Early recognition and intervention are needed with preoperation templating for successful outcomes in cases with complex injuries.
Dr. Hind Alraeh, Department of Orthopedic Surgery, Aseer Central Hospital, Abha, Saudi Arabia. E-mail: hind.raeh@hotmail.com
Introduction:High-energy trauma has increased the incidence of traumatic hip dislocation. In most cases, dislocation of the hip is associated with fractures of the acetabulum. However, its association with ipsilateral intertrochanteric fracture is very rare.
Case Report:We present a case of a 54-year-old male who had uncommon fracture pattern involving ipsilateral intertrochanteric femur fracture associated with ipsilateral posterior fracture dislocation of hip following a road traffic accident. He underwent closed reduction of the dislocation followed by an open reduction and internal fixation of the fractures. Through Kocher-Langenbeck approach, the intertrochanteric fracture was reduced and fixed with dynamic hip screw and derotation anti-rotation screw. Acetabulum fractures then fixed after reduction with two reconstruction plates.
Conclusion:Early recognition and orthopedic intervention constitute the cornerstones of satisfactory outcomes in cases with such complex injuries.
Keywords:Posterior hip dislocation, acetabular fractures, intertrochanteric fracture.
The anatomic features of hip joint imply a high degree of stability due to its ball and socket architecture and tight ligamentous and muscular structures type [1]. Dislocation of the hip is usually caused by high-energy trauma such as high-speed car crashes, falls from heights, and extreme sporting events [2]. The direction of the dislocation is dependent on the position of the hip, vectors, and intensity of the forces at the moment of impact [3]. The combination between traumatic posterior hip dislocations with ipsilateral intertrochanteric femur fracture is extremely rare. In medical literature, similar cases are rarely reported [4, 5, 6, 7].
The aim of the current paper is to report our experience with successful management of this rare presentation and briefly review the relevant literature and treatment options.
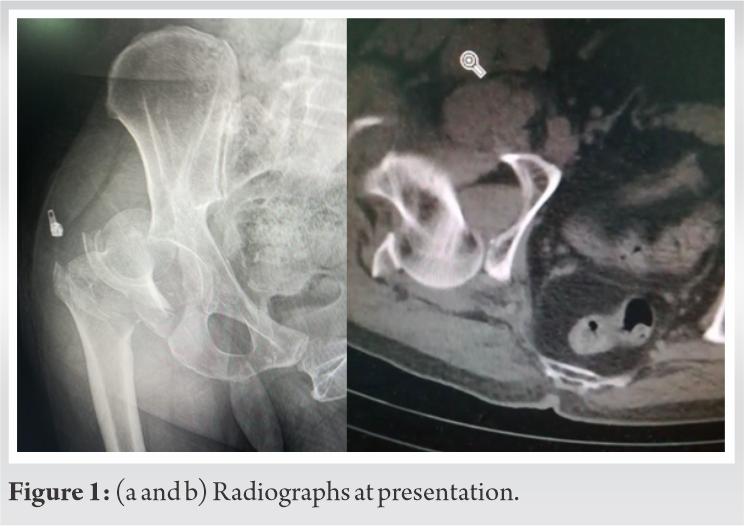
A 54-year-old male was admitted to our hospital in October 2019 after a road traffic accident. On admission, he was conscious (Glasgow Coma Scale = 15) and hemodynamically stable. He had severe pain in the right knee and was unable to move his right leg. On examination, his right leg was 2 cm shortened and rotated internally. Skin overlying the right patella had an open wound. Vascular and neurological examinations were normal. Examination of other limbs showed no injury. After primary stabilization of the patient as per advance trauma life support protocol, trauma series radiographs that were obtained showed right posterior hip dislocation and intertrochanteric with acetabulum fractures (Fig. 1). There were no further skeletal, spinal, or visceral injuries identified on secondary and tertiary surveys, focused assessment with sonography for trauma and computed tomography scans.
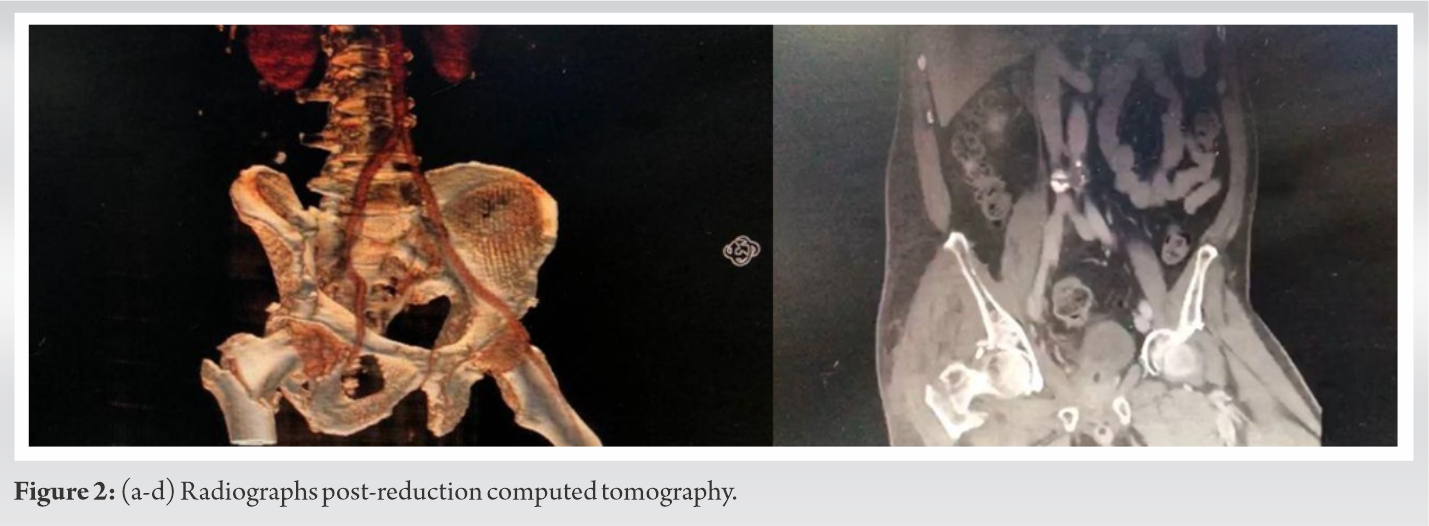
Immediately after resuscitation, the right hip dislocation was reduced in the emergency department with axial traction and gentle manipulation. Reduction was maintained with skin traction. Repeated post-reduction images (Fig. 2-4) showed no intra-articular fragments or loose bodies in the hip joint.
He was taken to the OR the next day. On the orthopedic table in lateral position with Kocher-Langenbeck approach, the intertrochanteric fracture was reduced and fixed with dynamic hip screw and derotation anti-rotation screw using C-arm imaging.
The procedure done through one approach. Acetabulum fractures fixation addressed after fractures reduction, then fixed with two reconstruction plates (Fig. 3). No drain was used postoperatively. Injuries of the knee were treated by debridement and primary closure.
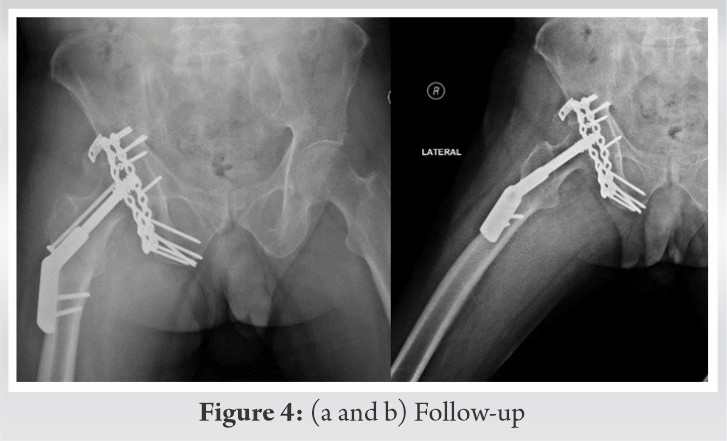
Postoperatively, the patient started inpatient physiotherapy immediately after surgery, then, he was discharged to complete a planned outpatient physiotherapy. That is, hip joint mobilization exercises were started at 3 weeks after surgery and walking without weight-bearing on the left lower limb was followed at 6 weeks after surgery. Progressive weight-bearing of the injured limb is allowed at 3 months after surgery (Fig. 4).
At the end of 1 year, the patient had painless hip with full range of motion. No radiological signs of avascular necrosis have been seen by the end of 1 year.
Road traffic accident is the leading cause of traumatic hip dislocation. Furthermore, posterior hip dislocation is reported more frequent than the anterior type [3]. Majority of patients with traumatic hip dislocations have severe associated injuries in as many as 40–75% of them, mostly head and visceral injuries, contralateral femur fractures, ipsilateral leg and knee injuries, and upper limb injuries [8]. In a large number of traffic accident cases, the right side of the vehicle is more involved in the crash; therefore, the right hip is predominantly injured [9].
The initial treatment of a patient with a dislocated hip is the same treatment for a patient with polytrauma. Life-threatening injuries must be addressed and stabilized first; however, the hip dislocation is an orthopedic emergency that requires immediate evaluation and reduction to avoid further complications. In general, open reduction and internal fixation of the acetabular fracture is best done in the first 10 days after injury [10]. Surgical treatment of the acetabular fracture has to be delayed in some patients because of associated injuries.
We described a case of a complex fracture pattern involving ipsilateral intertrochanteric fracture associated with ipsilateral posterior hip dislocation and posterior acetabular wall fracture. Few similar cases have been described in the literature [4, 5, 6, 7]. Up to now, such a fracture pattern has not been explained by the classification systems described for hip dislocation injuries [11, 12].
In our case, through Kocher-Langenbeck, we performed open reduction and fixation for intertrochanteric, posterior acetabular wall, and posterior column fractures in one session of surgery. Avascular necrosis of the femoral head, post-traumatic osteoarthritis, heterotopic ossification around the joint, and paralysis of the sciatic nerve are the main complications that can occur following hip dislocation with acetabular fractures [3, 13, 14].
On the follow-up of the patient, he did not get avascular necrosis of the femoral head, could be due to the early intervention. As the time passed between the initial trauma and reduction directly influences the incidence of avascular necrosis. Hougaard and Thomsen reviewed 98 patients with 100 dislocations after a minimum follow-up of 5 years to clarify the prognostic factors influencing the incidence of avascular necrosis of the femoral head. They observed the development of avascular necrosis in 4.8% of the hips reduced within 6 h and in 52.9% of the hips reduced more than 6 h after the injury [15].
The risk of developing AVN may also increase by performing an open reduction for the hip joint dislocation [6]. The sciatic nerve injury is common in traumatic posterior hip dislocations associated with displaced posterior acetabular fractures which have been reported to occur in 10–13% of patients [16].
With the increase in high-energy trauma and associated injuries, early recognition and intervention are needed for successful outcomes in cases with such complex injuries. Pre-operative planning is of high importance to achieve satisfactory results, as in our case, the surgeon addressed many fractures using single approach in one-stage operation.
The rapid evaluation and treatment are crucial in the management of such cases to avoid significant long-term morbidity.
References
- 1.Michael H. The anatomy of the hip joint. In: Surgery of the Hip Joint. New York: Springer; 1984. p. 45-74. [Google Scholar]
- 2.Azar FM, Canale ST, Beaty JH. Campbell’s Operative Orthopaedics E-book. Netherlands: Elsevier Health Sciences; 2016. [Google Scholar]
- 3.Thompson VP, Epstein HC. Traumatic dislocation of the hip: A survey of two hundred and four cases covering a period of twenty-one years. JBJS 1951;33:746-92. [Google Scholar]
- 4.Sinha S, Naik AK, Arya RK, Jain VK. Ipsilateral traumatic posterior hip dislocation, posterior wall and transverse acetabular fracture with trochanteric fracture in an adult: Report of first case. J Orthop Case Rep 2013;3:31. [Google Scholar]
- 5.Agarwal R, Rai A, Saraf S, Singh S, Singh A. An unusual pattern of posterior dislocation of hip associated with comminuted trochanteric fracture. Internet J Orthop Surg 2008;9:1-4. [Google Scholar]
- 6.Alexa O, Puha B, Veliceasa B, Păduraru D. Posterior dislocation of the hip associated with ipsilateral trochanteric fracture--a very rare case. Chirurgia (Bucur) 2009;104:761-4. [Google Scholar]
- 7.Jamshidi MH, Mirkazemi M, Birjandinejad A. Posterior hip fracture-dislocation associated with ipsilateral intertrochantric fracture; A rare case report. Arch Bone Joint Surg 2014;2:75. [Google Scholar]
- 8.Tornetta P, Mostafavi HR. Hip dislocation: Current treatment regimens. J Am Acad Orthop Surg 1997;5:27-36. [Google Scholar]
- 9.Singh R, Singh HK, Gupta SC, Kumar Y. Pattern, severity and circumtances of injuries sustained in road traffic accidents: A tertiary care hospital-based study. Indian J Community Med 2014;39:30. [Google Scholar]
- 10.Brueton RN. A review of 40 acetabular fractures: The importance of early surgery. Injury 1993;24:171-4. [Google Scholar]
- 11.Pipkin G. Treatment of grade IV fracture-dislocation of the hip: A review. JBJS 1957;39:1027-197. [Google Scholar]
- 12.Brumback RJ, Kenzora JE, Levitt LE, Burgess AR, Poka A. Fractures of the femoral head. Hip 1987;???: 181-206. [Google Scholar]
- 13.Armstrong JR. Traumatic dislocation of the hip joint. J Bone Joint Surg Br 1948;30:430-45. [Google Scholar]
- 14.Stewart MJ, Milford LW. Fracture-dislocation of the hip: An end-result study. JBJS 1954;36:315-42. [Google Scholar]
- 15.Hougaard K, Thomsen PB. Traumatic posterior dislocation of the hip-prognostic factors influencing the incidence of avascular necrosis of the femoral head. Arch Orthop Traum Surg 1986;106:32-5. [Google Scholar]
- 16.Jacob JR, Karakaş ES, Aksu S, Atlihan D, Turk CY, Halici M. Traumatic dislocation and fracture dislocation of the hip. A long-term follow-up study. Clin Orthop Related Res 1987;214:249-63. [Google Scholar]