Whenever destruction of posterior elements of the spine is seen on magnetic resonance imaging always keep neoplasm in differential diagnosis.
Dr. Nandlal Bharwani, Department of Orthopaedics, Dr. S.N Medical College, Jodhpur, Rajasthan India. E-mail: nandlalbharwani21@gmail.com
Introduction: Hemangioma is most common lesion frequently encountered in dorsolumbar region. Although most of these lesions are asymptomatic and are incidental findings on imaging such as computed tomography (CT)-scan and magnetic resonance imaging (MRI).
Case Report: A 24-year-old young male presenting to orthopedic outdoor with complaint of severe mid backache and lower limb paraparesis which developed after trivial trauma and increases with daily routine activities such as sitting, standing, and postural changes. For these lesion, “Enneking staging” was used.
Conclusion: In such unusual cases, it is very important to differentiate these lesions from vertebral body metastasis, pott’s spine, or aggressive bone tumors to reduce intraoperative or post-operative complications.
Keywords: Hemangioma, enneking staging, vertebrae, MRC grading.
Hemangioma of vertebral bodies is benign tumors of vascular origin and its incidence is approximately between 10% and 30% [1,2]. Hemangioma of vertebral bodies is most common lesions frequently encountered in dorsolumbar region [3]. It is commonly classified as typical and atypical hemangiomas based on radiological findings [4]. Although most of these lesions are asymptomatic and are incidental findings on radiological investigations such as CT-scan and MRI. Whenever it presents as aggressive lesions vertebral body destruction, extension into epidural space and paraspinal region is a characteristic finding [4]. Clinically, aggressive lesions present with back ache, neurological involvement, or signs and symptoms of the upper motor lesions [5,6,7]. We report a case of 24-year-old male presenting with severe backache and lower limb paraparesis and on magnetic resonance imaging (MRI) and computed tomography (CT)-scan presents with unusual presentation of multilevel aggressive vertebral hemangioma.
A 24-year-old male presenting to orthopedic outdoor with complaint of severe mid backache and lower limb paraparesis which developed after trivial trauma and increases with daily routine activities such as sitting, standing, and postural changes. On examination, bilateral lower limb power was 2/5 as per “Medical Research Council, London” , with no bowel and bladder involvement. Digital radiograph of dorsolumbar region shows collapse of D10-D11 vertebrae. CT scan (Fig. 1a) and MRI (Figs.1b and 2a) dorsolumbar spine without IV contrast were done and demonstrate significant destruction of D11 vertebral body with retropulsion of D11 vertebral body and abnormal high T2/STIR bone marrow signal intensity in D9-D12 vertebral bodies. CT and MRI show adjacent soft-tissue component in epidural space and paraspinal region with significant compression and compressive myelopathy changes of dorsal spinal cord. These MRI and CT findings were keeping with aggressive bone lesion.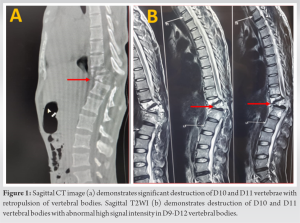
Hematological investigations including ESR and CRP were within normal limits. Informed consent was taken before undergoing invasive procedure. Then transpedicular needle biopsy was planned which turned out to be inconclusive thereafter open biopsy along with posterior segment fixation was planned using posterior midline approach for dorsolumbar spine. Posterior vertebral elements complex was eaten up which was noticed intraoperatively; therefore, frozen section was sent which suggests aggressive hemangioma like lesion followed by long segment from D7- L3 level (Fig. 3). Profuse bleeding was present intraoperatively, post-operative period was eventful on day 1 with massive blood transfusion required and patient was on ionotropic support, flaccidity in lower limbs were noticed and according to “Medical research council, London” power 1/5 in both lower limbs were recorded which gradually improved to 4/5 , 4-week post-surgery.
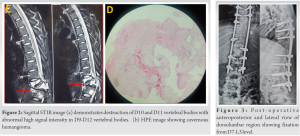
Intraoperative frozen section finding was confirmed with histopathological examination (Fig. 2b) which turned to capillary hemangioma. The vertebral body hemangioma in this case belongs to Stage 3 as per “Enneking staging classification.” “Enneking staging”- [8]
- Latent No symptoms and mild bony destruction
- Active Pain and moderate bony destruction
- Aggressive Neurological involvement and severe bony destruction with soft-tissue extension.
At each follow-up, muscle power was assessed according to “Medical Research Council, London”
In 1863, vertebral body hemangioma term was coined by virchow, commonly affecting thoracolumbar region and occurs as a result of endothelial cell growth within in marrow of vertebral body [9]. We present an aggressive thoracic vertebrae hemangioma (Stage-3 as per Enneking staging). For these lesions, CT-scan and MRI are diagnostic modalities of choice but in present case report, aggressive haemangioma had unusual presentation and it was confirmed intraoperatively frozen section and histopathological examination postoperatively. Although variable treatment options such as pre-operative embolization, surgery and radiotherapy are available but in the present case, as diagnostic imaging was not much characteristic for aggressive hemangioma along with inconclusive needle biopsy so open biopsy and posterior long segment fixation was planned [10,11,12].
Although vertebral body hemangioma is incidental finding on diagnostic modality such as CT and MRI but whenever symptomatic, they can present as low back ache, progressive paraparesis, and myelopathic signs symptoms. In such unusual cases, it is very important to differentiate these lesions from vertebral body metastasis, pott’s spine, or aggressive bone tumors to reduce intraoperative or post-operative complications.
For such unusual lesions involving vertebral bodies, radiological investigations such as MRI and intraoperative frozen sections are of utmost importance for definitive management.
References
- 1.Pastushyn AI, Slin’ko EL, Mirzoyeva GM. Vertebral hemangiomas: Diagnosis, management, natural history and clinic-pathological correlates in 86 patients. Surg Neurol 1998;50:535-47. [Google Scholar | PubMed]
- 2.Barzin M, Maleki I. Incidence of vertebral haemangioma on spinal magnetic resonance imaging in Northen Iran. Pak J Biol Sci 2009;12:542-4. [Google Scholar | PubMed]
- 3.Samade R, Malik AT, Jain N, Scharschmidt TJ, Yu E. Integrated treatment of a lumbar vertebral hemangioma with spinal stenosis and radiculopathy: A case report and a review of the literature. J Craniovertebr Junction Spine 2019;10:259-62. [Google Scholar | PubMed]
- 4.Gaudino S, Martucci M, Colantonio R, Lozupone E, Visconti E, Leone A, et al. A systematic approach to vertebral hemangioma. Skeletal Radiol 2014;44:25-36. [Google Scholar | PubMed]
- 5.Chi JH, Bydon A, Hsieh P, Witham T, Wolinsky JP, Gokaslan ZL. Epidemology and demographics for primary vertebral tumors. Neurosurg Clin N Am 2008;19:1-4. [Google Scholar | PubMed]
- 6.Jiang L, Liu XG, Yuan HS, Yang SM, Li J, Wei F, et al. Diagnosis and treatment of vertebral haemangiomas with neurologic deficit: A report of 29 cases and literature review. Spine J 2014;14:944-54. [Google Scholar | PubMed]
- 7.Schrock WB, Wetzel RJ, Tanner SC, Khan MA. Aggressive hemangioma of the thoracic spine. J Radiol Case Rep 2011;5:7-13. [Google Scholar | PubMed]
- 8.Boriani S, Weinstein JN, Biagini R. Primary bone tumors of the spine. Terminology and surgical staging. Spine Phila Pa 1976 1997;22:1036-44. [Google Scholar | PubMed]
- 9.Manning HJ. Symptomatic hemangioma of the spine. Radiology 1951;56:58-65. [Google Scholar | PubMed]
- 10.Laredo JD, Reizine D, Bard M, Merland JJ. Vertebral hemangiomas: Radiologic evaluation. Radiology 1986;161:183-9. [Google Scholar | PubMed]
- 11.Chen HI, Heuer GG, Zaghloul K, Simon SL, Weigele JB, Grady MS. Lumbar vertebral hemangioma presenting with the acute onset of neurological symptoms. Case report. J Neurosurg Spine 2007;7:80-5. [Google Scholar | PubMed]
- 12.Fox MW, Onofrio BM. The natural history and management of symptomatic and assymptomatic vertebral hemangiomas. J Neurosurg 1993;78:36-45. [Google Scholar | PubMed]










