Localized infection of Baker’s cyst presents with systemic symptoms.
Dr. Thomas Revak, Department of Orthopaedic Surgery, Division of Orthopaedic Trauma, School of Medicine, Saint Louis University, St. Louis, Missouri. E-mail: thomas.revak@health.slu.edu
Introduction: Baker’s cysts are benign fluid-filled cysts that commonly form around knee joints which typically resolve spontaneously. Infection of baker’s cysts is uncommon, but most often associated with septic arthritis or bacteremia. We describe a unique case of an infected Baker’s cyst that presented without bacteremia, septic knee, or external source of infection. This is a rare manifestation that has not been described in the current literature.
Case Presentation: This is a case of a 46 year-old woman who developed an infected Baker’s cyst without bacteremia or septic arthritis. She initially presented with the right knee pain, swelling, and limited range of motion. Blood work and synovial fluid aspiration of her right knee showed no source of infection. The patient subsequently developed erythema and tenderness over her right knee. This prompted MRI imaging that demonstrated a complex Baker’s cyst. The patient later developed a fever, tachycardia, and worsening anion-gap metabolic-acidosis. Aspiration of the fluid collection was performed and revealed purulent fluid which grew pansensitive Methicillin-Sensitive Staphylococcus aureus, blood and knee aspiration cultures remained negative. The patient was treated with antibiotics and debridement procedures and her symptoms/infection resolved.
Conclusion: Given that isolated infections of Baker’s cysts are rare, the localized aspect of this infection makes this case quite unique. Development of an infected Baker’s cyst after negative aspiration cultures, combined with the presence of systemic symptoms including fever, without evidence of systemic spread, has not been seen before in the literature to our knowledge. The unique presentation of this case is important for future analysis of Baker’s cysts as it introduces the possibility of localized cyst infections as a possible diagnosis for physicians to consider.
Keywords: Baker’s cyst, knee, infection
Baker’s (popliteal) cysts are benign fluid-filled cysts that commonly form around the knee joint in adults [1]. In adults, Baker’s cysts are commonly associated with internal knee pathology, such as meniscal or anterior cruciate ligament lesions, as well as inflammatory conditions such as osteoarthritis and rheumatoid arthritis [2,3]. Increased intracapsular pressure creates a valve-like communication allowing unidirectional flow of synovial fluid into the pre-existing gastrocnemius-semimembranosus bursa on the medial aspect of the popliteal fossa [1,2]. These cysts usually resolve spontaneously, commonly not requiring surgical intervention. If surgical intervention is required, treatment of the intracapsular pathology is the mainstay of treatment. In rare cases, the cyst may rupture causing the synovial fluid to leak into the surrounding tissues causing irritation and occasionally leading to infection. Infection of popliteal cysts is uncommon and mostly associated with septic arthritis [4,5,6]. Infections can also occur due to bacteremia since the cyst provides an ideal environment for growth and most likely are due to Staphylococcus aureus [2,3,4,7,8,9]. Furthermore, while there have been reported cases of infected Baker’s cysts, many of them ruptured [2,3,6,8,10,11]. The goal of this case report is to describe an infected Baker’s cyst without bacteremia, septic knee, or other source of infection.
A 46-year-old woman presented to the emergency room with the right knee pain and swelling which had worsened over the past 2 weeks. The patient was unable to fully extend her knee secondary to pain and restriction from swelling. Radiographs were obtained and showed no osseous lesions or fractures. Blood work was obtained which revealed a white blood cell count of 12.7, C-reactive protein of 7.2, and erythrocyte sedimentation rate of 105. The patient was evaluated by the internal medicine service and orthopedics was consulted to rule out septic right knee. A right knee aspiration was performed which revealed a synovial white blood cell count of 6500, polymorphonuclear leukocytes of 71%, and no crystals present. The patient was admitted for further evaluation and vancomycin was prophylactically started to treat suspected infections due to her worsening symptoms. On hospital day 2, a new fluctuant area with erythema and tenderness was identified on her medial proximal tibia. Magnetic resonance imaging with and without contrast was obtained of her right lower leg (Fig. 1) which revealed a complex Baker’s cyst and observation recommended due to aspiration results not concerning for septic arthritis. The following day, the patient developed a fever, worsening anion-gap metabolic-acidosis and became tachycardic and disoriented. An aspiration was performed of the posteromedial knee fluid collection which revealed purulent aspirate. Subsequently, as a results of the aspiration findings, an incision and debridement were performed of dressing. Two hundred milliliters of purulent fluid were evacuated and multiple cultures were sent for analysis. After the Baker’s cyst decompression, the flexion contracture resolved. Cultures from the Baker’s cyst aspiration and intraoperative cultures grew pansensitive Methicillin-Sensitive Staphylococcus aureus (MSSA). 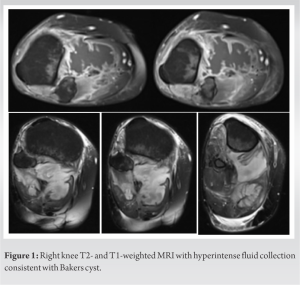 Vancomycin and Zoysn were discontinued and Nafcillin was commenced. Multiple subsequent irrigation and debridement procedures were performed with eventual wound closure. Drains were removed 3 days after wound closure and she was discharged with 4 weeks of intravenous Nafcillin. At time of discharge, knee pain and fevers had resolved and knee range of motion was nearly full. The patient presented to the clinic 2 weeks later. She was weight-bearing as tolerated at that time. Her incisions were healing well without any sign of infection, fluid reaccumulation, and her pain was well-controlled.
Vancomycin and Zoysn were discontinued and Nafcillin was commenced. Multiple subsequent irrigation and debridement procedures were performed with eventual wound closure. Drains were removed 3 days after wound closure and she was discharged with 4 weeks of intravenous Nafcillin. At time of discharge, knee pain and fevers had resolved and knee range of motion was nearly full. The patient presented to the clinic 2 weeks later. She was weight-bearing as tolerated at that time. Her incisions were healing well without any sign of infection, fluid reaccumulation, and her pain was well-controlled.
Baker’s cysts most commonly form due to degenerative knee injuries, meniscal lesions, as well as ammatory conditions such as rheumatoid arthritis or osteoarthritis. These typically will resolve witinflhout intervention [1,9]. However, on rare occasions, the Baker’s cyst will become infected in the setting of a septic knee and may require operative debridement [2]. Review of the current literature revealed only 25 cases of infected Baker’s cysts, with ten of those infected by S. aureus bacteria, the most common causative species of an infected Baker’s cyst [3]. While in the majority of the reviewed cases, the infection remained isolated to the knee joint, there were also reports of infected Baker’s cysts present in the setting of bacteremia [3,8]. Baker’s cysts are ideal places for a circulating infectious agent to accumulate [3]. An infected Baker’s cyst should be considered when the patient presents with a popliteal cyst, local inflammation, and signs of systemic infection `3]. In this case, the patient met all of these criteria including: tenderness of the popliteal knee, aggravation with full knee flexion or extension, a palpable well-circumscribed swelling, and fever. This case was particularly interesting because, although the patient developed signs of an infected Baker’s Cyst, the initial blood and knee joint fluid aspiration cultures were negative, meaning that the infection remained isolated in the cyst. The cyst grew outward, down into the gastrocnemius, instead of dispersing inward into the knee joint. It was not until the subsequent ultrasound guided aspiration of the cyst, which was drawn 5 days after admission that the source of the infection was identified. The cyst’s aspiration fluid culture demonstrated the presence of MSSA in the Baker’s cyst, but the blood culture and the proximal joint space remained negative. This means that the infection was localized to the Baker’s cyst, in the setting of an uninfected knee joint, despite the development of systemic symptoms. This development of an infected Baker’s cyst after negative fluid cultures, combined with the lack of systemic spread, has not been seen before in the literature to our knowledge.
An infected Baker’s cyst is rare; however, when there is suspicion of an infection based on the patient’s clinical presentation, blood work and a synovial fluid aspiration are sent to be cultured, allowing for diagnosis of the infective species and subsequent antibiotic treatment. After an initially negative synovial fluid culture, a subsequent cyst aspiration cultured positively for MSSA. However, despite the patient’s worsening symptoms, the blood culture and knee joint fluid culture remained negative, determining the absence of any systemic infection. The unique presentation of this case is important for future analysis and diagnosis of infected Baker cysts.
Even without bacteremia, septic arthritis, or a known external source, an infection may localize within a Baker’s cyst and cause systemic symptoms.
References
- 1.Herman AM, Marzo JM. Popliteal cysts: A current review. Orthopedics 2014;37:e678-84. [Google Scholar | PubMed]
- 2.Verbner JM, Pereira-Duarte M, Zicaro JP, Yacuzzi C, Costa-Paz M. Infected Baker’s cyst: A new classification, diagnosis and treatment recommendations. J Orthop Case Rep 2018;8:16-23. [Google Scholar | PubMed]
- 3.Drees C, Lewis T, Mossad S. Baker’s cyst infection: Case report and review. Clin Infect Dis 1999;29:276-8. [Google Scholar | PubMed]
- 4.Izumi M, Ikeuchi M, Tani T. Septic arthritis of the knee associated with calf abscess. J Orthop Surg (Hong Kong) 2012;20:272-5. [Google Scholar | PubMed]
- 5.Kosuge DD, Teare L, MacDowell A. Corynebacterium septic arthritis of the knee presenting as a ruptured septic popliteal cyst. Eur J Trauma Emerg Surg 2010;36:597-9. [Google Scholar | PubMed]
- 6.Papadopoulos A, Karachalios TS, Malizos CN, Varitimidis S. Complicated septic arthritis after knee arthroscopy in a 75-year-old man with osteoarthritis and a popliteal cyst. BMJ Case Rep 2015;2015:bcr2014207394. [Google Scholar | PubMed]
- 7.Corten K, Vandenneucker H, Reynders P, Nijs S, Pittevils T, Bellemans J, et al. A pyogenic, ruptured baker’s cyst induced by arthroscopic pressure pump irrigation. Knee Surg Sports Traumatol Arthrosc 2009;17:266-9. [Google Scholar | PubMed]
- 8.Mason L, Vannett N, Carpenter E, Davies J. Posterior leg compartment abscess following rupture of infected baker’s cyst: A complication of intra-articular corticosteroid injection. Internet J Orthop Surg 2007;10:1-4. [Google Scholar | PubMed]
- 9.Lee BI, Seo JH, Kim YB, Seo GW. A potential risk factor of total knee arthroplasty: An infected Baker’s cyst-a case report. BMC Musculoskelet Disord 2020;21:137. [Google Scholar | PubMed]
- 10.Hamabuchi M, Takeda Z. Isolated tuberculosis of the popliteal cyst. Nihon Geka Hokan 1990;59:337-43. [Google Scholar | PubMed]
- 11.Tashjian RZ, Nickisch F, Dennison D. Ruptured septic popliteal cyst associated with psoriatic arthritis. Orthopedics 2004;27:231-3. [Google Scholar | PubMed]