Distraction histogenesis using Ilizarov technique not only promotes bone regeneration but also aids in soft-tissue healing.
Dr. Hari Krishna Pentela, Department of Orthopaedics, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India. E-mail: hkpentela@gmail.com
Introduction: Management of open tibial fractures with large bone segment and soft-tissue loss can be challenging. To restore the functionality of the limb, the continuity of the soft-tissue envelope and bone needs to be achieved.
Case Report: A 29-year-old gentleman sustained right leg crush injury and open Gustilo Anderson Grade IIIB right tibia shaft fracture with 17.2 cm tibial shaft bone segment loss and large soft-tissue defect. An initial free flap failed. In spite of this, the functionality of the limb was restored by bone transport using Ilizarov method.
Conclusion: The case report details the surgical technique and obstacles encountered and illustrate that bone transport using Ilizarov technique not only regenerates bone but can facilitate healing of soft tissues.
Keywords: Segmental bone loss, bone transport, Ilizarov.
The incidence of open fractures with bone loss is increasing due to rising incidence of high velocity trauma and road traffic accidents. Management of segmental bone loss after trauma remains a challenging problem for both the surgeon and the patient. Over the past decades, a various treatment techniques which have been described for the management of bone defects were bone transport using external frames such as Ilizarov ring fixator or circular hexa pods or monolateral devices, bone transport using lengthening intramedullary (IM) nails or plate fixation, Masquelet-induced membrane technique, acute shortening with or without gradual lengthening, autogenous bone grafting and vascularized osteomyocutaneous flaps from fibula, and iliac crest or ribs [1,2]. Each of these techniques has its advantages and disadvantages, and the choice of treatment depends on various factors, such as the size and location of the bone defect, the presence of infection or soft-tissue damage, the patient’s age, overall health, and the availability of resources and expertise. Improper management can result in deformity, non-union, recurrent infections, and other complications, and in some cases, amputation may be necessary to prevent further damage or infection. Soft-tissue coverage is critical for open fractures because it helps to reduce the risk of infection, promotes wound healing, and supports bone healing [3]. Early and appropriate plastic surgery for open fractures to obtain soft-tissue coverage before any bony reconstruction is a crucial step in the management of such injuries. It can help to reduce the risk of complications, promote healing, and improve patient outcomes. When a bone defect is combined with a fracture-related infection, the chances of successful bone consolidation and infection clearance are reduced leading to non-union or delayed union causing severe morbidity to the patient. Literature denotes that there is no single technique at present which is optimally successful in the management of large bone defects associated with complications. Therefore, the management should be individualized and tailored to the patient’s specific needs and circumstances.
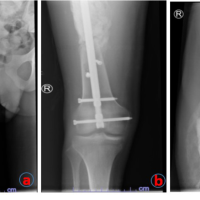
A 29-year-old male Gustilo Anderson type IIIB open tibial segmental fracture to the right leg with exposed large bone segment of tibia shaft following a high-velocity road traffic accident (Fig. 1a). Radiographs of the right leg showed segmental fracture of the tibia AO type 42C2 and fracture of the fibula 42A3 (Fig. 1b). Emergency right leg wound debridement was done by the Senior Orthopedic Surgeon. Loose bone fragments without soft-tissue attachments were excised – a large segment of bone of about 17.2 cm length had to be removed (Fig. 1c). To serve as a guide for leg length, fibula titanium elastic nailing was done by closed technique inserted from distal to proximal. Uniplanar uniaxial external fixator was applied to stabilize the tibia (Fig. 1d).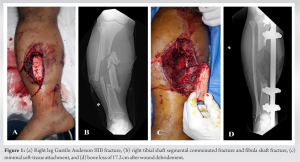 Four days after initial debridement, latissimus dorsi free flap cover for the soft-tissue defect was done by plastic surgical team which unfortunately got infected. The flap had to be debrided on post-operative day 6 and split skin grafting was done to cover defect. Once the split skin graft healed (Fig. 2a), at around 2 months post-injury, Ilizarov ring fixation and proximal tibia corticotomy were done. Bone transport was started after a week (Fig. 2b) and was transported for 4 months until the transported fragment reached the distal fragment (Fig. 2c). As is common in all large bone transport, there was invagination of soft tissues at the docked site (Fig. 2d).
Four days after initial debridement, latissimus dorsi free flap cover for the soft-tissue defect was done by plastic surgical team which unfortunately got infected. The flap had to be debrided on post-operative day 6 and split skin grafting was done to cover defect. Once the split skin graft healed (Fig. 2a), at around 2 months post-injury, Ilizarov ring fixation and proximal tibia corticotomy were done. Bone transport was started after a week (Fig. 2b) and was transported for 4 months until the transported fragment reached the distal fragment (Fig. 2c). As is common in all large bone transport, there was invagination of soft tissues at the docked site (Fig. 2d).  The invaginated soft tissues were excised and bone grafting was done at the docked site with realignment of Ilizarov frame. An additional foot frame was connected to improve stability of the bone. The patient was mobilized full weight-bearing with walker support and was on regular follow-up. Bone regenerate gradually consolidated and docking site also healed well (Fig. 3a). Ilizarov fixator and TENS fibula nail was removed and patellar tendon bearing cast was applied, which was retained for 1 month and then removed (Fig. 3b).
The invaginated soft tissues were excised and bone grafting was done at the docked site with realignment of Ilizarov frame. An additional foot frame was connected to improve stability of the bone. The patient was mobilized full weight-bearing with walker support and was on regular follow-up. Bone regenerate gradually consolidated and docking site also healed well (Fig. 3a). Ilizarov fixator and TENS fibula nail was removed and patellar tendon bearing cast was applied, which was retained for 1 month and then removed (Fig. 3b). 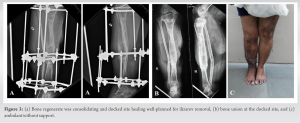 The series of events enumerated in Table 1. There was 1.5 cm shortening and equinus contracture of 10° present with excellent bone results and good functional results using the Association for the Study and Application of Methods of Ilizarov Scoring System [4]. The patient was walking well without support and has returned back to work (Fig. 3c).
The series of events enumerated in Table 1. There was 1.5 cm shortening and equinus contracture of 10° present with excellent bone results and good functional results using the Association for the Study and Application of Methods of Ilizarov Scoring System [4]. The patient was walking well without support and has returned back to work (Fig. 3c).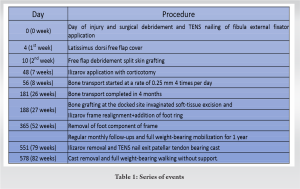
In Gustilo Anderson type IIIB injuries, devitalized soft tissues and loose bone fragments that do not have soft-tissue attachment need to be excised as these bony fragments get necrosed and act as a nidus of infection [5]. Bone transport using Ilizarov works on the principle of distraction osteogenesis which allows new bone and soft-tissue regeneration to fill the defect site [6]. Ilizarov frame helps in early weight-bearing causing loading on the bone which increases blood flow by 3–10 times in the extremity enhancing the local tissue level of antibiotics as well as rapid bone regenerate formation and soft-tissue healing [7]. Using bone transport, the regenerate is formed away from the already damaged site of trauma. Large bone defects can also be managed by Masquelet technique. Initially, a cement block is placed at the site of bone defect. This induces the formation of a membrane around the cement block at the site of bone defect which acts as a source of osteoprogenitor cells. Cement block is removed and filled with bone graft. For this technique to succeed, it is vital to have a good soft-tissue cover [8] and massive amount of graft is required to fill the large segmental defect and the time required for growth and maturation of the graft is relatively long. Free vascularized fibula grafting requires microvascular technique, needs an experienced surgeon and as well as the prolonged period of protected weight-bearing while waiting for graft hypertrophy. De Boer and Wood, in a study on 62 patients, found that hypertrophy of the vascularized bone grafts was 43% in 1 year follow-up and 80% after 2–3 year and only 32% in non-vascularized fibular bone grafts. This study reported 40% incidence of stress fractures within 8 months follow-up [9]. Shortening followed by gradual lengthening using IM lengthening nails is an another way to address bone defects and may aid in downgrading the soft-tissue defects. For acute shortening and gradual lengthening, the tibia can be shortened by 10% of its original length and the femur by 20% of its original length without any complications. This technique is not ideal for larger defects as it might cause kinking of the blood vessels and nerves [10]. Bowen and Widmaier investigated the incidence of infection following open fractures in patients classified according to the McPherson system. They found that immunocompromised patients were 2.86 times and severely immunocompromised patients were 5.72 times more likely to develop an infection following open fractures than normal host [11]. Bezstarosti et al. found that infection recurrence occurred in 8% of cases and amputation occurred in 3% of cases in their systematic review of 50 studies with fracture-related infections [1]. Often young surgeons are cautious to remove bony fragments which can potentially act as a source of infection. Adequate debridement of non-viable bone and soft tissues is one of the key step in reducing infections after open fractures. Soft-tissue coverage is critical for the success of bone reconstruction, as it provides a stable environment for bone healing and reduces the risk of infection. However, in some cases, the soft-tissue cover may fail, leading to complications such as infection, bone exposure, and delayed healing. The reasons for failed soft-tissue cover can vary, but common causes include poor wound management, inadequate blood supply, infections, and underlying patient health conditions such as diabetes or vascular disease. Once the cause of failure is identified, the treatment plan will depend on the severity and location of the bone loss. In some cases, a revision surgery such as such as skin grafting, local tissue flaps, or free tissue transfer may be needed. In cases where the soft-tissue coverage cannot be improved, the bone reconstruction technique which involves minimal internal fixations and minimal soft-tissue dissections is preferred. The bone reconstruction technique should be planned after assessing several factors such as size and site of defect, soft-tissue cover status, underlying infections, and patient comorbidities. The risk of infections is minimized by use of local antibiotics, minimal internal fixations, and avoiding multiple incisions to prevent extensive scarring. According to a systematic review by McMahon et al., open reduction internal fixation and IM nailing have higher rates of infection while circular external fixation offers the most satisfactory outcomes [12]. Systematic review by Papakostidis et al. has demonstrated that Ilizarov method of distraction osteogenesis significantly reduced the risk of deep infection in infected osseous lesions [13]. Rapid bone remodeling and hypertrophy requires mechanical loading on the bone [14], in which we can achieve early in Ilizarov technique and delayed weight-bearing is required in Masquelet technique and fibular graft technique to protect from stress fractures. Bone transport using Ilizarov technique is associated with complications such as pin tract infections and joint contractures leading to deformities. Patient compliance is required to be on external ring frame for long-term periods until bone regenerate consolidates and union of the docked site occurs. Daily pin tract care by patient and attenders is very important. However, ultimately the fracture healing is “biological.” The patient developed an equinus contracture only after foot frame was fixed to the distal tibial ring to improve stability during bone grafting of the docking fracture site after completion of bone transport. The ankle could not be moved for 6 months. Foot frame was removed retaining the distal tibial ring 6 months after bone grafting following which patient was noticed to have developed an equinus contracture. This emphasizes the importance of “keeping the joints moving” during any fracture treatment. The best method to prevent contractures is not by splinting alone but by actively and passively mobilizing adjacent joints. Even though the free flap had failed in the patient, distraction osteogenesis/histogenesis had definitely improved the blood supply to the bone and soft tissues as is evident by the excellent bone and soft-tissue healing.
Bone transport with Ilizarov method is a reliable technique of managing large bone defects even when soft-tissue cover is deficient. Early weight-bearing helps in rapid bone remodeling of the regenerated bone and helps in restoring the bone biology and can prevent the complications like stress fracture.
In large segmental bone loss with minimal soft-tissue cover, bone transport using Ilizarov technique can facilitate healing of soft tissues along with bone regeneration.
References
- 1.Bezstarosti H, Metsemakers WJ, van Lieshout EM, Voskamp LW, Kortram K, McNally MA, et al. Management of critical-sized bone defects in the treatment of fracture-related infection: A systematic review and pooled analysis. Archi Orthop Trauma Surg 2021;141:1215-30. [Google Scholar | PubMed]
- 2.Ferreira N, Tanwar YS. Systematic approach to the management of post-traumatic segmental diaphyseal long bone defects: Treatment algorithm and comprehensive classification system. Strategies Trauma Limb Reconstr 2020;15:106-16. [Google Scholar | PubMed]
- 3.VandenBerg J, Osei D, Boyer MI, Gardner MJ, Ricci WM, Spraggs-Hughes A, et al. Open tibia shaft fractures and soft-tissue coverage: The effects of management by an orthopaedic microsurgical team. J Orthop Trauma 2017;31:339-44. [Google Scholar | PubMed]
- 4.Paley D, Catagni MA, Argnani F, Villa A, Benedetti GB, Cattaneo R. Ilizarov treatment of tibial nonunions with bone loss. Clin Orthop Relat Res 1989;241:146-65. [Google Scholar | PubMed]
- 5.Swiontkowski MF. Criteria for bone debridement in massive lower limb trauma. Clin Orthop Relat Res1989;243:41-7. [Google Scholar | PubMed]
- 6.Ilizarov GA. The tension-stress effect on the genesis and growth of tissues: Part II. The influence of the rate and frequency of distraction. Clin Orthop Relat Res 1989;239:263-85. [Google Scholar | PubMed]
- 7.Aronson J. Temporal and spatial increases in blood flow during distraction osteogenesis. Clin Orthop Relat Res 1994;301:124-31. [Google Scholar | PubMed]
- 8.Masquelet AC, Fitoussi F, Begue T, Muller GP. Reconstruction of the long bones by the induced membrane and spongy autograft. Ann Chir Plast Esthet 2000;45:346-53. [Google Scholar | PubMed]
- 9.De Boer HH, Wood MB. Bone changes in the vascularised fibular graft. J Bone Joint Surg Br 1989;71:374-8. [Google Scholar | PubMed]
- 10.Tennyson M, Krzak AM, Krkovic M, Abdulkarim A. Cambridge protocol for management of segmental bone loss. J Orthop Case Rep 2021;11:45-50. [Google Scholar | PubMed]
- 11.Bowen TR, Widmaier JC. Host classification predicts infection after open fracture. Clin Orthop Relat Res 2005;433:205-11. [Google Scholar | PubMed]
- 12.McMahon SE, Little ZE, Smith TO, Trompeter A, Hing CB. The management of segmental tibial shaft fractures: A systematic review. Injury 2016;47:568-73. [Google Scholar | PubMed]
- 13.Papakostidis C, Bhandari M, Giannoudis PV. Distraction osteogenesis in the treatment of long bone defects of the lower limbs: Effectiveness, complications and clinical results; A systematic review and meta-analysis. Bone Joint J 2013;95:1673-80. [Google Scholar | PubMed]
- 14.Carter DR. Mechanical loading histories and cortical bone remodeling. Calcif Tissue Int 1984;36 Suppl 1:S19-24. [Google Scholar | PubMed]