Using photodynamic device intraoperatively as a technique to tamponade acute bleeding from hypervascular pathologic fractures.
Dr. Shalin S Patel, Department of Orthopedic Surgery, University of Texas MD Anderson Cancer Center, P.O. Box 301402, Unit 1448 Houston, Texas 77230-1402, United States. E-mail: sspatel@mdanderson.org
Introduction: Hypervascular tumors such as renal and thyroid carcinoma have a significant risk of intraoperative bleeding. To help mitigate bleeding, interventional preoperative embolization is traditionally used; however, it is success is highly variable. This is the first case report to discuss using expandable balloon implants with a minimally invasive approach to achieve fracture fixation and tamponade acute intraoperative bleeding.
Case Report: A 48-year-old male with clear-cell renal cell carcinoma presented with a left humeral shaft pathologic fracture. The patient was scheduled to undergo open biopsy, curettage of tumor, and fracture fixation with an intramedullary device. Intraoperatively, during open biopsy and curettage, brisk bleeding was encountered, which ceased after inserting an intramedullary photodynamic bone stabilization implant (IlluminOss). The implant’s balloon expanded to the diameter of the humerus allowing for tamponade, fracture stability, and a minimally invasive approach.
Conclusion: We present a possible intraoperative option for achieving control of bleeding in pathologic long bone fractures by deploying a photodynamic stabilization device. The method described can have applications in specific patients and obviate the need for pre-operative embolization for highly vascular tumors due to the implant’s ability to create tamponade within the bone.
Keywords: Photodynamic bone stabilization, IlluminOss, Pathologic fracture, Tamponade, Renal cell carcinoma, Hemorrhage.
The primary pathology in about 80% of skeletal metastasis is from prostate, breast, lung, renal, or thyroid cancers [1]. The humerus is one of the most common sites for metastasis, after the spine and femur [2,3]. Metastases are frequent in renal neoplasms, with an incidence of 30% [3]. Surgical prophylactic or fracture fixation of long bones is commonly done to minimize pain, increase patient mobility, and provide easier access to other medical management, such as radiation or chemotherapy, if required. Surgical approach and fixation methods vary widely based on the patient-specific factors and tumor type [4]. The photodynamic bone stabilization system (PBSS), developed by IlluminOss Medical Inc., is a percutaneous light-curable polymer contained within an inflatable balloon catheter. It offers customizable intramedullary stabilization for long bone fractures. The device received initial approval in 2009 from the European regulatory authority for use in osteoporotic patients. In 2017, the European Union Registry reported the initial success of the procedure in 149 fractures [5]. Due to its versatility, the device gained popularity in the oncologic community. In 2018, it was approved by The United States Food and Drug Administration for the treatment of impending and actual pathological fractures of the humerus, radius, and ulna resulting from metastatic bone disease [6,7]. In addition to fracture stabilization, pre-operative embolization of hypervascular tumors such as renal and thyroid carcinoma has been well described [8,9]. The goal is to help mitigate bleeding. The mortality risk increases by about 7% per unit of transfused blood [10]. However, prior studies have shown interventional pre-operative embolization to be highly variable and success ranging from 30% to 80% [9]. This case report describes using PBBS a minimally invasive approach to achieve fracture fixation and tamponade of acute intraoperative bleeding [11].
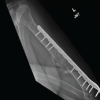
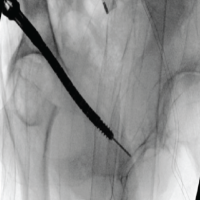
The patient was a 48-year-old male with oligometastatic renal clear cell carcinoma to the pancreatic body. He presented for the evaluation of atraumatic progressive left arm pain for 2 weeks. Radiographs showed a left pathologic midshaft humeral fracture (Fig. 1).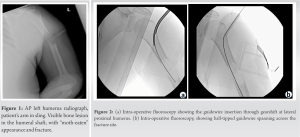 Radiotracer uptake of the left humerus was seen on bone scan. We discussed with the patient the risks and benefits of pre-operative embolization. We proceeded with intervention without embolization due to his significant instability at the fracture site, pain, and minimal soft-tissue tumor component [11,12]. We discussed with the patient that given his medical history of oligometastatic disease, a biopsy would be beneficial along with fracture stabilization. The surgical plan was to perform an open biopsy frozen section analysis. If the biopsy was consistent with metastatic carcinoma, we planned for left humerus curettage of the tumor and stabilization of his left pathologic humeral shaft fracture with an intramedullary implant [2]. Due to the hypervascular nature of this tumor histology, multiple points of large-bore peripheral access and an arterial line were placed by the anesthesia team. Given the increased complexity involved with pathologic fracture fixation, a standard humeral intramedullary nail system, humeral plating system, and PBSS were available. The patient was positioned supine on Jackson table, and a 3cm incision was made utilizing a mini-open anterolateral approach to the humeral shaft to take an intra-operative biopsy. The frozen section pathology appeared to be grossly abnormal, consistent with metastatic clear-cell renal cell carcinoma. After the frozen section analysis yielded a diagnosis of metastatic carcinoma, curettage of the tumor was performed through the same open biopsy site. During curettage, significant bleeding was encountered. The patient’s hemodynamics was monitored closely, and the patient was resuscitated appropriately. The patient’s blood loss from the mini-open biopsy was not unexpected, and both the surgical and anesthesia teams were prepared with multiple units of blood ready in the room. Most large diameter humeral nails are around 10 mm [13]. Given the width of the lytic metastatic lesion in our patient, there was a concern about having no control of bleeding at the fracture site due to the bleeding from dead space that cannot be filled quickly after standard intramedullary rod placement. The use of a plate system in an acute setting is limited by the amount of soft-tissue dissection required to reach the area of concern. An intra-operative decision was made to achieve hemostasis and fracture fixation with an expandable device [14]. Fluoroscopy was utilized to identify the lateral portion of the proximal humerus distal to the greater tuberosity, which allowed for the protection of the rotator cuff insertion during the approach. An incision was made proximal to the course of the axillary nerve. Careful dissection of the deltoid allowed for access to the proximal humerus. A threaded guidewire was inserted into the proximal humerus. The opening reamer was used to ream the lateral cortex of the proximal humerus for the PBSS implant. A 2.0 mm ball-tipped guidewire was inserted into the proximal humerus using a curved gearshift (Fig. 2a). This guidewire was inserted across the fracture site and into the distal fracture fragment (Fig. 2b). Anteroposterior (AP) and lateral fluoroscopy imaging was taken to ensure that the guidewire was in the bone both proximally and distally. The length of the IlluminOss implant was determined utilizing an external fluoroscopic ruler. To ensure the delivery sheath can be inserted, a minimum internal diameter of 7.0 mm must be achieved using the reamer [15]. A sheath was inserted over the ball-tipped guidewire, ensuring that the sheath went past the fracture site. Ball-tipped guidewire was removed. On the back table, the device was primed with monomer and prepared according to the manufacturer’s instructions. Before delivery to the surgical site, it is essential to cover the device from OR and room lights to maintain its integrity. The balloon was inserted through the sheath (Fig. 3a).
Radiotracer uptake of the left humerus was seen on bone scan. We discussed with the patient the risks and benefits of pre-operative embolization. We proceeded with intervention without embolization due to his significant instability at the fracture site, pain, and minimal soft-tissue tumor component [11,12]. We discussed with the patient that given his medical history of oligometastatic disease, a biopsy would be beneficial along with fracture stabilization. The surgical plan was to perform an open biopsy frozen section analysis. If the biopsy was consistent with metastatic carcinoma, we planned for left humerus curettage of the tumor and stabilization of his left pathologic humeral shaft fracture with an intramedullary implant [2]. Due to the hypervascular nature of this tumor histology, multiple points of large-bore peripheral access and an arterial line were placed by the anesthesia team. Given the increased complexity involved with pathologic fracture fixation, a standard humeral intramedullary nail system, humeral plating system, and PBSS were available. The patient was positioned supine on Jackson table, and a 3cm incision was made utilizing a mini-open anterolateral approach to the humeral shaft to take an intra-operative biopsy. The frozen section pathology appeared to be grossly abnormal, consistent with metastatic clear-cell renal cell carcinoma. After the frozen section analysis yielded a diagnosis of metastatic carcinoma, curettage of the tumor was performed through the same open biopsy site. During curettage, significant bleeding was encountered. The patient’s hemodynamics was monitored closely, and the patient was resuscitated appropriately. The patient’s blood loss from the mini-open biopsy was not unexpected, and both the surgical and anesthesia teams were prepared with multiple units of blood ready in the room. Most large diameter humeral nails are around 10 mm [13]. Given the width of the lytic metastatic lesion in our patient, there was a concern about having no control of bleeding at the fracture site due to the bleeding from dead space that cannot be filled quickly after standard intramedullary rod placement. The use of a plate system in an acute setting is limited by the amount of soft-tissue dissection required to reach the area of concern. An intra-operative decision was made to achieve hemostasis and fracture fixation with an expandable device [14]. Fluoroscopy was utilized to identify the lateral portion of the proximal humerus distal to the greater tuberosity, which allowed for the protection of the rotator cuff insertion during the approach. An incision was made proximal to the course of the axillary nerve. Careful dissection of the deltoid allowed for access to the proximal humerus. A threaded guidewire was inserted into the proximal humerus. The opening reamer was used to ream the lateral cortex of the proximal humerus for the PBSS implant. A 2.0 mm ball-tipped guidewire was inserted into the proximal humerus using a curved gearshift (Fig. 2a). This guidewire was inserted across the fracture site and into the distal fracture fragment (Fig. 2b). Anteroposterior (AP) and lateral fluoroscopy imaging was taken to ensure that the guidewire was in the bone both proximally and distally. The length of the IlluminOss implant was determined utilizing an external fluoroscopic ruler. To ensure the delivery sheath can be inserted, a minimum internal diameter of 7.0 mm must be achieved using the reamer [15]. A sheath was inserted over the ball-tipped guidewire, ensuring that the sheath went past the fracture site. Ball-tipped guidewire was removed. On the back table, the device was primed with monomer and prepared according to the manufacturer’s instructions. Before delivery to the surgical site, it is essential to cover the device from OR and room lights to maintain its integrity. The balloon was inserted through the sheath (Fig. 3a).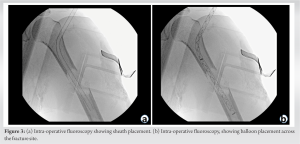 The sheath was then removed (Fig. 4a). AP and lateral fluoroscopy was utilized to ensure appropriate length, alignment, and rotation of the humerus (Fig. 3b). The FDA recommends a minimum canal diameter of 13 mm for the standalone use of the implant or a diameter <13 mm when used in conjunction with plates [15]. In this case, a 22 mm diameter balloon was chosen. The liquid monomer was injected into the balloon until maximum fit and fill were achieved. As the balloon expanded and the monomer filled, there was a noticeable decrease in bleeding due to the tamponade effect (Fig. 4b and Fig. 5a).
The sheath was then removed (Fig. 4a). AP and lateral fluoroscopy was utilized to ensure appropriate length, alignment, and rotation of the humerus (Fig. 3b). The FDA recommends a minimum canal diameter of 13 mm for the standalone use of the implant or a diameter <13 mm when used in conjunction with plates [15]. In this case, a 22 mm diameter balloon was chosen. The liquid monomer was injected into the balloon until maximum fit and fill were achieved. As the balloon expanded and the monomer filled, there was a noticeable decrease in bleeding due to the tamponade effect (Fig. 4b and Fig. 5a).  The light source was activated, delivering 436 NM visible light intramedullary. The cure time for the polymerization process ranges from 300 to 1000 s, depending on the size of the balloon [15]. This process initiated an exothermic reaction, causing the device to eventually set at body temperature (Fig. 4c). Finally, the balloon was cut following standard manufacturer instructions. To help provide rotational control, large fragment cortical nonlocking screws were placed utilizing a freehand percutaneous technique with the assistance of fluoroscopy. A single screw was placed lateral to medial in the proximal humerus. A single screw was placed anterior to posterior in the distal humerus. This completed the treatment of humeral shaft fracture with the insertion of an intramedullary implant with locking screws (Fig. 5b).
The light source was activated, delivering 436 NM visible light intramedullary. The cure time for the polymerization process ranges from 300 to 1000 s, depending on the size of the balloon [15]. This process initiated an exothermic reaction, causing the device to eventually set at body temperature (Fig. 4c). Finally, the balloon was cut following standard manufacturer instructions. To help provide rotational control, large fragment cortical nonlocking screws were placed utilizing a freehand percutaneous technique with the assistance of fluoroscopy. A single screw was placed lateral to medial in the proximal humerus. A single screw was placed anterior to posterior in the distal humerus. This completed the treatment of humeral shaft fracture with the insertion of an intramedullary implant with locking screws (Fig. 5b).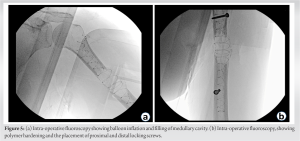
Bone metastases from renal cell carcinoma are very vascular and can cause significant intra-operative bleeding during open surgical approaches. Pre-operative embolization of vascular tumors has been a common practice for almost 20 years [16,17]. However, there are limitations in the efficacy of embolization based on tumor type, location, amount of soft tissue versus bone involvement, and location of feeding vessels [16,17]. In addition, sometimes, patient factors such as significant pain and instability at the fracture site require urgent surgical attention and do not allow for scheduled pre-operative embolization. Although rare, embolization involves some risks inherent to the procedure, arterial dissection; accidental embolization of adjacent vessels; muscle necrosis; transient paresthesia in the lower limbs (most common); and contrast nephropathy. Pre-operative embolization is dependent on interventional radiologist techniques and patient-specific factors [18]. Large systematic reviews have shown the effectiveness of embolization to be highly variable from 30% to 70% [9,19]. Current literature recommends that the open surgery be carried out at most three days after the embolization. After that, neo-angiogenesis occurs, and there is a new cumulative risk of bleeding [20]. Currently, if a patient does not receive or has a poor response to pre-operative embolization, the primary method of hemostasis in surgery is manual pressure, electrocautery, ligation (if vessels can be identified), and the utilization of products containing fibrin [21]. A randomized controlled trial has shown that open surgery without a method of control in hypervascular patients has shown increased average blood loss [22]. In particular, this is a risk in surgeries done through small percutaneous and mini-open approaches due to the difficulty to control brisk bleeding with limited visualization. This case report discusses a novel method of using an expandable intramedullary device to help tamponade intra-operative bleeding in the management of long bone metastases. A retrospective study involving 70 femur fractures treated with rigid intramedullary fixation demonstrated that the diameter of the nail and the ratio of the nail diameter to the medullary canal were directly correlated with intraoperative bleeding [23]. Photodynamic implants have the ability to conform to the shape of the medullary canal, providing a maximal fit within the intramedullary space [24]. PBSS’s entry point is less strictly defined than for rigid nails [13]. The implantation of the device does not inhibit endosteal remodeling and angiogenesis. The cured polymer allows for the augmentation of fixation with additional screws and hardware [25]. In situ, polymerization of the monomer to form a stable implant occurs at the surgeons’ discretion by applying blue light. Once hardened, the implant provides immediate stabilization and mechanical strength at the fracture site. Similar to traditional intramedullary devices, PBSS has the capability to provide primary stability [5,26]. Biomechanical and compatibility studies have indicated that the cured polymer possesses a modulus of elasticity similar to that of bone, and it does not elicit a significant tissue reaction [26,27]. The monomer is contained within the delivery balloon, ensuring no extravasation risk at the fracture site [28]. Moreover, post-operative imaging displays minimal artifacts, facilitating improved observation of tumor recurrence and bone union. In terms of basic scientific literature, there is evidence demonstrating that visible blue light emitted by the PBSS device can result in a temporary reduction of S. aureus based on in vitro testing [29]. Multiple long-term studies have demonstrated the successful implementation of PBSS in the elderly patients with long bone fractures [5,6,7,30]. In a retrospective study involving 105 procedures and a 2-year follow-up, comparing PBSS to traditional fixation methods for pathologic humerus fractures, no statistical difference was found in the reoperation rate and hardware durability between intramedullary nails (IMN) and PBSS. However, rigid intramedullary nail showed a statistically significant lower rate of broken hardware compared to PBSS [31]. In cases where aggressive tumor phenotypes are associated with specific histologic diagnoses, additional hardware can be utilized along the length of the implant to provide supplementary stabilization. A retrospective case series involving 12 patients with a two-year follow-up, who underwent PBSS for pathologic humerus fractures, reported two cases of nail rupture occurring after the four-month mark. These cases were successfully treated by adding a plate for additional support [25].
With this case report, we present a possible intra-operative option for achieving control of bleeding in pathologic long bone fractures by deploying a photodynamic stabilization device. The method described can have applications in specific patients and obviate the need for pre-operative embolization for highly vascular tumors due to the implant’s ability to create tamponade within the bone. At present, there are no existing studies that specifically address the use of PBSS in acute hemorrhage settings as an intraoperative option for achieving bleeding control in pathologic long bone fractures. Therefore, it is recommended that surgeons thoroughly assess patient-specific factors, urgency of the situation, operative technique, and the availability of local hemostatic agents before considering the adoption of this technique.
Hypervascular tumors associated with pathologic fractures have a significant risk of acute intraoperative bleeding. This case report presents a detailed analysis of a novel surgical implementation of a photodynamic balloon device as a potential adjunct intra-operative management technique for acute bleeding.
References
- 1.Macedo F, Ladeira K, Pinho F, Saraiva N, Bonito N, Pinto L, et al. Bone metastases: An overview. Oncol Rev 2017;11:321. [Google Scholar | PubMed]
- 2.Frassica FJ, Frassica DA. Evaluation and treatment of metastases to the humerus. Clin Orthop Relat Res 2003;415:S212-8. [Google Scholar | PubMed]
- 3.Saad F, Lipton A, Cook R, Chen YM, Smith M, Coleman R. Pathologic fractures correlate with reduced survival in patients with malignant bone disease. Cancer 2007;110:1860-7. [Google Scholar | PubMed]
- 4.Coleman RE. Metastatic bone disease: Clinical features, pathophysiology and treatment strategies. Cancer Treat Rev 2001;27:165-76. [Google Scholar | PubMed]
- 5.Gausepohl T, Pennig D, Heck S, Gick S, Vegt PA, Block JE. Effective management of bone fractures with the illuminoss® photodynamic bone stabilization system: Initial clinical experience from the European Union registry. Orthop Rev (Pavia) 2017;9:6988. [Google Scholar | PubMed]
- 6.Perisano C, Greco T, Fulchignoni C, Maccauro G. The IlluminOss® system: A solution in elderly patients with upper limbs bone metastases. Eur Rev Med Pharmacol Sci 2022;26:119-26. [Google Scholar | PubMed]
- 7.Melkerson M. IlluminOss Photodynamic Bone Stabilization System. Silver Spring, MD, United States: Food and Drug Administration Center for Devices and Radiological Health; 2018. [Google Scholar | PubMed]
- 8.Görich J, Solymosi L, Hasan I, Sittek H, Majdali R, Reiser M. Embolization of bone metastases. Radiologe 1995;35:55-9. [Google Scholar | PubMed]
- 9.Geraets SEW, Bos PK, van der Stok J. Preoperative embolization in surgical treatment of long bone metastasis: a systematic literature review. EFORT Open Rev 2020;5:17-25. [Google Scholar | PubMed]
- 10.Janssen SJ, Braun Y, Ready JE, Raskin KA, Ferrone ML, Hornicek FJ, et al. Are Allogeneic Blood Transfusions Associated With Decreased Survival After Surgery for Long-bone Metastatic Fractures? Clin Orthop Relat Res 2015;473:2343-51 . [Google Scholar | PubMed]
- 11.Jernigan EW, Tennant JN, Esther RJ. Not all patients undergoing stabilization of impending pathologic fractures for renal cell carcinoma metastases to the femur need preoperative embolization. Clin Orthop Relat Res 2018;476:529-34. [Google Scholar | PubMed]
- 12.Kickuth R, Waldherr C, Hoppe H, Bonel HM, Ludwig K, Beck M, et al. Interventional management of hypervascular osseous metastasis: Role of embolotherapy before orthopedic tumor resection and bone stabilization. AJR Am J Roentgenol 2008;191:W240-7. [Google Scholar | PubMed]
- 13.Schwarz GM, Zak L, Hirtler L, Wozasek GE. Anatomical considerations of intramedullary humeral nailing and lengthening. J Clin Med 2020;9:806. [Google Scholar | PubMed]
- 14.Vegt P, Muir JM, Block JE. The photodynamic bone stabilization system: A minimally invasive, percutaneous intramedullary polymeric osteosynthesis for simple and complex long bone fractures. Med Devices (Auckl) 2014;7:453-61. [Google Scholar | PubMed]
- 15.IlluminOss Medical. Surgical Technique Guide Humerus, Radius and Ulna. East Providence, Rhode Island. Online Surgical Technique Guide PDF; 2019 [Google Scholar | PubMed]
- 16.Roscoe MW, McBroom RJ, St Louis E, Grossman H, Perrin R. Preoperative embolization in the treatment of osseous metastases from renal cell carcinoma. Clin Orthop Relat Res 1989;238:302-7. [Google Scholar | PubMed]
- 17.Van Tol KM, Hew JM, Links TP. Images in thyroidology. Embolization of a bone metastasis of follicular thyroid carcinoma. Thyroid 2000;10:621-2. [Google Scholar | PubMed]
- 18.Owen RJ. Embolization of musculoskeletal bone tumors. Semin Intervent Radiol 2010;27:111-23. [Google Scholar | PubMed]
- 19.Mavrogenis AF, Rossi G, Rimondi E, Papagelopoulos PJ, Ruggieri P. Embolization of bone tumors. Orthopedics 2011;34:303-10. [Google Scholar | PubMed]
- 20.Leenknegt B, Pesapane F, Huang D. Pre-operative trans-arterial embolization of a hypervascular bone metastasis. J Belg Soc Radiol 2019;103:9. [Google Scholar | PubMed]
- 21.Sileshi B, Achneck HE, Lawson JH. Management of surgical hemostasis: Topical agents. Vascular 2008;16 Suppl 1:S22-8. [Google Scholar | PubMed]
- 22.Chen Y, Tai BC, Nayak D, Kumar N, Chua KH, Lim JW, et al. Blood loss in spinal tumour surgery and surgery for metastatic spinal disease: A meta-analysis. Bone Joint J 2013;95-B:683-8. [Google Scholar | PubMed]
- 23.Yu X, Zhang H, Zhang X, Xu R, She Y, Yu Z, et al. Effects of the ratios of marrow cavity diameter to intramedullary nail diameter from different layers on blood loss during perioperative period for femoral intertrochanteric fractures. Medicine (Baltimore) 2019;98:e16936. [Google Scholar | PubMed]
- 24.Krumme J, MacConnell A, Wallace M, Aboulafia A, Jelinek J, Adams B, et al. Early experience in pathologic humerus fracture treated with the photodynamic bone stabilization system shows limitations related to patient selection. Orthopedics 2021;44:154-9. [Google Scholar | PubMed]
- 25.Zoccali C, Attala D, Pugliese M, di Uccio AS, Baldi J. The IlluminOss® photodynamic bone stabilization system for pathological osteolyses and fractures of the humerus: Indications, advantages and limits in a series of 12 patients at 24 months of minimum follow-up. BMC Musculoskelet Disord 2021;22:63. [Google Scholar | PubMed]
- 26.McSweeney AL, Zani BG, Baird R, Stanley JRL, Hayward A, Markham PM, et al. Biocompatibility, bone healing, and safety evaluation in rabbits with an IlluminOss bone stabilization system. J Orthop Res 2017;35:2181-90. [Google Scholar | PubMed]
- 27.Pieretti AC, Shapiro DD, Westerman ME, Hwang H, Wang X, Segarra LA, et al. Tumor diameter response in patients with metastatic clear cell renal cell carcinoma is associated with overall survival. Urol Oncol 2021;39:837.e9-17. [Google Scholar | PubMed]
- 28.Heck S, Gicki S, Rabiner B, Penne D. Initial clinical experiences with a photodynamic polymer (IlluminOss). Med Rev J Med Contin Educ Conf (German) 2012:15-6. [Google Scholar | PubMed]
- 29.Van Oijen GW, Croughs PD, Hagenaars T, Verhofstad MH, Van Lieshout EM. Antimicrobial effect of visible blue light used in a minimally invasive intramedullary fracture stabilization system. J Bone Jt Infect 2019;4:216-22. [Google Scholar | PubMed]
- 30.Vegt P, Verbruggen J, Gausepohl T, Vroemen JP, Schafer W, Pennig D, et al. The photodynamic bone stabilization system in the treatment of humerus fractures: A prospective clinical trial. Cureus 2018;10:e2809. [Google Scholar | PubMed]
- 31.Hoellwarth JS, Weiss K, Goodman M, Heyl A, Hankins ML, McGough R 3rd. Evaluating the reoperation rate and hardware durability of three stabilizing implants for 105 malignant pathologic humerus fractures. Injury 2020;51:947-54. [Google Scholar | PubMed]