Metallosis or the accumulation of metallic debris, is an uncommon complication of unicompartmental knee replacement surgery. It is important to always rule out infection as a potential cause and to consider one or two stages of surgical treatment as the gold standard for addressing this complication.
Dr. Ali Alayane, Department of Orthopedic surgery, Grand Hospital de l’Est Francilien - Meaux, France. Email: Alyane_ali@hotmail.com
Introduction: Metallosis following prosthetic hip and knee replacement is a well-known complication. However, unicompartmental knee arthroplasty (UKA) metallosis is rare. In this paper, we report a case of septic metallosis after unicompartmental knee replacement and we review the literature for the available treatment options.
Case Report: A 83-year-old female patient presented with left periprosthetic knee infection on the top of unicompartmental knee prosthesis three months after septic endocarditis that was treated with anti-biotherapy. Surgical exploration showed severe infected metallosis due to chronic polyethylene wear reaction; hence, management consisted of total synovectomy and debridement of all metallic debris and two stage revision.
Conclusion: Metallosis is a well-known complication after prosthetic hip and knee replacements. However, in UKA, it remains a rare complication where only few cases were reported in the literature.
Keywords: Metallosis, metal ions, unicompartmental knee replacement, prosthetic knee joint infection, knee joint, knee prosthesis, PE wear.
Metallosis following total hip and knee arthroplasty is a well-described complication in the literature [1]. However, unicompartmental knee arthroplasty (UKA) metallosis is uncommon, and it can be explained by different mechanisms: it can result from direct metal-on-metal (MoM) contact secondary to polyethylene (PE) wear, or the corrosion of the uncemented tibia plateau from the contact with the metallic screw fixation or the stemmed components [2]. The accumulation of metal ions in the articulation stimulates inflammatory cells and thereby induces inflammation process throughout the surrounding soft tissues [3,4]. Clinical presentation is unspecific and prosthetic joint infection should always be ruled out. Late complications include implant loosening, osteolysis, tissue necrosis, and pseudotumors. It may also induce neuropathy or cardiomyopathy [5]. Extensive synovectomy and removal of all metallic debris associated with one-stage exchange arthroplasty is commonly recommended for surgical treatment of knee arthroplasty metallosis [6,7]. The aim of this work is to present a case of septic left UKA metallosis and to review the current literature concerning the diagnosis and surgical treatment.
An 83-year-old female patient with multiple medical comorbidities presented to the emergency department for severe left knee pain and decrease range of motion. She is known to have a unicompartmental prosthesis implanted in her left knee 20 years ago with good functional and clinical follow-up. On physical examination, she had a swollen and erythematous knee, in addition to diffuse tenderness and remarkable pain throughout her arc of motion. 3 months before presentation, she had infectious endocarditis on her native aortic valve and spondylodiscitis. AP chest X-ray showed enlarged cardiac silhouette due to pericardial effusion (Fig. 1) and the germ that was isolated by cultures that time was methicillin-resistant Staphylococcus aureus (MRSA).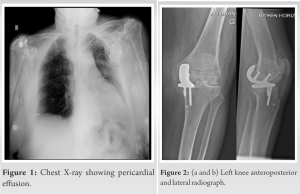 She was treated with intravenous and oral antibiotics for 3 months duration. AP and lateral left knee radiographs showed osteolysis of the medial femoral condyle without prosthetic loosening (Fig. 2). Blood tests showed high CRP level (207 g/L) and blood culture showed MRSA bacteremia. Serum chrome and Cobalt were not done and left knee scintigraphy showed abnormal hot spots in the left medial knee compartment all around the prosthesis. Aspiration of the knee joint yielded the growth of MRSA. Based on the clinical and paraclinical information, a diagnosis of periprosthetic joint infection was confirmed, and a decision to do a two-stage revision arthroplasty was taken. Utilizing the same old incision and through a medial parapatellar approach, surgical exploration showed diffuse infiltration of the synovial tissue throughout the knee with metallic debris (Fig. 3). Extensive synovectomy was done, and multiple specimens were sent for bacteriological and pathological analysis (Fig. 4).
She was treated with intravenous and oral antibiotics for 3 months duration. AP and lateral left knee radiographs showed osteolysis of the medial femoral condyle without prosthetic loosening (Fig. 2). Blood tests showed high CRP level (207 g/L) and blood culture showed MRSA bacteremia. Serum chrome and Cobalt were not done and left knee scintigraphy showed abnormal hot spots in the left medial knee compartment all around the prosthesis. Aspiration of the knee joint yielded the growth of MRSA. Based on the clinical and paraclinical information, a diagnosis of periprosthetic joint infection was confirmed, and a decision to do a two-stage revision arthroplasty was taken. Utilizing the same old incision and through a medial parapatellar approach, surgical exploration showed diffuse infiltration of the synovial tissue throughout the knee with metallic debris (Fig. 3). Extensive synovectomy was done, and multiple specimens were sent for bacteriological and pathological analysis (Fig. 4). 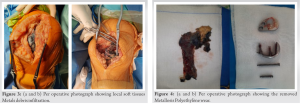 Medial unicompartmental knee prosthesis was removed and replaced by a cement spacer (Fig. 4). The patient was then hospitalized for IV antibiotics, and 6 weeks later, a second stage revision to implant a total knee prosthesis was done after confirming that the knee joint is clean of any infection. Left knee anteroposterior and lateral radiograph post-second stage revision are shown in Fig. 5.
Medial unicompartmental knee prosthesis was removed and replaced by a cement spacer (Fig. 4). The patient was then hospitalized for IV antibiotics, and 6 weeks later, a second stage revision to implant a total knee prosthesis was done after confirming that the knee joint is clean of any infection. Left knee anteroposterior and lateral radiograph post-second stage revision are shown in Fig. 5.  At 1-year post-operatively, she patient was free of symptoms with good functional and clinical outcome (Range of motion: 0–120°). Left knee anteroposterior and lateral radiograph at 1-year follow up are shown in Fig. 6.
At 1-year post-operatively, she patient was free of symptoms with good functional and clinical outcome (Range of motion: 0–120°). Left knee anteroposterior and lateral radiograph at 1-year follow up are shown in Fig. 6.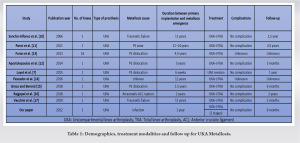
Metallosis is one of the most known and serious complications that can follow knee and hip arthroplasty [1]. In hip prosthesis, it can occur in cases where metal on metal designs is used, while in knee prosthesis, it is a consequence of a complication that was responsible for making the metallic tibial and femoral components in direct contact with each other [1]. Metallosis in knee prosthesis is usually caused by MoM friction, and this can never occur unless there is severe wear in the PE component, third body wear, friction between screws, and metallic tibial plateau of uncemented prosthetic designs and dislocation of PE when speaking about mobile-bearing designs [1]. It is usually caused by metallic debris infiltrating periprosthetic bone and soft tissues [8,9]. It can occur following both unicompartmental knee arthroplasty (UKA) and total knee arthroplasty (TKA), but it is more prevalent with TKA. Twenty-four cases of UKA metallosis are reported in the literature (Table 1) [7,10,11,12,13,14,15,16,17]. The most common cause of UKA metallosis was PE dislocation (19 cases); however, our case represents the first case of UKA metallosis secondary to prosthetic joint infection associated with PE wear. Several causes of PE wear were described in the literature, from them, incongruent articulating surfaces, a prosthesis that was implanted long time ago, resecting insufficient amount of bone on either side of the joint, and by that allowing only the utilization of thin PE component; in addition to flat PE configurations that decrease congruency and increase the rate of PE wear [18,19,20,21,22]. Furthermore, the weakening and exhaustion of the anterior cruciate ligament (ACL) when speaking about UKA will lead to the concentration of stress at a specific point of the PE, and consequently incurring its wear [18,23]. Accordingly . In addition to what is mentioned before, there is a vicious circle that knees go through when there is PE wear. As PE wears out during repetitive stress cycles or any of the mentioned reasons in medial UKA, the varus deformity will increase, and as the varus alignment becomes worse, there will be augmentation of the loads on the PE insert and whence increase its wear [22]. It is well known that osteolysis is also a consequence of PE wear, where PE debris will be phagocytosed by macrophages, and in there turn, macrophages will secrete some cytokines such as TNF alpha, IL1, and IL6 which have bone resorptive effects [24,25,26,27,28]. This is clear in our case, where we can see most of the medial femoral condyle being osteolysed. Nevertheless, several authors believe that UKA with mobile bearing designs have lower rates of PE wear, and not only that, but also these designs can even prevent failures associated with PE wear [19,22]. The diagnosis of metallosis is usually obscure, but sometimes, when it is severe enough it can be seen on plain X-rays involving soft tissues around the prosthesis [29]. This will aid surgeons in confirming the diagnosis and planning for the surgical procedure. Surgical treatment is the sole valid method of treatment when approaching post-arthroplasty metallosis; in addition, it should be done as soon as the diagnosis is confirmed. Rolf et al. recommended extensive synovectomy and bony debridement to remove all metallic debris and wear particles, thereby avoiding further bone destruction and osteolysis that is mediated by bone resorbing cytokines [30]. There are several reasons that highlight the importance of early diagnosis and treatment. As we have mentioned above, PE debris and metallosis by themselves are a cause of osteolysis, so the sooner the surgical treatment is provided, the better the outcomes will be at the level of bone stock. Second, high levels of metallic ions in the blood remain worrisome in terms of oncological and immunological levels [31]. Lastly, when revision surgery is done earlier, we could sometimes salvage the prosthesis by itself and just exchange the PE, while on the other hand, if surgical treatment is delayed, loosening and damage to the metallic components will arrive hence mandating both components revision [10]. All reported cases of UKA metallosis in the literature was treated with extensive synovectomy and conversion to TKA with good clinical and functional follow up (Table 1). However, for our patient, we did two stage exchange arthroplasties due to chronic prosthetic joint infection.
Metallosis after UKA is rare and few cases were reported in literature. Infection should be ruled out, and early diagnosis using radiographic, histological, and serum metal ions analyses is essential to prevent joint destruction and systemic extra-articular complications. Extensive surgical synovectomy and soft-tissue debridement should be always performed. Early-stage PE dislocation without prosthetic components damage could be treated with PE exchange; however, conversion to TKA results in good clinical and functional outcomes in cases of damaged components.
Two-stage revision of septic unicompartmental knee metallosis and conversion to total knee arthroplasty is a reasonable surgical treatment to achieve good clinical and functional outcomes.
References
- 1.Fehring KA, Fehring TK. Modes of failure in metal-on-metal total hip arthroplasty. Orthop Clin N Am 2015;46:185-92. [Google Scholar | PubMed]
- 2.Wolff M, Haasper C, Zahar A, Gauck C, Gehrke T, Citak M. Severe metallosis and elevated chromium in serum following implantation of the joint unloading implant system. Arch Orthop Trauma Surg 2017;137:1751-4. [Google Scholar | PubMed]
- 3.Mahendra G, Pandit H, Kliskey K, Murray D, Gill HS, Athanasou N. Necrotic and inflammatory changes in metal-on-metal resurfacing hip arthroplasties. Acta Orthop 2009;80:653-9. [Google Scholar | PubMed]
- 4.Matsushita I, Morita Y, Gejo R, Kimura T. Severe bone defects and reduced mineralization caused by massive metallosis after total knee arthroplasty: Histopathologic and bone morphometric findings. Mod Rheumatol 2007;17:507-10. [Google Scholar | PubMed]
- 5.Tower SS. Arthroprosthetic cobaltism associated with metal on metal hip implants. BMJ 2012;344:e430. [Google Scholar | PubMed]
- 6.Sharareh B, Phan DL, Goreal W, Schwarzkopf R. Metallosis presenting as knee pain 26 years after primary total knee arthroplasty. J Orthop Case Rep 2015;5:62-5. [Google Scholar | PubMed]
- 7.Luyet A, Fischer JF, Jolles BM, Lunebourg A. Unexpected wear of an unicompartimental knee arthroplasty in oxidized zirconium. Acta Orthop Belg 2015;81:790-5. [Google Scholar | PubMed]
- 8.Hart R, Janecek M, Bucek B. Case report of extensive metallosis in extra-articular tissues after unicompartmental knee joint replacement. Acta Chir Orthop Traumatol Cech 2003;70:47-50. [Google Scholar | PubMed]
- 9.Ottaviani G, Catagni MA, Matturri L. Massive metallosis due to metal-on-metal impingement in substitutive long-stemmed knee prosthesis. Histopathology 2005;46:237-8. [Google Scholar | PubMed]
- 10.Sanchis-Alfonso V. Severe metallosis after unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2007;15:361-4. [Google Scholar | PubMed]
- 11.Panni AS, Vasso M, Cerciello S, Maccauro G. Metallosis following knee arthroplasty: A histological and immunohistochemical study. Int J Immunopathol Pharmacol 2011;24:711-9. [Google Scholar | PubMed]
- 12.Apostolopoulos AP, Katsougrakis I, Fanous R, Harrison A, Saavedra E. Severe metallosis following polyethylene dislocation in a mobile-bearing medial unicompartmental knee replacement. J Long Term Eff Med Implants 2014;24:147-50. [Google Scholar | PubMed]
- 13.Foran JR, Brown NM, Valle CJ, Berger RA, Galante JO. Long-term survivorship and failure modes of unicompartmental knee arthroplasty. Clin Orthop Relat Res 2013;471:102-8. [Google Scholar | PubMed]
- 14.Pescador D, Calero-Paniagua I, Sánchez-González MD, Montilla C. Metallosis as a cause of pain and inflammation in a patient with a knee replacement: A case description. Reumatol Clin 2016;12:112-3. [Google Scholar | PubMed]
- 15.Greco N, Berend K. Polyethylene liner dislocation of fixed-bearing medial oxinium unicompartmental arthroplasty with severe metallosis. Knee 2018;25:341-5. [Google Scholar | PubMed]
- 16.Rajgopal A, Panda I, Tyagi VC. Early failure with massive metallosis and posteromedial wear following atraumatic anterior cruciate ligament rupture after medial unicompartmental knee arthroplasty. Arthroplast Today 2018;4:15-9. [Google Scholar | PubMed]
- 17.Vecchini E, Ditta A, Gelmini M, Maluta T, Valentini R, Ricci M, et al. Rupture of the femoral component and severe metallosis of the knee 10 years after unicompartmental knee arthroplasty (UKA): A case report. Acta Biomed 2019;90:198-202. [Google Scholar | PubMed]
- 18.Bartley RE, Stulberg SD, Robb WJ 3rd, Sweeney HJ. Polyethylene wear in unicompartmental knee arthroplasty. Clin Orthop Relat Res 1994;299:18-24. [Google Scholar | PubMed]
- 19.Murray DW, Goodfellow JW, O’Connor JJ. The Oxford medial unicompartmental arthroplasty. A ten-year survival study. J Bone Joint Surg 1998;80:983-9. [Google Scholar | PubMed]
- 20.Keblish PA. The case for unicompartmental knee arthroplasty. Orthopedics 1997;17:853-5. [Google Scholar | PubMed]
- 21.Palmer SH, Morrison PJ, Ross AC. Early catastrophic tibial component wear after unicompartmental knee arthroplasty. Clin Orthop Relat Res 1998;350:143-8. [Google Scholar | PubMed]
- 22.Psychoyios V, Crawford RW, O’Connor JJ, Murray DW. Wear of congruent meniscal bearings in unicompartmental knee arthroplasty: A retrieval study of 16 specimens. J Bone Joint Surg Br 1998;80:976-82. [Google Scholar | PubMed]
- 23.Engh GA, Ammeen D. Is an intact anterior cruciate ligament needed in order to have a well-functioning unicondylar knee replacement? Clin Orthop Relat Res 2004;428:170-3. [Google Scholar | PubMed]
- 24.Kadoya Y, Kobayashi A, Ohashi H. Wear and osteolysis in total joint replacements. Acta Orthop Scand Suppl 1998;278:1-16. [Google Scholar | PubMed]
- 25.Suggs JF, Li G, Park SE, Sultan PG, Rubash HE, Freiberg AA. Knee biomechanics after UKA and its relation to the ACL--a robotic investigation. J Orthop Res 2006;24:588-94. [Google Scholar | PubMed]
- 26.Berry DJ, Wold LE, Rand JA. Extensive osteolysis around an aseptic, stable, uncemented total knee replacement. Clin Orthop Relat Res 1993;293:204-7. [Google Scholar | PubMed]
- 27.Kim KJ, Kobayashi Y, Itoh T. Osteolysis model with continuous infusion of polyethylene particles. Clin Orthop Relat Res 1998;352:46-52. [Google Scholar | PubMed]
- 28.Whiteside LA. Polyethylene, osteolysis, and total joint replacement. Am J Knee Surg 1997;10:243. [Google Scholar | PubMed]
- 29.McGovern TF, Moskal JT. Radiographic evaluation of periprosthetic metallosis after total knee arthroplasty. J South Orthop Assoc 2002;11:18-24. [Google Scholar | PubMed]
- 30.Rolf O, Baumann B, Sterner T, Schutze N, Jakob F, Eulert J, et al. Characterization of mode II-wear particles and cytokine response in a human macrophage-like cell culture. Biomed Tech (Berl) 2005;50:25-9. [Google Scholar | PubMed]
- 31.Merritt K, Brown SA. Distribution of cobalt chromium wear and corrosion products and biologic reactions. Clin Orthop Relat Res 1996;329 Suppl:S233-43. [Google Scholar | PubMed]