To get familiar with an exceedingly rare type of osteosarcoma and it's management.
Dr. Ankith Chacko, Department of Orthopaedics, Rajagiri Hospital, Aluva, Kochi, Kerala, India. E-mail: ankithchacko02@gmail.com
Introduction: Periosteal osteosarcoma is a rare, intermediate-grade, malignant tumor arising on the surface of the bone. There are only a few numbers of periosteal osteosarcoma of fibula reported. However, there has never been a case concerning distal fibula recorded so far. Wide surgical removal is the commonly advised treatment. In the present report, we describe a case of periosteal osteosarcoma localized to the distal fibula, which was treated by wide resection and reconstruction of ankle mortise with the ipsilateral proximal fibula.
Case Report: The patient was a 48-year-old female who presented with ankle pain and swelling. A surface lesion, with “hair on end” periosteal reaction but without obvious medullary involvement, was seen on the distal fibular shaft by imaging studies. The diagnosis of periosteal sarcoma was confirmed with tru-cut biopsy. Wide resection and ankle mortise reconstruction with ipsilateral proximal fibula were done and 1 year of follow-up shows a good outcome.
Conclusion: Periosteal osteosarcoma is a well-defined pathological entity with characteristic radiological and histological features. It is essential to distinguish it from other surface osteosarcomas as treatment modalities are different. Controversy remains about the appropriate treatment of periosteal osteosarcoma. Reconstruction of ankle mortise with reversed proximal fibular autograft is a good option in low-to-intermediate-grade periosteal osteosarcoma of the distal fibula rather than going for extensive radical procedures or adding chemotherapy to the treatment regimen.
Keywords: Periosteal osteosarcoma, distal fibula, ankle mortise reconstruction.
Periosteal osteosarcoma is a rare variant of osteosarcoma. They account for <2% of all osteosarcomas. It is a surface osteosarcoma without medullary involvement [1]. The distal femur and proximal tibia, respectively, are the most common sites of origin, and they account for nearly 80% of cases. There are only a few periosteal osteosarcoma of fibula reported so far, most of which are proximal fibula. To our knowledge, this is the first case of periosteal osteosarcoma of the distal shaft of the fibula being reported. Wide surgical removal is the commonly advised treatment. These tumors have a lower propensity to metastasis and have a better prognosis than conventional osteosarcoma [2]. The benefit of adjuvant chemotherapy is doubtful. This report describes an exceedingly rare case of periosteal osteosarcoma localized to the distal fibula shaft in a lady, which was treated by wide resection and reconstruction of ankle mortise with the ipsilateral proximal fibula.
A 48-year-old female presented to our hospital on referral for evaluation and treatment for pain of the left ankle for approximately 3 months’ duration. She had no history of ankle or leg trauma, and her medical and family histories were unremarkable. The physical examination revealed mild swelling and edema over the lower leg and ankle, more towards the lateral aspect. Tenderness was present over the distal fibula. No neurovascular deficits noted. Ankle range of movement was full, with pain in the terminal range. No evidence of ipsilateral inguinal or popliteal adenopathy. General examination and other system examinations were within the normal limits. The laboratory data, including complete blood count, erythrocyte sedimentation rate, calcium, phosphorus, and alkaline phosphatase levels, were normal. Plain radiographs of her left ankle showed a coarse, perpendicular periosteal reaction with ‘’hair on end’’ pattern and thickening of the shaft of distal fibula (diaphyseal/metaphyseal) cortex, without scalloping or erosion (Fig. 1). 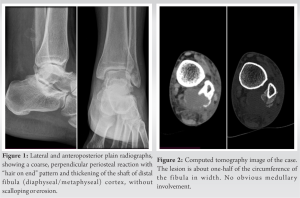 The lesion decreased in intensity from the cortical base (medullary surface) toward the surface. The cortex of the fibula was intact, and cortical scalloping was not seen. Computed tomography showed a lesion about one-half of the circumference of the fibula in width without obvious medullary involvement. The foci of mineralization was also seen and which was in continuation with the periosteal reaction (Fig. 2). Fig. 3 shows the Magnetic resonance imaging of the patient. The distal end of the fibular shaft for a length of 7 cm showed periosteal elevation on the posterior, lateral, and medial aspects. A 2.1 × 1.7 cm sized focus of lysis within the periosteal reaction was noted on the posteromedial aspect of this periosteal elevation. This focus appears heterogeneously T2 hyperintense, T1 hypointense with mild diffusion restriction. Mild diffuse edema was noted in the surrounding muscles of the posterior aspect of the leg.
The lesion decreased in intensity from the cortical base (medullary surface) toward the surface. The cortex of the fibula was intact, and cortical scalloping was not seen. Computed tomography showed a lesion about one-half of the circumference of the fibula in width without obvious medullary involvement. The foci of mineralization was also seen and which was in continuation with the periosteal reaction (Fig. 2). Fig. 3 shows the Magnetic resonance imaging of the patient. The distal end of the fibular shaft for a length of 7 cm showed periosteal elevation on the posterior, lateral, and medial aspects. A 2.1 × 1.7 cm sized focus of lysis within the periosteal reaction was noted on the posteromedial aspect of this periosteal elevation. This focus appears heterogeneously T2 hyperintense, T1 hypointense with mild diffusion restriction. Mild diffuse edema was noted in the surrounding muscles of the posterior aspect of the leg.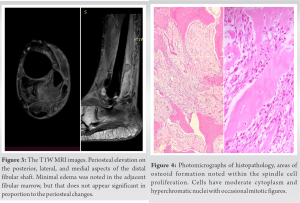 Minimal edema was noted in the adjacent fibular marrow, but that did not appear significant in proportion to the periosteal changes. Other visualized bones, joints, medial and lateral ligaments, and tendons around the ankle were normal. After initial evaluation and imaging studies, the initial differentials were metastatic disease and primary bone tumor. Ultrasonography (USG) abdomen, USG thyroid, and mammogram were done to rule out a primary in the breast, thyroid, and kidney, and were unremarkable, thus suspicion of a primary bone tumor was made. USG-guided tru-cut biopsy showed (Fig. 4) spindle-shaped cells arranged in sheets. The cells had moderate cytoplasm and hyperchromatic nuclei with occasional mitotic figures. Areas of osteoid formation were noted within the spindle cell proliferation. The histological features were consistent with periosteal osteosarcoma. Further, the patient underwent a metastatic workup (NCCT chest and Bone scan), and there was no evidence of metastasis. Hence, the patient was planned for resection with reconstruction. Wide excision (distal fibulectomy) and reconstruction of ankle mortise with ipsilateral proximal fibula done. Tumor was located at the distal fibula, 3 cm above the lateral malleolus. Surrounding muscle fibers were edematous. Wide excision of the tumor with adhered muscle fibers done. Biopsy tract excised en bloc with the specimen. Peroneus longus muscle saved, part of brevis excised. Proximal fibular cut taken 15 cm from the tip of the lateral malleolus (Imaging studies showed periosteal reaction up to 11.5 cm).
Minimal edema was noted in the adjacent fibular marrow, but that did not appear significant in proportion to the periosteal changes. Other visualized bones, joints, medial and lateral ligaments, and tendons around the ankle were normal. After initial evaluation and imaging studies, the initial differentials were metastatic disease and primary bone tumor. Ultrasonography (USG) abdomen, USG thyroid, and mammogram were done to rule out a primary in the breast, thyroid, and kidney, and were unremarkable, thus suspicion of a primary bone tumor was made. USG-guided tru-cut biopsy showed (Fig. 4) spindle-shaped cells arranged in sheets. The cells had moderate cytoplasm and hyperchromatic nuclei with occasional mitotic figures. Areas of osteoid formation were noted within the spindle cell proliferation. The histological features were consistent with periosteal osteosarcoma. Further, the patient underwent a metastatic workup (NCCT chest and Bone scan), and there was no evidence of metastasis. Hence, the patient was planned for resection with reconstruction. Wide excision (distal fibulectomy) and reconstruction of ankle mortise with ipsilateral proximal fibula done. Tumor was located at the distal fibula, 3 cm above the lateral malleolus. Surrounding muscle fibers were edematous. Wide excision of the tumor with adhered muscle fibers done. Biopsy tract excised en bloc with the specimen. Peroneus longus muscle saved, part of brevis excised. Proximal fibular cut taken 15 cm from the tip of the lateral malleolus (Imaging studies showed periosteal reaction up to 11.5 cm). 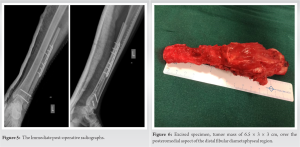 Ipsilateral proximal fibula exposed and harvested as an autograft. The head of the fibula was reversed and fixed to the lower tibia with two syndesmotic screws and fixed to the remaining shaft of the fibula using a 7 hole titanium plate with screws. Fig. 5 shows immediate postoperative radiographs. Excised specimen (Fig. 6) showed a tumor mass of 6.5 × 3 × 3 cm over the posteromedial aspect of the distal fibular dia-metaphyseal region accompanied by periosteal elevation. This lesion was located at a distance of 2 cm from the proximal and 7 cm from the distal bony margin. Cut section of the lesion showed gray white and myxoid areas. Histopathological evaluation showed a low-to-intermediate-grade periosteal osteosarcoma.
Ipsilateral proximal fibula exposed and harvested as an autograft. The head of the fibula was reversed and fixed to the lower tibia with two syndesmotic screws and fixed to the remaining shaft of the fibula using a 7 hole titanium plate with screws. Fig. 5 shows immediate postoperative radiographs. Excised specimen (Fig. 6) showed a tumor mass of 6.5 × 3 × 3 cm over the posteromedial aspect of the distal fibular dia-metaphyseal region accompanied by periosteal elevation. This lesion was located at a distance of 2 cm from the proximal and 7 cm from the distal bony margin. Cut section of the lesion showed gray white and myxoid areas. Histopathological evaluation showed a low-to-intermediate-grade periosteal osteosarcoma. Mitotic rates were 1–2/10 hpf. No areas of necrosis or lymphovascular invasion identified. Closest soft-tissue clearance was 0.5 cm. Both resected margins and skin were free of tumor. Pathologic stage was pT1. The patient had an uneventful postoperative recovery. Initially, the ankle was immobilised in a slab and later changed to below knee cast. Nonweight-bearing continued for 8 weeks, and after that, the patient mobilized on a weight-bearing cast for 4 more weeks. Follow-up radiographs at 6 months and 1 year (Fig. 7 and 8) showed adequate union and congruent ankle mortise. At 6 months and 1 year, the patient was evaluated with USG soft tissue of the left lower leg and NCCT chest, and both were found to be within normal limits and no evidence of local recurrence or metastasis detected. The patient has neither pain related to the surgical site nor difficulty in carrying out her activities of daily living. Fig. 9 shows clinical images of the patient’s limb at 1 year follow-up, demonstrating tiptoe standing, standing comfortably, and ankle range of movements with dorsiflexion and plantar flexion. At 1-year follow-up, her Foot and Ankle Disability Index Score is 82.7 and her American Foot and Ankle Score is 77 out of 100.
Mitotic rates were 1–2/10 hpf. No areas of necrosis or lymphovascular invasion identified. Closest soft-tissue clearance was 0.5 cm. Both resected margins and skin were free of tumor. Pathologic stage was pT1. The patient had an uneventful postoperative recovery. Initially, the ankle was immobilised in a slab and later changed to below knee cast. Nonweight-bearing continued for 8 weeks, and after that, the patient mobilized on a weight-bearing cast for 4 more weeks. Follow-up radiographs at 6 months and 1 year (Fig. 7 and 8) showed adequate union and congruent ankle mortise. At 6 months and 1 year, the patient was evaluated with USG soft tissue of the left lower leg and NCCT chest, and both were found to be within normal limits and no evidence of local recurrence or metastasis detected. The patient has neither pain related to the surgical site nor difficulty in carrying out her activities of daily living. Fig. 9 shows clinical images of the patient’s limb at 1 year follow-up, demonstrating tiptoe standing, standing comfortably, and ankle range of movements with dorsiflexion and plantar flexion. At 1-year follow-up, her Foot and Ankle Disability Index Score is 82.7 and her American Foot and Ankle Score is 77 out of 100.
Periosteal osteosarcoma is an intermediate-grade, malignant, cartilage and bone-forming neoplasm arising on the surface of bone. In contrast to the metaphyseal location of conventional osteosarcoma, periosteal osteosarcoma is predominantly diaphyseal or diaphyseal/metaphyseal in location [3]. The tumor initially was described in 1959 by Lichtenstein [4]. Unni et al. [5] in 1976 provided a detailed pathologic description. There are only a few numbers of periosteal osteosarcoma of fibula reported so far, and there are no cases of periosteal osteosarcoma of distal fibula reported in the literature. To our knowledge, this is the first case of periosteal osteosarcoma of the distal shaft of the fibula. The standard treatment recommended for conventional osteosarcoma consists of a combination of chemotherapy and surgery. It is essential to distinguish high grade surface osteosarcomas and parosteal osteosarcomas from periosteal osteosarcoma. As periosteal osteosarcoma is an intermediate-grade malignancy, sometimes chemotherapy is included in the treatment protocol. Periosteal osteosarcoma is considered to have a good prognosis with an overall 5 and 10 year survival of 89% and 83%, respectively, with approximately 15% of patients developing metastasis [6, 7]. Although the literature shows that adjuvant and neoadjuvant chemotherapy has increased the survival of patients with conventional osteosarcomas, the benefit of chemotherapy in periosteal osteosarcoma is doubtful, and several studies concluded that it does not improve the outcome or survival [6, 7, 8]. Controversy remains about the appropriate treatment of periosteal osteosarcoma. All agree that complete, wide surgical excision is mandatory for local control, but the role of chemotherapy is still debatable. The important factor which affects metastasis-free survival is the radical resection of the tumor, preventing local recurrence, which is known to be a risk factor for the subsequent development of metastatic disease. Grimer et al. [7] recommended chemotherapy when the tumor is of high grade. They reported 17 cases treated over 16 years. No patient has developed metastases, and no deaths have resulted from recurrence or metastasis of the tumour. They suggested that chemotherapy was valuable but emphasized the importance of complete surgical excision. In the presented case, the metastatic workup was negative. The histopathological evaluation was suggestive of an intermediate-grade periosteal osteosarcoma. As a mobile and stable ankle joint plays a paramount role in functional recovery, it was important to do a reconstruction of the ankle mortise along with wide excision rather than arthrodesis or amputation. With wide excision, we were able to achieve a disease-free margin. The available evidence from literature has failed to find any survival benefit from chemotherapy for periosteal osteosarcoma. As the case was an intermediate grade and wide excision showed a negative margin, chemotherapy was deferred for the patient. Regular follow-up done for evaluation of local recurrence and metastasis. 1 year follow-up has a good functional outcome with no evidence of local recurrence or metastasis.
Periosteal osteosarcoma is a well-defined pathological entity with characteristic radiological and histological features. It is essential to distinguish it from other surface osteosarcomas as treatment modalities are different. Controversy remains about the appropriate treatment of periosteal osteosarcoma. The confusion is regarding whether to add chemotherapy along with wide local excision. There is a higher risk for local recurrence when complete excision is not achieved. The role of neo or adjuvant chemotherapy is unclear, and available evidence has failed to find any survival benefit from chemotherapy for low to intermediate types of periosteal osteosarcoma. For cases with high-grade areas or medullary involvement, a combination of chemotherapy and wide surgical resection may benefit. Reconstruction of ankle mortise with reversed proximal fibular autograft is a good option in cases of low-to-intermediate-grade type of periosteal osteosarcoma of distal fibula rather than going for extensive radical procedures or adding chemotherapy to the treatment regimen.
- The periosteal osteosarcoma is a rare intermediate-grade malignant tumor.
- The distal fibula is a rare site for metastasis and even for primary bone tumor. In the literature, we could not find a case report concerning periosteal osteosarcoma of the distal fibula.
- It is essential to distinguish high-grade surface osteosarcomas and parosteal osteosarcomas from periosteal osteosarcoma, as the treatment modalities are different.
- Reconstruction of ankle mortise with proximal fibular autograft, along with resection of the tumor is a good option in cases of low-to-intermediate-grade type of periosteal osteosarcoma of the distal fibula.
References
- 1.Liu XW, Zi Y, Xiang LB, Han TY. Periosteal osteosarcoma: A review of clinical evidence. Int J Clin Exp Med 2015;8:37-44. [Google Scholar]
- 2.Chan CM, Lindsay AD, Spiguel AR, Gibbs CP Jr., Scarborough MT. Periosteal osteosarcoma: A single-institutional study of factors related to oncologic outcomes. Sarcoma 2018;2018:8631237. [Google Scholar]
- 3.Murphey MD, Jelinek JS, Temple HT, Flemming DJ, Gannon FH. Imaging of periosteal osteosarcoma: Radiologic-pathologic comparison. Radiology 2004;233:129-38. [Google Scholar]
- 4.Lichtenstein L. Tumors of periosteal origin. Cancer 1955;8:1060-9. [Google Scholar]
- 5.Unni KK, Dahlin DC, Beabout JW, Ivins JC. Parosteal osteogenic sarcoma. Cancer 1976;37:2466-75. [Google Scholar]
- 6.Cesari M, Alberghini M, Vanel D, Palmerini E, Staals EL, Longhi A, et al. Periosteal osteosarcoma: A single-institution experience. Cancer 2011;117:1731-5. [Google Scholar]
- 7.Grimer RJ, Bielack S, Flege S, Cannon SR, Foleras G, Andreeff I, et al. Periosteal osteosarcoma – A European review of outcome. Eur J Cancer 2005;41:2806-11. [Google Scholar]
- 8.Rose PS, Dickey ID, Wenger DE, Unni KK, Sim FH. Periosteal osteosarcoma: Long-term outcome and risk of late recurrence. Clin Orthop Relat Res 2006;453:314-7. [Google Scholar]










