Keeping pseudoaneurysm on the differential for bone lesions is essential as they have a remarkably different treatment plan than a tumor or infection, which they may imitate.
Dr. Drew D. Moore, Department of Orthopedic Surgery, William Beaumont University Hospital, 3535 W. 13 Mile Road, Suite 744, Royal Oak, MI 48073, USA. E-mail: drew.moore@corewellhealth.org
Introduction: Pseudoaneurysms are vascular lesions occurring after injury to a blood vessel wall. Peripheral artery pseudoaneurysms as a fracture complication are uncommon and typically appear immediately after trauma or surgery. We report a unique case of sciatic nerve palsy associated with external iliac artery pseudoaneurysm arising 20 years after pelvic trauma, presenting within the fracture site as an erosive bone lesion masquerading as a possible malignancy. To the best of our knowledge, no cases of delayed external iliac artery pseudoaneurysm involving sciatic pain have been reported.
Case Report: We present a 78-year-old female who sustained an acetabular fracture with an uneventful recovery for 20 years. The patient presented post-injury with symptoms and physical examination findings consistent with sciatic nerve palsy. Computed tomography angiography and duplex imaging revealed a pseudoaneurysm of the external iliac artery. The patient was taken to the operating room for endovascular repair of the external iliac artery using a covered stent.
Conclusion: This case of sciatic nerve palsy is a unique contribution to the literature concerning the specific vascular injury observed and the delayed presentation of pseudoaneurysm causing sciatic nerve palsy. Orthopedic surgeons must consider a wide differential when confronted with suspicious pelvic masses. Failure to diagnose these as a vascular etiology could prove catastrophic should the surgeon attempt an open debridement or sampling.
Keywords: Pseudoaneurysm, false aneurysm, sciatic nerve palsy, pelvis fracture, bone lesion.
Pseudoaneurysms of the external iliac artery are often clinically silent, making them difficult to detect, but the consequences of rupture can be life-threatening [1]. Peripheral artery pseudoaneurysms as a complication of fractures are uncommon; most appear immediately after trauma or surgery [2, 3]. Even rarer are pseudoaneurysms that occur at fracture sites following an uneventful period of months or years [4, 5]. Extraspinal causes of sciatic pain and motor dysfunction most commonly occur following lumbar disc disease, resulting in compression of nerve roots. We report a unique case of sciatic nerve palsy associated with external iliac artery pseudoaneurysm arising 20 years after a quiescent pelvic trauma that presented within the fracture site as an erosive bone lesion masquerading as a possible malignancy.
A 78-year-old female presented to the emergency department with subacute intractable left lower extremity neuropathic pain, back pain, and left foot drop. The patient reported a fall 20 years ago in Iraq, sustaining a left acetabular fracture; the fracture was treated non-operatively at that time. Specific treatment modalities are unknown. The patient reports ambulating with minimal difficulty but has had intermittent left hip pain since her initial fracture. In the past 6 months, she has had increasing back pain, left-sided radiculopathy-like pain, and excruciating pain over her left foot. She also developed a left foot drop in the past 2 weeks before presenting to the emergency department. Her neuromuscular examination revealed strength scores in the left lower extremity of four for hip flexion, five for knee extension, zero for ankle dorsiflexion, one for great toe extension, and four for ankle plantar flexion. She had hypersensitivity in superficial peroneal, deep peroneal, sural, saphenous, and tibial distributions. She had a brisk capillary refill and a palpable dorsalis pedis pulse. An initial pelvic radiograph showed no fracture or soft-tissue abnormality but significant hip arthrosis and sclerotic changes around the greater sciatic notch on the left innominate bone (Fig. 1). The primary team performed computed tomography (CT) with oral contrast of the abdomen and pelvis. CT demonstrated post-traumatic changes involving the left iliac bone with a lytic lesion containing cystic or soft-tissue components favored to represent tumor or infection (Fig. 1a). The lesion extended from the supra-acetabular region into the pelvis and under the psoas muscle posteriorly (Fig. 1b). The intraosseous component measured 5.8 cm × 3.6 cm, the soft-tissue component measured 5.0 cm × 3.5 cm, and the craniocaudal height measured up to 7 cm. The patient had no history of cancer. The patient had pain with palpation of the groin and deep pressure over the anterior superior iliac spine and greater trochanter. Orthopedic oncology was consulted for concern of tumor or infection within the acetabulum. Magnetic resonance imaging (MRI) with contrast was then performed to evaluate and determine if biopsy or aspiration was required (Fig. 2a).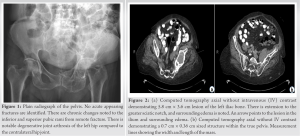 MRI suggested a nonaggressive mass, given that it was partially visualized on a prior examination from 2014. Likely etiologies such as peripheral nerve sheath tumor, vascular aneurysm, and an organized hematoma were considered – mucinous or myxoid-type neoplasm was less likely. A CT-guided biopsy was performed, which revealed coagulated blood and no malignancy raising suspicion of a vascular lesion. A CT angiography (CTA) with intravenous contrast of the pelvis was then performed and revealed a mass within the left iliac bone concerning for external iliac artery pseudoaneurysm (Fig. 2b). The mass on CTA was seen close to the neurovascular bundle, suggesting that the sciatic nerve palsy symptoms were secondary to mass compression of the sciatic nerve. Duplex imaging revealed a 4 cm pseudoaneurysm (Fig. 2c). No orthopedic intervention was planned, and vascular surgery was consulted, given the diagnosis of pseudoaneurysm. Endovascular repair of the external iliac artery using a covered stent was performed without complication. The patient began acetylsalicylic acid and apixaban on discharge. The patient’s stent healed uneventfully. An MRI at 18 months showed improvement in the previous erosive remodeling due to pseudoaneurysm (Fig. 3).
MRI suggested a nonaggressive mass, given that it was partially visualized on a prior examination from 2014. Likely etiologies such as peripheral nerve sheath tumor, vascular aneurysm, and an organized hematoma were considered – mucinous or myxoid-type neoplasm was less likely. A CT-guided biopsy was performed, which revealed coagulated blood and no malignancy raising suspicion of a vascular lesion. A CT angiography (CTA) with intravenous contrast of the pelvis was then performed and revealed a mass within the left iliac bone concerning for external iliac artery pseudoaneurysm (Fig. 2b). The mass on CTA was seen close to the neurovascular bundle, suggesting that the sciatic nerve palsy symptoms were secondary to mass compression of the sciatic nerve. Duplex imaging revealed a 4 cm pseudoaneurysm (Fig. 2c). No orthopedic intervention was planned, and vascular surgery was consulted, given the diagnosis of pseudoaneurysm. Endovascular repair of the external iliac artery using a covered stent was performed without complication. The patient began acetylsalicylic acid and apixaban on discharge. The patient’s stent healed uneventfully. An MRI at 18 months showed improvement in the previous erosive remodeling due to pseudoaneurysm (Fig. 3). 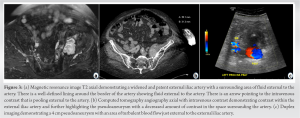 A post-operative pelvis radiograph at 18 months demonstrated interval stent placement and stable bony changes without further erosion or compromise (Fig. 5). The interosseous component was overall smaller in size compared to the previous CT. The patient has not maintained regularly scheduled follow-up, but she has been to the hospital multiple times since stent placement for other concerns. In the most recent consult notes, the patient’s motor symptoms have fully resolved 2 years post-repair. Extensor hallucis longus and tibialis anterior motor function have returned. She maintains intact sensation throughout the ankle and foot.
A post-operative pelvis radiograph at 18 months demonstrated interval stent placement and stable bony changes without further erosion or compromise (Fig. 5). The interosseous component was overall smaller in size compared to the previous CT. The patient has not maintained regularly scheduled follow-up, but she has been to the hospital multiple times since stent placement for other concerns. In the most recent consult notes, the patient’s motor symptoms have fully resolved 2 years post-repair. Extensor hallucis longus and tibialis anterior motor function have returned. She maintains intact sensation throughout the ankle and foot.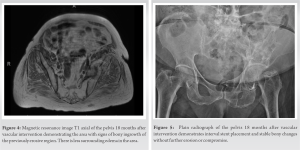
A pseudoaneurysm, or false aneurysm, is a vascular lesion that occurs when a blood vessel wall is injured – blood escapes through a gap in the vessel wall and collects in the surrounding tissue. It may be contained by adventitia or surrounding perivascular soft tissue. Pseudoaneurysms are unlike true aneurysms because they lack the complete arterial wall and tend to have an adjacent hemorrhage. Several reports describe cases of pseudoaneurysm occurring in orthopedic practice following fracture, reduction attempts, during surgical fixation of a fracture, or from implants [6, 7, 8, 9]. Sharp tips of bone or implant components may injure adjacent vessels. Pseudoaneurysm of the external iliac artery following pelvis fracture is rare and likely occurs acutely [10]. Pseudoaneurysms are usually asymptomatic, except when they rupture, which may occur several days or months after the initial trauma [1]. Few cases of delayed external iliac artery pseudoaneurysm have been reported. Of the cases reported, most occurred following complications after total hip arthroplasty [11]. A predisposing factor of this complication is implant infection, which results in the loosening and migration of the acetabular component and damage to external iliac vessels [11]. Compression of the sciatic nerve may cause pain in sciatic nerve distribution and motor dysfunction, which tend to present weeks to months after the initial injury [12]. An uncommon cause of sciatic pain is the presentation of arterial pseudoaneurysm. A small percentage of false aneurysms occur at the superior and inferior gluteal arteries, branches of the internal iliac artery [11]. Several cases of pseudoaneurysms at branches of the internal iliac artery describe sciatic pain caused by compression of the sciatic nerve [12, 13]. Clinical presentation of sciatic nerve palsy may include pain and progressive leg numbness and weakness. Intrapelvic or buttock masses may compress the sciatic nerve and lumbosacral plexus, causing pain, and motor symptoms [13]. The workup for sciatic nerve palsy should include careful palpation of the abdomen and buttocks. However, external iliac artery pseudoaneurysms are challenging to diagnose because the physical examination is almost impossible. CT and MRI of the pelvic and buttock regions should be selected as initial diagnostic methods [12]. CTA and sonography are recommended to demonstrate vascular lesions clearly and confirm the diagnosis of pseudoaneurysm [14]. Thorough imaging is crucial to confirm the diagnosis of pseudoaneurysm because its presentation can mimic entities such as tumors and infection. Treatment of pseudoaneurysm is obtained through endovascular repair using a covered stent with vascular surgery [15]. Our case provides a unique example of an external iliac artery pseudoaneurysm that presented in a delayed fashion after remote trauma. The patient presented with lower extremity neuropathic pain, back pain, and left foot drop. The mass showed resolution with stenting, resulting in subsequent bone remodeling and neurologic recovery at follow-up. Orthopedic surgeons need to consider a wide differential for pelvic masses. During the care of this patient, a pseudoaneurysm was not initially considered. In this case, the pseudoaneurysm mimicked a tumor or possibly infection due to the significant bone changes and appearance on the initial CT without contrast.
To the best of our knowledge, no cases of delayed external iliac artery pseudoaneurysm involving sciatic pain have been reported. This case demonstrates that for patients presenting with sciatic nerve palsy or a history of remote trauma, keeping pseudoaneurysms on the differential for lesions in this proximity to the greater sciatic notch is essential. The decision was made to obtain further advanced imaging and, eventually a biopsy. The biopsy results helped focus the differential on a vascular lesion, and further imaging supported the diagnosis. These results led to a vastly different treatment algorithm, with successful management through an endovascular repair. The failure to diagnose these pelvic masses as a pseudoaneurysm could prove disastrous if the surgeon attempts an open debridement or sampling.
The main purpose of this article is to spread awareness regarding pseudoaneurysms, which can arise in a delayed fashion in areas of remote trauma. Diagnosing the cause of a pelvic mass can be challenging. Keeping pseudoaneurysms on the differential is essential. Failure to diagnose these as a vascular etiology could prove catastrophic should the surgeon attempt an open debridement or sampling.
References
- 1.Ozkavukcu E, Cayli E, Yağci C, Erden I. Ruptured iliac aneurysm presenting as lumbosacral plexopathy. Diagn Interv Radiol 2008;14:26-8. [Google Scholar]
- 2.Horton RE. Arterial injuries complicating orthopaedic surgery. J Bone Joint Surg Br 1972;54:323-7. [Google Scholar]
- 3.Dhal A, Chadha M, Lal H, Singh T, Tyagi S. Encounters with pseudoaneurysms in orthopaedic practice. Injury 2001;32:771-8. [Google Scholar]
- 4.Harris O, Roche C, Torreggiani W, Ritchie D, Jane M, McWilliams R, et al. Delayed presentation of pseudoaneurysm complicating closed humeral fracture: MR diagnosis. Skeletal Radiol 2001;30:648-51. [Google Scholar]
- 5.González JF, Terriza MD, Cabada T, Garcia-Araujo C. False aneurysm of the femoral artery as a late complication of an intertrochanteric fracture. A case report. Int Orthop 1995;19:187-9. [Google Scholar]
- 6.Amrani A, Dandane MA, El Alami Z, El Madhi T, Gourinda H, Miri A. False aneurysm of the radial artery: Unusual complication of both-bone forearm fracture in children: A case report. Cases J 2008;1:170. [Google Scholar]
- 7.Ritchie ED, Haverkamp D, Schiphorst TJ, Bosscha K. False aneurysm of the profunda femoris artery, a rare complication of a proximal femoral fracture. Acta Orthop Belg 2007;73:530-2. [Google Scholar]
- 8.Stephen DJ. Pseudoaneurysm of the superior gluteal arterial system: An unusual cause of pain after a pelvic fracture. J Trauma 1997;43:146-9. [Google Scholar]
- 9.O’Donoghue D, Muddu BN, Woodyer AB, Kumar R. False aneurysm of the profunda femoris artery due to malunion of a hip fracture. Injury 1994;25:681-2. [Google Scholar]
- 10.Sousa CM, Silva LF, Rodrigues ME, Félix A, Alpoim B, Marques P, et al. Spontaneous resolution of pseudoaneurysm of an iliac artery branch in a multiple trauma patient with pelvic fracture: Clinical case. Rev Bras Ortop 2015;46:87-90. [Google Scholar]
- 11.Fukuhara S, Kanki S, Daimon M, Shimada R, Ozawa H, Katsumata T. Pseudoaneurysm of the external iliac artery is a rare late complication after total hip arthroplasty. J Vasc Surg Cases Innov Tech 2017;3:149-51. [Google Scholar]
- 12.Lowenthal RM, Taylor BV, Jones R, Beasley A. Severe persistent sciatic pain and weakness due to a gluteal artery pseudoaneurysm as a complication of bone marrow biopsy. J Clin Neurosci 2006;13:384-5. [Google Scholar]
- 13.Yurtseven T, Zileli M, Göker EN, Tavmergen E, Hoşcoşkun C, Parildar M. Gluteal artery pseudoaneurysm, a rare cause of sciatic pain: Case report and literature review. J Spinal Disord Tech 2002;15:330-3. [Google Scholar]
- 14.Soto JA, Múnera F, Cardoso N, Guarín O, Medina S. Diagnostic performance of helical CT angiography in trauma to large arteries of the extremities. J Comput Assist Tomogr 1999;23:188-96. [Google Scholar]
- 15.Ricciardi E, di Martino G, Maniglio P, Schimberni M, Frega A, Jakimovska M, et al. Life-threatening bleeding after pelvic lymphadenectomy for cervical cancer: Endovascular management of ruptured false aneurysm of the external iliac artery. World J Surg Oncol 2012;10:149. [Google Scholar]








