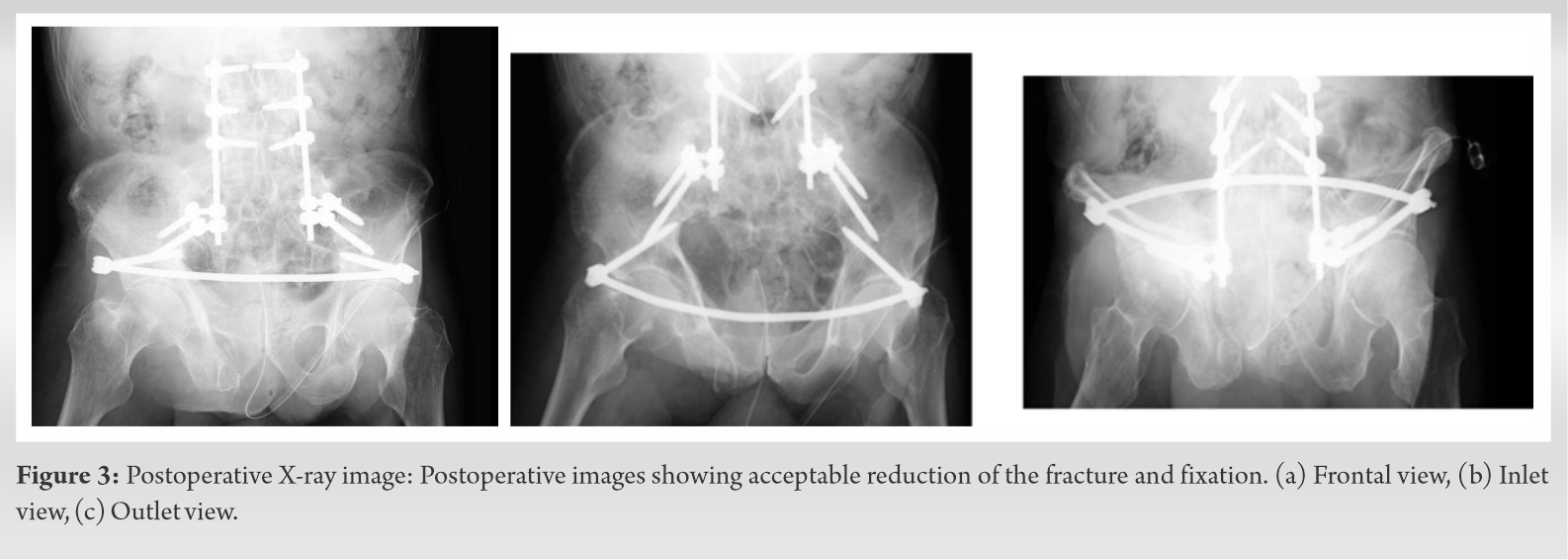 The estimated surgical time from posterior and anterior surgeries was 147 min and 49 min, respectively. Blood loss from posterior and anterior surgeries was 268 g and 150 g, respectively. The postoperative clinical course of the patient was uneventful and bony fusion was achieved as seen on X-ray obtained 1 year postoperatively even without any medical treatment for osteoporosis (Fig. 4).
The estimated surgical time from posterior and anterior surgeries was 147 min and 49 min, respectively. Blood loss from posterior and anterior surgeries was 268 g and 150 g, respectively. The postoperative clinical course of the patient was uneventful and bony fusion was achieved as seen on X-ray obtained 1 year postoperatively even without any medical treatment for osteoporosis (Fig. 4).  However, because of consciousness disorder and muscle weakness of the lower limb (Manual Muscle Test 2) due to disuse syndrome, the patient was bedridden without a limitation in range of movement of the bilateral hip joint for up to 2 years postoperatively. We considered implant removal after bony fusion was achieved. However, the patient and his family did not want the surgery under general anaesthesia because he was elderly and there were no serious complications such as lateral femoral cutaneous nerve irritation or improper placement of the rod.
However, because of consciousness disorder and muscle weakness of the lower limb (Manual Muscle Test 2) due to disuse syndrome, the patient was bedridden without a limitation in range of movement of the bilateral hip joint for up to 2 years postoperatively. We considered implant removal after bony fusion was achieved. However, the patient and his family did not want the surgery under general anaesthesia because he was elderly and there were no serious complications such as lateral femoral cutaneous nerve irritation or improper placement of the rod.
This patient was ankylosed from spine to pelvis due to DISH and sacroiliac joint ankylosis and sustained bilateral sacral fractures which dissociated the sacrum from the rest of the pelvis. Therefore, this fracture required spinopelvic fixation from the ankylosing spine to the pelvis [7]. Recently minimally invasive spinopelvic posterior fixation using PPS for sacral fractures was developed, and good clinical results were reported [1]. Because this patient was so elderly and in poor general health, we performed minimally invasive spinopelvic posterior fixation using PPS. Spinal fractures related to DISH are almost always the result of a long lever arm so neutralization of fractures requires stabilization of long segments of the spine [3,4,5]. Reports suggest that fusing three segments above and below the fracture is a reliable range of fusion for spinal fractures with DISH [3]. Similarly, for this case, we considered that many screw insertions that would equivalently stabilize the spine several segments above and below the fracture would be needed to stabilize the sacral fractures in this patient with DISH. Minimally invasive spinopelvic posterior fixation can be placed many pedicle screws in the spine, but only two screws can be placed bilaterally in the pelvis. Because of this limitation of screw insertion to the pelvis with posterior spinopelvic fixation, we added anterior pelvic fixation in this case. Recently INFIX was developed, and good clinical results have been reported as support for posterior fixation [8,9,10]. In this case, we stabilized the unstable right pelvis, in a patient with a stable left side, using INFIX. Although osteoporosis is frequently associated with DISH [3], bony fusion was achieved even without any medical treatment for osteoporosis in this case. This demonstrates that this procedure is sufficient fixation for an unstable sacral fracture in patients with DISH. Although cement augmented screw is one option for better purchase of screws in osteoporotic bone, this case report demonstrates that many screw insertions even without cement augmentation that would equivalently stabilize the spine several segments above and below the fracture would be reliable to stabilize the sacral fractures in this patient with DISH.
Because closed reduction is used in this procedure, a strict reduction of the fracture cannot be achieved as it can with plate fixation, which requires open reduction [11,12]. Because the type C fracture reduced by closed reduction can become a symptomatic malunion [13,14,15,16], such cases ideally should be treated by open reduction. However, although plate fixation for pelvic ring fractures achieves an anatomic reduction of fractures under direct vision, it requires major open surgery. Because this patient was very elderly and in poor general health, a spinopelvic fixation using a minimally invasive procedure was given priority over strict reduction. Because the surgery was minimally invasive, the postoperative clinical course of the patient was uneventful.
We conclude that minimally invasive spinopelvic posterior fixation and INFIX is effective for the treatment of stabilization of pelvic fractures in patients with DISH, especially in patients who are in poor general health.
Treatment of unstable sacral fractures in DISH patients with ankylosis of the sacroiliac joints requires a treatment strategy that includes a consideration of the condition of the spine. This article is the first report of an unstable sacral fracture in a patient with DISH. Minimally invasive spinopelvic posterior fixation and INFIX is effective for the treatment of stabilization of pelvic fractures in patients with DISH, especially in patients who are in poor general health.
References
- 1.Koshimune K, Ito Y, Sugimoto Y, Kikuchi T, Morita T, Mizuno S, et al. Minimally invasive spinopelvic fixation for unstable bilateral sacral fractures. Clin Spine Surg 2016;29:124-7. [Google Scholar | PubMed]
- 2.Keil DS, Gross S, Seymour RB, Sims S, Karunakar MA. Mortality after high-energy pelvic fractures in patients of age 65 years or older. J Orthop Trauma 2018;32:124-8. [Google Scholar | PubMed]
- 3.Caron T, Bransford R, Nguyen Q, Agel J, Chapman J, Bellabarba C. Spine fractures in patients with ankylosing spinal disorders. Spine (Phila Pa 1976) 2010;35:e458-64. [Google Scholar | PubMed]
- 4.Robinson Y, Robinson AL, Olerud C. Complications and survival after long posterior instrumentation of cervical and cervicothoracic fractures related to ankylosing spondylitis or diffuse idiopathic skeletal hyperostosis. Spine (Phila Pa 1976) 2015;40:e227-33. [Google Scholar | PubMed]
- 5.Lindtner RA, Kammerlander C, Goetzen M, Keiler A, Malekzadeh D, Krappinger D, et al. Fracture reduction by postoperative mobilization for the treatment of hyperextension injuries of the thoracolumbar spine in patients with ankylosing spinal disorders. Arch Orthop Trauma Surg 2017;137:531-41. [Google Scholar | PubMed]
- 6.Leibushor N, Slonimsky E, Aharoni D, Lidar M, Eshed I. CT abnormalities in the sacroiliac joints of patients with diffuse idiopathic skeletal hyperostosis. AJR Am J Roentgenol 2017;208:834-7. [Google Scholar | PubMed]
- 7.Bederman SS, Hassan JM, Shah KN, Kiester PD, Bhatia NN, Zamorano DP. Fixation techniques for complex traumatic transverse sacral fractures: A systematic review. Spine (Phila Pa 1976) 2013;38:E1028-40. [Google Scholar | PubMed]
- 8.Dahill M, McArthur J, Roberts GL, Acharya MR, Ward AJ, Chesser TJ. The use of an anterior pelvic internal fixator to treat disruptions of the anterior pelvic ring: A report of technique, indications and complications. Bone Joint J 2017;99:1232-6. [Google Scholar | PubMed]
- 9.Vigdorchik JM, Esquivel AO, Jin X, Yang KH, Onwudiwe NA, Vaidya R. Biomechanical stability of a supra-acetabular pedicle screw internal fixation device (INFIX) vs external fixation and plates for vertically unstable pelvic fractures. J Orthop Surg Res 2012;7:31. [Google Scholar | PubMed]
- 10.Vaidya R, Colen R, Vigdorchik J, Tonnos F, Sethi A. Treatment of unstable pelvic ring injuries with an internal anterior fixator and posterior fixation: Initial clinical series. J Orthop Trauma 2012;26:1-8. [Google Scholar | PubMed]
- 11.Yin Y, Luo J, Zhang R, Li S, Jiao Z, Zhang Y, et al. Anterior subcutaneous internal fixator (INFIX) versus plate fixation for pelvic anterior ring fracture. Sci Rep 2019;9:2578. [Google Scholar | PubMed]
- 12.Tsuji H, Takigawa T, Misawa H, Shiozaki Y, Yamakawa Y, Noda T, et al. Minimally invasive percutaneous spinopelvic fixation for unstable pelvic ring fracture performed with the patient in a lateral position. Clin Spine Surg 2019;32:191-7. [Google Scholar | PubMed]
- 13.Lindahl J, Hirvensalo E, Böstman O, Santavirta S. Failure of reduction with an external fixator in the management of injuries of the pelvic ring. Long-term evaluation of 110 patients. J Bone Joint Surg Br 1999;81:955-62. [Google Scholar | PubMed]
- 14.Lee KJ, Min BW, Oh GM, Lee SW. Surgical correction of pelvic malunion and nonunion. Clin Orthop Surg 2015;7:396-401. [Google Scholar | PubMed]
- 15.Vanderschot P, Daenens K, Broos P. Surgical treatment of post-traumatic pelvic deformities. Injury 1998;29:19-22. [Google Scholar | PubMed]
- 16.Matta JM, Dickson KF, Markovich GD. Surgical treatment of pelvic nonunions and malunions. Clin Orthop Relat Res 1996;329:199-206. [Google Scholar | PubMed]





