In patients that presents with a non-displaced or minimally displaced type II odontoid fracture, a past medical history of seizures should be a relative indication to fix the odontoid fracture due to risk of seizure displacing the odontoid fracture.
Dr. Matthew A. Prevost, Department of Orthopaedic Surgery, Medical College of Georgia at Augusta University, Augusta, Georgia, USA. E-mail: mprevost@augusta.edu
Introduction: Odontoid fractures are one of the most common injuries to the cervical spine. Type II odontoid fracture treatment varies depending on age, co-morbidities, and fracture morphology. Treatment ranges from cervical orthosis to surgical intervention. Currently fractures with high non-union rates are considered for operative management which includes displacement of >6 mm, increasing age (>40-60 years), fracture gap >1 mm, delay in treatment >4 days, posterior re-displacement >2 mm, increased angulation, and history of smoking. While re-displacement of >2 mm has been associated with increased risk of non-union;, to the best of our knowledge, no studies have looked at the risk factors for re-displacement.
Case Report: We present two 26-year-old male patients who were found to have minimally displaced type II odontoid fractures initially treated in a cervical collar. These two patients were subsequently found to have displaced their odontoid fracture after having a documented seizure.
Conclusion: We suggest that a history of seizures be considered a risk factor for re-displacement of non-displaced type II odontoid fractures.
Keywords: Operative indications odontoid case report, Type II odontoid fracture, Displacement, Seizure, Odontoid fracture displacement, Nondisplaced type Ⅱ odontoid fracture.
Odontoid fractures are one of the most common injuries to the cervical spine with a recent increase in incidence. These fractures now account for 15% of traumatic cervical spine injuries [1]. There is a bimodal age distribution among those who sustain an odontoid fracture. Younger patients typically are associated with high-energy mechanisms such as motor vehicle crashes, often with concomitant injuries. Elderly patients more commonly sustain low energy mechanisms such as a ground level fall [2].
In 1974, Anderson and D’Alonzo described three types of odontoid fractures and remain the most commonly used classification. A type I odontoid fracture involves the most proximal tip of the odontoid and represents an avulsion fracture of the alar ligament. The type II fracture traverses the waist of the odontoid and is the most common fracture type. Type III fractures are through the body of the axis, maintaining the odontoid process intact. Each type is then further characterized as either displaced or nondisplaced [3]. Type I fractures are generally considered stable fractures due to the commonly retained transverse ligament and at least one alar ligament; thus, it can be treated in a hard cervical collar [2]. Type III fractures are also generally managed nonoperatively with either a halo vest (HV) or hard cervical collar [2,4]. Management of type II fractures is still highly controversial and is the subject of much debate currently.
Type II odontoid fracture patterns are at a higher risk of non-union due to the watershed blood supply to the odontoid from the internal carotid artery and the vertebral artery. Pseudarthrosis has been reported as high as 85% with non-operative treatment [5]. Fusion rates have been recorded as high as 100% in C1–2 posterior spinal fusion; however, surgery comes with its own inherent risks [5]. Elderly patients who may already be medically compromised (chronic obstructive pulmonary disease, chronic heart failure, dementia, diabetes, hypertension, myocardial infarction [MI], etc.) are at an increased risk for surgical complications such as MI, cerebrovascular accidents (CVA/transient ischemic attack), pulmonary embolism, cardiac arrhythmia, pneumonia, and deep vein thrombosis [6]. Furthermore, the clinical significance of osseous union versus fibrous union has not been established [5]. A lack of correlation between osseous union and clinical outcomes was shown by Molinari et al. when they reviewed 34 geriatric patients with type II odontoid fractures treated in a cervical orthosis. Odontoid osseous union did not correlate with clinical outcomes such as neck pain and disability in their study [7]. However, current surgical indications are aimed at identifying fracture types that are at an increased risk of non-union. The following have been reported in the literature to increase non-union rates: Displacement of >6 mm, increasing age (>40–60 years), fracture gap >1 mm, delay in treatment >4 days, posterior re-displacement >2 mm, increased angulation, and history of smoking (Table 1) [2,4,8,9]. While re-displacement of >2 mm has been associated with increased risk of nonunion, no studies of our knowledge have looked at the risk factors for re-displacement. If risk factors can be identified upon injury, the treating physician can better predict who may fail non-operative management at the initial evaluation.
Non-operative treatment options for odontoid fractures include HV and semi-rigid cervical collar. The HV is considered more stable than cervical collars but come with increased morbidity and mortality, especially in the elderly [10]. The clinical relevance of this increased stability has recently been questioned with some evidence that cervical collars have equal failure rates as HV without the increased complications [11]. Operative management of odontoid fractures includes variations of either anterior screw fixation of the odontoid or posterior spinal fusion of C1–C2. Both options have inherent pros and cons such as difficulty of the procedure, dysphagia, and loss of range of motion. Operative management through either approach also carries the risks of anesthesia, which is more significant in the geriatric population with comorbid conditions [4,6].
Case 1
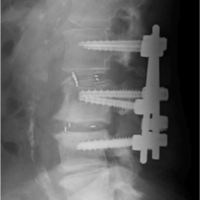
A 26-year-old male was admitted with a type II odontoid fracture that was minimally displaced (<2 mm) and minimally posteriorly angulated after falling from a tree (Fig. 1).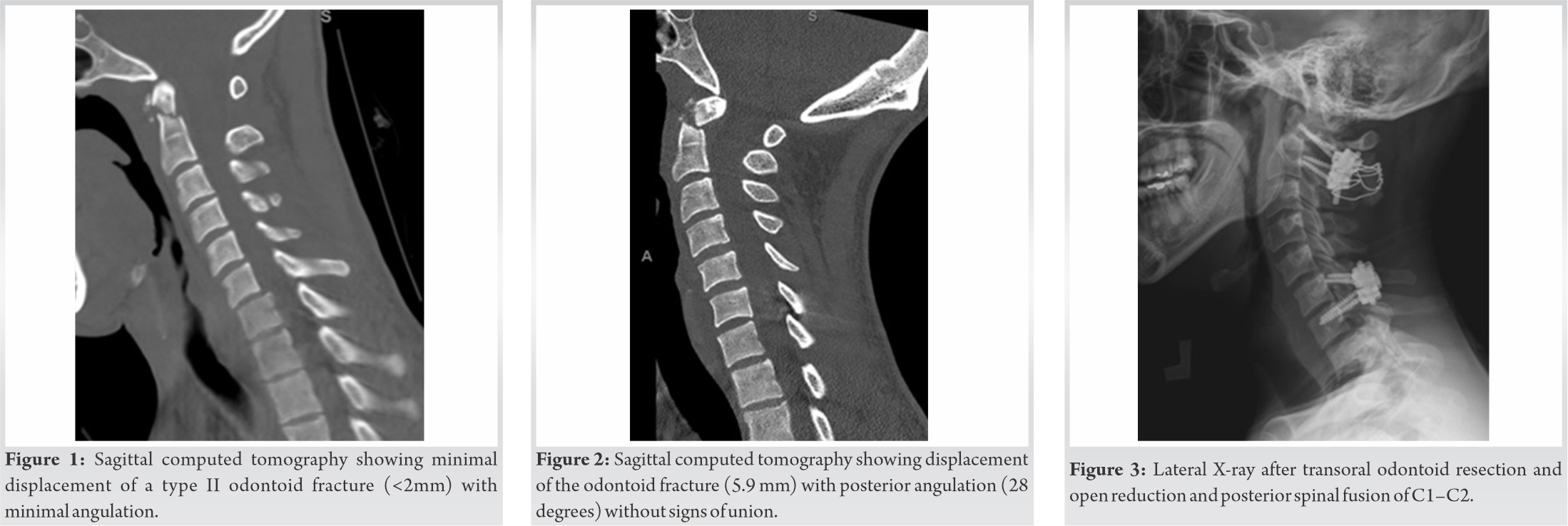 He also had a nondisplaced C1 arch fracture, left C7 lateral mass fracture/dislocation with C6–7 anterolisthesis. He complained of subjective numbness in the left hand and neck pain. His medical history was significant for epilepsy treated with medication and was reported to be seizure free. On exam, he had a normal neurological exam of his spine to include sensation, motor strength, and reflexes (ASIA E). He underwent open reduction and posterior spinal fusion of C6–7 the next day while the odontoid fracture was treated nonoperatively in a cervical collar. He was followed in clinic with serial physical exams and radiographs at 3 weeks, 6 weeks, and 12 weeks. He remained in his c-collar consistently at the 3 and 6 weeks follow-up appointments with mild neck pain, normal neurological exam (ASIA E), and maintained alignment of odontoid fracture on radiographs. At his 12-week post-operative appointment, he reported that while he had been incarcerated, he did not take his seizure medications and did not wear his cervical collar. He had four seizures with resulting new left-hand pain. He was found to have decreased but intact sensation to the left C6 and C8 distributions and positive Hoffman’s reflex bilaterally (ASIA E). A radiograph and computed tomography (CT) exam were obtained that confirmed displacement of the odontoid fracture (5.9 mm) with posterior angulation (28 degrees) without signs of union (Fig. 2). The patient began having subjective bilateral hand numbness. On flexion and extension films no motion was noted, but he noted a positive Lhermittes and worsening function. Magnetic resonance imaging (MRI) showed evidence of spinal cord compression due to the posteriorly angulated odontoid. The patient was indicated for transoral odontoid resection in conjunction with an open reduction and posterior spinal fusion of C1–C2 (Fig. 3). Postoperatively, he continued to do well despite having additional documented seizures. Six months after surgery, the patient reported minimal neck pain, stiffness, and no subjective numbness in either hand. On physical exam, he was found to have limited neck flexion and extension (15/10 degrees) with a normal neurological exam (ASIA E).
He also had a nondisplaced C1 arch fracture, left C7 lateral mass fracture/dislocation with C6–7 anterolisthesis. He complained of subjective numbness in the left hand and neck pain. His medical history was significant for epilepsy treated with medication and was reported to be seizure free. On exam, he had a normal neurological exam of his spine to include sensation, motor strength, and reflexes (ASIA E). He underwent open reduction and posterior spinal fusion of C6–7 the next day while the odontoid fracture was treated nonoperatively in a cervical collar. He was followed in clinic with serial physical exams and radiographs at 3 weeks, 6 weeks, and 12 weeks. He remained in his c-collar consistently at the 3 and 6 weeks follow-up appointments with mild neck pain, normal neurological exam (ASIA E), and maintained alignment of odontoid fracture on radiographs. At his 12-week post-operative appointment, he reported that while he had been incarcerated, he did not take his seizure medications and did not wear his cervical collar. He had four seizures with resulting new left-hand pain. He was found to have decreased but intact sensation to the left C6 and C8 distributions and positive Hoffman’s reflex bilaterally (ASIA E). A radiograph and computed tomography (CT) exam were obtained that confirmed displacement of the odontoid fracture (5.9 mm) with posterior angulation (28 degrees) without signs of union (Fig. 2). The patient began having subjective bilateral hand numbness. On flexion and extension films no motion was noted, but he noted a positive Lhermittes and worsening function. Magnetic resonance imaging (MRI) showed evidence of spinal cord compression due to the posteriorly angulated odontoid. The patient was indicated for transoral odontoid resection in conjunction with an open reduction and posterior spinal fusion of C1–C2 (Fig. 3). Postoperatively, he continued to do well despite having additional documented seizures. Six months after surgery, the patient reported minimal neck pain, stiffness, and no subjective numbness in either hand. On physical exam, he was found to have limited neck flexion and extension (15/10 degrees) with a normal neurological exam (ASIA E).
Case 2
A 26-year-old male presented after a high-speed all-terrain vehicle accident with a type II odontoid fracture, C2 and C3 lateral mass fracture, and an L2 transverse process fracture. He had loss of consciousness but had a normal neurological exam without abnormal reflexes (ASIA E). A CT exam showed minimal displacement of an odontoid fracture (<2 mm) with minimal angulation (<5 degrees) (Fig. 4).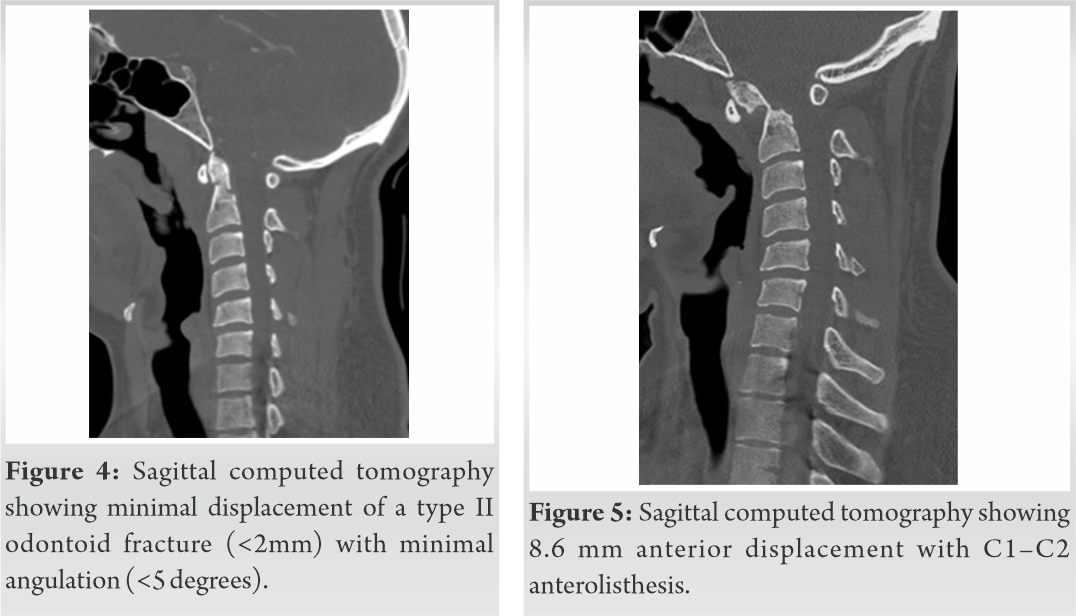 The patient was treated with a cervical collar as he demonstrated a normal exam and was instructed to follow-up as an outpatient 2 weeks later. Two days after injury while hospitalized, the patient had experienced a seizure, and an MRI was obtained by the primary medical team demonstrating diffuse axonal injury. Select cuts on this MRI incidentally showed interval displacement of odontoid fracture (6.8 mm) that was not recognized. A cervical radiograph was obtained the following day with displacement of the odontoid fracture that was not discovered until 3 months post-injury when the patient followed up with the spine team. At that time, a CT was ordered and showed 8.6 mm anterior displacement with C1–C2 anterolisthesis (Fig. 5). He also experienced a car wreck the week before this visit. He had mild neck pain with a normal neurologic exam without pathological reflexes (ASIA E) and stable flexion extension cervical radiographs. At that time, osteoclasis and reduction with PSF of C1–C2 were offered, but he elected for non-operative management.
The patient was treated with a cervical collar as he demonstrated a normal exam and was instructed to follow-up as an outpatient 2 weeks later. Two days after injury while hospitalized, the patient had experienced a seizure, and an MRI was obtained by the primary medical team demonstrating diffuse axonal injury. Select cuts on this MRI incidentally showed interval displacement of odontoid fracture (6.8 mm) that was not recognized. A cervical radiograph was obtained the following day with displacement of the odontoid fracture that was not discovered until 3 months post-injury when the patient followed up with the spine team. At that time, a CT was ordered and showed 8.6 mm anterior displacement with C1–C2 anterolisthesis (Fig. 5). He also experienced a car wreck the week before this visit. He had mild neck pain with a normal neurologic exam without pathological reflexes (ASIA E) and stable flexion extension cervical radiographs. At that time, osteoclasis and reduction with PSF of C1–C2 were offered, but he elected for non-operative management.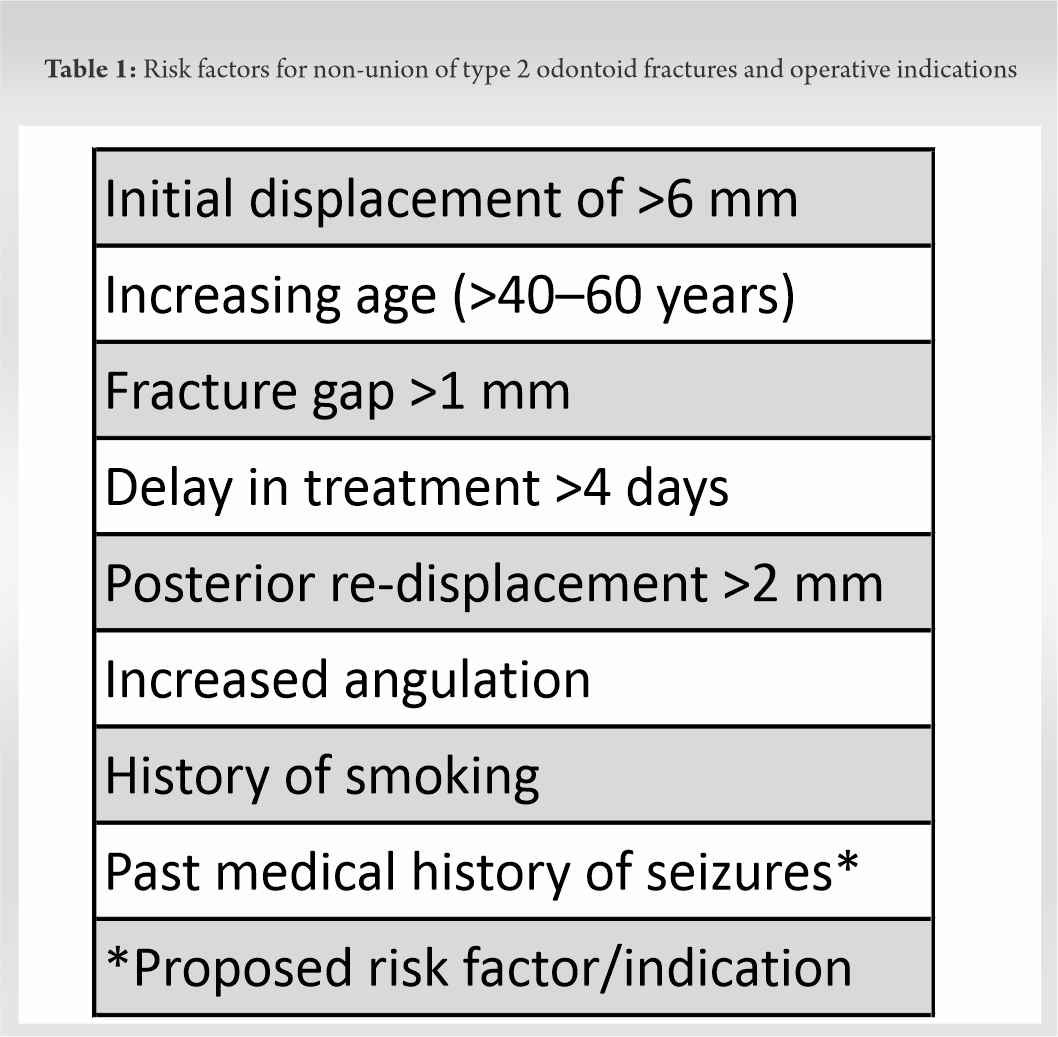
Non-operative treatment options for odontoid fractures include HVs and semi-rigid cervical collars. HVs provide the most stable external construct to prevent neck motion [4]. It allows only 3.4° of motion compared to 8.5° of motion seen with rigid cervical collars [10]. A high rate of complications from HV have been reported to include >4 times the risk of pneumonia (34%), 5 times risk of cardiac arrest, and twice as likely to have any complications versus non-HV cohort. When the cohort was compared in respect to age, elder patients (>65) were found to have a 40% mortality rate compared to only 2% in younger patients [12]. However, more recent studies show lower complication rates: 8% mortality rate and 46% complication rate (neck pain – 20.7% and decreased range of motion – 14%) with 81% clinical success [13]. Semi-rigid cervical collars have also been used to treat odontoid fractures with minimal serious adverse events. The increase in motion compared to halo has a theoretical increased risk of osseous nonunion [4]. However, a recent systematic review showed that there was no difference in failure rates of cervical collar versus halo in both young and old populations including for type II odontoid fractures. The authors also found that of the fractures that resulted in a fibrous malunion, only 7% went on to fail of which only one case had any neurological symptoms. There was, however, a significantly higher rate of complications in HV [11].
Operative management of odontoid fractures includes variations of either anterior screw fixation of the odontoid or posterior spinal fusion of C1–C2. Anterior screw fixation advantages include direct fixation across the fracture and preserved motion at C1–2. Disadvantages include difficult intraoperative imaging, osteopenia and hardware failure, dysphagia, and respiratory problems. The posterior approach relies on the posterior elements fusing which has been shown to be more reliable and predictable in outcome. The biggest disadvantage is loss of roughly 50% of axial rotation from the fusion of C1–2. Operative management through either approach also carries the risks of anesthesia, which is more significant in the geriatric population with comorbid conditions [4].
Due to the improving results of cervical collar treatment in the younger population and the disadvantages of surgical interventions, our institution has elected to treat nondisplaced odontoid fractures in both the young and the old in cervical collars. There is an abundance of literature identifying surgical indications aimed at identifying fracture types that are at an increased risk of malunion and non-union. Again, the following have been reported in the literature as having an increase in non-union rates: Displacement of >6 mm, increasing age (>40–60 years), fracture gap >1 mm, delay in treatment >4 days, posterior re-displacement >2 mm, increased angulation, and history of smoking (Table 1) [2,4,8,9]. However, there has been no literature to the authors’ knowledge that assesses the risk of a non-displaced or minimally displaced fracture progressing to a displaced fracture that would merit surgical intervention from a non-union risk. Both patients mentioned in this case series had minimally displaced type II odontoid fractures that did not originally meet any of the surgical indications based on their risk factors of non-union. However, both went on to displace their fracture after having a seizure. The authors propose that a medical history of seizures should be considered as a risk factor for displacement and that surgical intervention be considered in nondisplaced type II fractures of the odontoid. These patients may be more reliably treated with surgery initially even when they do not meet the current criteria for an increased risk of nonunion.
Type II odontoid fracture treatment is variable depending on age, comorbidities, and evolving research that ranges from cervical orthosis to surgical intervention. At present, those fractures with high non-union rates are considered for operative management which includes displacement of >6 mm, increasing age (>40–60 years), fracture gap >1 mm, delay in treatment >4 days, posterior re-displacement >2 mm, increased angulation, and history of smoking (Table 1) [2,4,8,9]. Which patients need surgical intervention and which ones can be safely treated nonoperatively is still being differentiated in current research. When reviewing our case study of two patients, we suggest that a history of seizures would be a reasonable consideration as a risk factor for future displacement of nondisplaced type II odontoid fractures. The authors agree that further research regarding the risk factors for future displacement and failure of non-operative treatment needs to be pursued.
Two young patients were diagnosed with type II odontoid fractures following a traumatic injury. During non-operative treatment in a cervical collar, both patients experienced seizures with follow-up imaging revealing displaced odontoid fractures. The authors suggest seizures as a risk factor for re-displacement of type II odontoid fractures.
References
- 1.1. Baogui L, Juwen C. Fusion rates for odontoid fractures after treatment by anterior odontoid screw versus posterior C1-C2 arthrodesis: A meta-analysis. Arch Orthop Trauma Surg 2019;139:1329-37. [Google Scholar | PubMed]
- 2.2. Chutkan NB, King AG, Harris MB. Odontoid fractures: Evaluation and management. J Am Acad Orthop Surg 1997;5:199-204. [Google Scholar | PubMed]
- 3.3. Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. 1974. J Bone Joint Surg Am 2004;86:2081. [Google Scholar | PubMed]
- 4.4. Iyer S, Hurlbert RJ, Albert TJ. Management of odontoid fractures in the elderly: A review of the literature and an evidence-based treatment algorithm. Neurosurgery 2018;82:419-30. [Google Scholar | PubMed]
- 5.5. Chapman J, Smith JS, Kopjar B, Vaccaro AR, Arnold P, Shaffrey CI, et al. The AOSpine North America geriatric odontoid fracture mortality study: A retrospective review of mortality outcomes for operative versus non-operative treatment of 322 patients with long-term follow-up. Spine (Phila Pa 1976) 2013;38:1098-104. [Google Scholar | PubMed]
- 6.6. Kasparek MF, Boettner F, Rienmueller A, Weber M, Funovics PT, Krepler P, et al. Predicting medical complications in spine surgery: Evaluation of a novel online risk calculator. Eur Spine J 2018;27:2449-56. [Google Scholar | PubMed]
- 7.7. Molinari RW, Khera OA, Gruhn WL, McAssey RW. Rigid cervical collar treatment for geriatric type II odontoid fractures. Eur Spine J 2012;21:855-62. [Google Scholar | PubMed]
- 8.8. Smith JS, Kepler CK, Kopjar B, Harrop JS, Arnold P, Chapman JR, et al. Effect of type II odontoid fracture non-union on outcome among elderly patients treated without surgery: Based on the AOSpine North America geriatric odontoid fracture study. Spine (Phila Pa 1976) 2013;38:2240-6. [Google Scholar | PubMed]
- 9.9. Koivikko MP, Kiuru MJ, Koskinen SK, Myllynen P, Santavirta S, Kivisaari L. Factors associated with non-union in conservatively-treated Type-II fractures of the odontoid process. J Bone Joint Surg Br 2004;86:1146-51. [Google Scholar | PubMed]
- 10.10. Johnson RM, Hart DL, Simmons EF, Ramsby GR, Southwick WO. Cervical orthoses. A study comparing their effectiveness in restricting cervical motion in normal subjects. J Bone Joint Surg Am 1977;59:332-9. [Google Scholar | PubMed]
- 11.11. Waqar M, Van-Popta D, Barone DG, Sarsam Z. External immobilization of odontoid fractures: A systematic review to compare the halo and hard collar. World Neurosurg 2017;97:513-7. [Google Scholar | PubMed]
- 12.12. Tashjian RZ, Majercik S, Biffl WL, Palumbo MA, Cioffi WG. Halo-vest immobilization increases early morbidity and mortality in elderly odontoid fractures. J Trauma 2006;60:199-203. [Google Scholar | PubMed]
- 13.13. Isidro S, Molinari R, Ikpeze T, Hernandez C, Mahmoudi MS, Mesfin A. Outcomes of halo immobilization for cervical spine fractures. Global Spine J 2019;9:521-6. [Google Scholar | PubMed]