When any adolescent or young patient comes in OPD with chronic mid/lower back pain, Scheuermann’s disease should be differential diagnosis along with infective, inflammatory etiology.
Dr. Mohit Bansal, Department of Orthopaedics, Dr. S.N. Medical College, Jodhpur, Jodhpur, Rajasthan, India. E-mail: mb01071995@gmail.com
Introduction: Atypical Scheuermann disease involves one or two vertebral bodies which result in kyphosis.
Case Report: An 18-year-old male presented in OPD with a complaint of chronic lower back pain without any lower limb pain and neurological deficit. Radiological imaging and blood parameters were in favor of atypical Scheuermann disease.
Conclusion: Radiological and blood investigations are required to rule out other possible causes of chronic back pain to make a diagnosis of atypical Scheuermann disease which should be treated conservatively initially.
Keywords: Atypical Scheuermann disease, kyphosis, lumbar spine, adolescent patient, lower back pain.
Scheuermann disease is a common condition which results in kyphosis of thoracic or thoracolumbar spine in adolescent age, usually presented with back pain. It occurs in approximately 5% (range 0.4–8%) of the general population with slight male predominance [1,2,3]. This disease mainly affects the thoracic spine and remains painless unless any severe deformity occurs and lumbar spine is affected less commonly [4,5,6]. Blumenthal et al. classified the Scheuermann disease into typical and atypical forms, respectively, according to affected area [7]. Sørensen [1] explained the radiological criteria for typical Scheuermann disease (anterior wedging >5° in at least three adjacent vertebral bodies), whereas Blumenthal et al. [7] described atypical Scheuermann disease which remains undetected in daily clinical practice. Radiological criteria for atypical Scheuermann disease include more than 5° anterior wedging in one or two vertebral bodies, changes in vertebral end plate, narrow disk space, and anterior schmorl nodes. Greene et al. suggested that disk material can be broken due to excessive force on immature vertebral body within the vertebral body [8]. We report a case of 18-year-old male presenting with complain of lower back pain. On radiography and magnetic resonance imaging (MRI) of spine suggestive of atypical Scheuermann disease.
A 18-year-old male presented to orthopedics clinic with complaint of lower back pain without any lower limb pain from past 6 months which was spontaneous in onset after trivial fall, increased with activity, and relieved by rest and analgesics, no diurnal and postural variation was observed. On examination, the patient was having muscular spasm of paravertebral muscle with reduced range of motion at lumbar spine noted. We did not observe any kind of neurological involvement in the patient. Chances of thecal sac compression are rare in these patients unless any concomitant disc disease. He had no visual deformity in spine, and no obvious swelling. We evaluated the patient further with radiological imaging and blood investigations. On digital X-ray of lumbosacral spine which showed irregularity in superior end plate of L3 vertebrae with decreased lordosis in lumbar region. MRI of lumbosacral spine showed anterior wedging in L3 vertebral body, erosion of superior end plate of L3 vertebra, narrow disk space of L3–L4, and schomrl nodes in L3 vertebrae (Fig. 1). Blood parameters CBC, ESR, and CRP were within normal limits which exclude any infective or inflammatory etiology. On basis of all above findings, it was suggestive of atypical Scheuermann disease (type IIa) which involves only one vertebra. This disease is divided into two types:
- Typical Scheuermann disease (type I): It involves three or more than three thoracic vertebrae which causes kyphotic deformity in dorsal spine. Adolescents have more chances of this type
- Atypical Scheuermann disease (type IIa): It involves one or two vertebrae of dorsolumbar or lumbar segment, disk space narrowing, and anterior schmorl nodes. It is seen less commonly
- Acute traumatic intraosseous disk herniation (type IIb): It consists history of acute vertical compression injury resulting in severe back pain and evidence of end plate fracture (anterior schmorl nodes).
The patient was explained about the disease and treated conservatively with anti-inflammatory medication and physical therapy. Indications for surgery include progression of deformity, cosmesis, severe pain and rarely, cardiopulmonary or neurological compromise.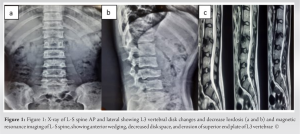
Scheuermann disease was described in 1920 as structural hyperkyphosis of thoracic or thoracolumbar spine [9]. It mainly involves multiple vertebrae. Other forms of this disease involve one or two levels of vertebrae which are very rare entity. These patients presented with back pain and radiological imaging shows erosion of vertebral bodies which mimics infectious etiology, but knowledge of this rare presentation with hematological parameters helps us to differentiate it from other disorders. Hence, all clinical and radiological parameters are required to make a diagnosis of atypical Scheuermann disease which can avoid from overtreatment or un-useful treatment [10]. Treatment of this disease is suggested in many articles which include conservative treatment until there is severe deformity or any neurological involvement [11,12].
Atypical Scheuermann disease is a very rare presentation which involves one or two lumbar vertebrae in patients. Patients have only complained of back pain generally and can be missed out. Radiological investigations (MRI and digital radiographs) and blood parameters (CBC, ESR, and CRP) with clinical history are required to make a proper diagnosis.
When adolescent or young patient comes in OPD with chronic mid or lower back pain then differentials such as infective cause, inflammatory cause, tumors, and degenerative disease should be ruled out with radiological investigations and blood parameters. Atypical Scheuermann disease should be treated conservatively until any neurological involvement any obvious deformity or cardiopulmonary involvement.
References
- 1.Sørensen KH. Scheuermann’s Juvenile Kyphosis: Clinical Appearances, Radiography, Etiology and Prognosis. Copenhagen: Munksgaard; 1964. p. 2. [Google Scholar | PubMed]
- 2.Gavin TM. The etiology and natural history of Scheuermann’s kyphosis. J Prosthet Orthot 2003;15:S11-4. [Google Scholar | PubMed]
- 3.Damborg F, Engell V, Andersen M, Kyvik KO, Thomsen K. Prevalence, concordance, and heritability of Scheuermann kyphosis based on a study of twins. J Bone Joint Surg Am 2006;88:2133-6. [Google Scholar | PubMed]
- 4.Mandell GA, Morales RW, Harcke HT, Bowen JR. Bone scintigraphy in patients with atypical lumbar Scheuermann disease. J Pediatr Orthop 1993;13:622-7. [Google Scholar | PubMed]
- 5.Shelton YA. Scoliosis and kyphosis in adolescents: Diagnosis and management. Adolesc Med State Art Rev 2007;18:121-39, X. [Google Scholar | PubMed]
- 6.Harreby M, Neergaad K, Hesselsoe G, Kjer J. Are radiologic changes in the thoracic and lumbar spine of adolescents risk factors for low back pain in adults? A 25-year prospective cohort study of 640 school children. Spine (Phila Pa 1976) 1995;20:2298-302. [Google Scholar | PubMed]
- 7.Blumenthal SL, Roach J, Herring JA. Lumbar Scheuermann’s. A clinical series and classification. Spine (Phila Pa 1976) 1987;12:929-32. [Google Scholar | PubMed]
- 8.Greene TL, Hensinger RN, Hunter LY. Back pain and vertebral changes simulating Scheuermann’s disease. J Pediatr Orthop 1985;5:1-7. [Google Scholar | PubMed]
- 9.Scheuermann HW. Kyphosis dorsalis juvenilis. Ugesk Leager 1920;82:385-93. [Google Scholar | PubMed]
- 10.Martín JC, Rodríguez LA, Dios JA, Martínez AD. Dolor de espalda en la infancia. An Esp Pediatr 1997;46:133-7 . [Google Scholar | PubMed]
- 11.Lucas-García FJ, Vicent-Carsí V, Sánchez-González M. Enfermedad de Scheuermann lumbar atípica: A propósito de 6 casos. Rev Esp Cir Ortop Traumatol 2013;57:135-9. [Google Scholar | PubMed]
- 12.Palazzo C, Sailhan F, Revel M. Scheuermann’s disease: An update. Joint Bone Spine 2014;81:209-14. [Google Scholar | PubMed]