TKA is an established model of moderate-to-severe pain that often requires opioids for post-operative pain management. This case reports the use of the NeuroCuple™ device, a patch based on nanotechnology, as an alternative to opioids.
Dr. Jacques E Chelly, Department of Anesthesiology and Perioperative Medicine, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania, United States. E-mail: chelje@anes.upmc.edu
Introduction: In response to the current opioid crisis, there is a great interest to develop non-pharmacologic approaches to post-operative pain management for patients undergoing total knee arthroplasty (TKA).
Case Report: We report a case of a patient whose post-operative pain following TKA was managed using the newly designed NeuroCuple™ device, a patch based on the use of nanotechnology. The NeuroCuple™ device was placed above the knee by the patient at home. The use of the NeuroCuple™ device allowed the patient completely avoid the use of any opioids at home.
Conclusion: Our report suggests that the use of the NeuroCuple™ device may represent an interesting alternative to opioids for the peri-operative management of pain following a primary, unilateral TKA.
Keywords: Primary knee arthroplasty, peri-operative pain management, nanotechnology.
Persistent post-operative opioid use has been established as a possible cause of opioid use disorder [1,2]. Therefore, the ability to offer non-opioid alternatives is of significant interest. Recently, the use of nanotechnology has been reported as a possible method to treat arthritis pain [3]. Here, we report the use of the newly designed NeuroCuple™ device (nCap Medical, Salt lake City, Utah) for the management of post-operative pain following a primary total knee arthroplasty (TKA) replacement. The proposed mechanism of action of the NeuroCuple™ is based on the concept that local pain is the result of inflammation, which is associated with an increase in local temperature/energy. The NeuroCuple™ contains nano-capacitances capable of absorbing local energy and is consequently able to decrease local inflammation and pain (Fig. 1).
Our patient was a male, 70-year-old, weight 107 kg, height 181 cm, who underwent a primary right total knee replacement on January 19, 2023. His medical history was remarkable for osteoarthritis of the right knee, hypertension, hyperlipidemia, diverticulosis, psoriatic arthritis, eczema, cataracts, left eye ptosis, benign prostatic hyperplasia, heart murmur, and a past fracture of the right ankle. The patient’s past surgical history included two right knee arthroscopies in 1993, anterior cruciate ligament reconstructive surgery in 1995, cataract surgery, and a tonsillectomy. Pre-operative medications included Lipitor 100 mg daily, hydrochlorothiazide 25 mg daily, potassium 10 mEq daily, apremilast 30 mg BID, and naproxen 660 mg BID that was stopped 7 days before the surgery. Before being transferred to the operating room, a right adductor canal block was performed using ultrasound and an injection of 15 mL of 0.5% ropivacaine. Surgery was performed under spinal anesthesia and propofol sedation. Following surgery, the patient’s pain was rated between 3 and 7 on the pain rating scale. Post-operative pain was managed with acetaminophen PO 1000 mg q8h, celecoxib PO 200 mg BID, and oxycodone 5–10 mg q 4 h PRN for breakthrough pain. In the hospital, the patient used a continuous passive motion machine. The patient was discharged home on post-operative day 2 (1/21) with a 1-time prescription of 44 pills of 5 mg of oxycodone to control 8/10 breakthrough pain at home for an additional 3–5 days.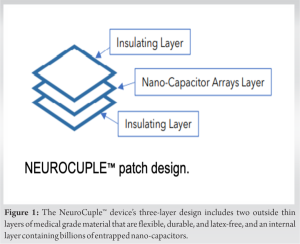 He was asked to continue taking celecoxib PO 200 mg BID and acetaminophen PO 1000 mg q8h. The patient’s opioid prescription was filled. At home, the patient placed a NeuroCuple™ device above the knee bandage (Fig. 2) and kept it in place from January 21 to February 6 (16 days). During this period, he did not require any opioids.
He was asked to continue taking celecoxib PO 200 mg BID and acetaminophen PO 1000 mg q8h. The patient’s opioid prescription was filled. At home, the patient placed a NeuroCuple™ device above the knee bandage (Fig. 2) and kept it in place from January 21 to February 6 (16 days). During this period, he did not require any opioids.
Although there is a consensus to reduce and sometime eliminate the use of opioids because of the ongoing opioid crisis and the documented associated risk of opioid use disorder in surgical patients, [4] most patients undergoing TKA are still prescribed a limited amount of opioids for breakthrough pain because evidence shows that the use of opioids facilitates immediate functional recovery following TKA [5]. Evidence supports the concept that complementary approaches, including acupuncture [6,7], auriculotherapy [8], hypnosis [9], and transcutaneous electrical nerve stimulation [10] may represent an alternative to opioid use in surgical patients. However, many reviews have questioned the validity of the effectiveness of these complementary approaches because the effectiveness of these techniques is based on anecdotal reports, and randomized placebo-controlled studies are lacking [11,12]. One report argued that acupuncture treatment is not superior to placebo [13]. In addition, these techniques require extensive expertise, which limits their use on a large scale. Nanotechnology has been shown to have several medical applications, including facilitating wound healing, the treatment of neurological and cardiac disorders [14,15,16], and the management of arthritic pain. Although evidence supporting the use of nanotechnology for pain associated with surgery is still lacking, the use of the NeuroCuple™ does not require extensive training and therefore represents a technique that can be used on a large scale and may represent an interesting alternative to the use of opioids in surgical patients undergoing skeletal-muscle procedures.
Although our data are encouraging, further research is required to confirm that the NeuroCuple™ device may represent an important and easy-to-use alternative to opioids to manage pain following surgery.
The use of nanotechnology may represent an interesting alternative to the use of opioids and may avoid the associated risk of opioid use disorder to manage pain following knee arthroplasty. The technology is non-invasive, easy-to-use, and well-tolerated.
References
- 1.Gudin JA, Dietze DT, Hurwitz PL. Improvement of pain and function after use of a topical pain relieving patch: Results of the RELIEF study. J Pain Res 2020;13:1557-68. [Google Scholar | PubMed]
- 2.Brummett CM, Waljee JF, Goesling J, Moser S, Lin P, Englesbe MJ, et al. New persistent opioid use after minor and major surgical procedures in US adults. JAMA Surg 2017;152:e170504. [Google Scholar | PubMed]
- 3.Kuck K, Naik BI, Domino KB, Posner KL, Saager L, Stuart AR, et al. Prolonged opioid use and pain outcome and associated factors after surgery under general anesthesia: A prospective cohort association multicenter study. Anesthesiology 2023;138:462-76. [Google Scholar | PubMed]
- 4.Munin MC, Rudy TE, Glynn NW, Crossett LS, Rubash HE. Early inpatient rehabilitation after elective hip and knee arthroplasty. JAMA 1998;279:847-52. [Google Scholar | PubMed]
- 5.Masood R, Mandalia K, Moverman MA, Puzzitiello RN, Pagani NR, Menendez ME, et al. Patients with functional somatic syndromes-fibromyalgia, irritable bowel syndrome, chronic headaches, and chronic low back pain-have lower outcomes and higher opioid usage and cost after shoulder and elbow surgery. Arthroscopy 2023;39:1529-38. [Google Scholar | PubMed]
- 6.Crespin DJ, Griffin KH, Johnson JR, Miller C, Finch MD, Rivard RL, et al. Acupuncture provides short-term pain relief for patients in a total joint replacement program. Pain Med 2015;16:1195-203. [Google Scholar | PubMed]
- 7.Lindsey MH, Mortensen S, Xu H, McNichol M, Abdeen A. The role of acupuncture in postoperative pain management of patients undergoing knee arthroplasty surgery: A systematic review and meta-analysis. JBJS Rev 2021;9. [Google Scholar | PubMed]
- 8.Usichenko TI, Lehmann Ch, Ernst E. Auricular acupuncture for postoperative pain control: A systematic review of randomised clinical trials. Anaesthesia 2008;63:1343-8. [Google Scholar | PubMed]
- 9.Fathi M, Ariamanesh AS, Joudi M, Joudi M, Sadrossadati F, Izanloo A. Hypnosis as an approach to control pain and anxiety in anterior cruciate ligament reconstruction and meniscal surgeries: Two case presentations. Anesth Pain Med 2019;9:e89277. [Google Scholar | PubMed]
- 10.Johnson MI, Paley CA, Jones G, Mulvey MR, Wittkopf PG. Efficacy and safety of transcutaneous electrical nerve stimulation (TENS) for acute and chronic pain in adults: A systematic review and meta-analysis of 381 studies (the meta-TENS study). BMJ Open 2022;12:e051073. [Google Scholar | PubMed]
- 11.Ko HF, Chen CH, Dong KR, Wu HC. Effects of acupuncture on postoperative pain after total knee replacement: Systematic literature review and meta-analysis. Pain Med 2021;22:2117-27. [Google Scholar | PubMed]
- 12.Sun Y, Gan TJ, Dubose JW, Habib AS. Acupuncture and related techniques for postoperative pain: A systematic review of randomized controlled trials. Br J Anaesth 2008;101:151-60. [Google Scholar | PubMed]
- 13.Plunkett A, McCoart A, Howard RS, Dennison E, Bartoszek M. A randomized, single-blind, prospective trial of auricular ‘battlefield’ acupuncture for the reduction of postoperative tonsillectomy pain in adults. Pain Manag 2018;8:287-95. [Google Scholar | PubMed]
- 14.Blanco-Fernandez B, Castaño O, Mateos-Timoneda MÁ, Engel E, Pérez-Amodio S. Nanotechnology approaches in chronic wound healing. Adv Wound Care (New Rochelle) 2021;10:234-56. [Google Scholar | PubMed]
- 15.Batool S, Nabipour H, Ramakrishna S, Mozafari M. Nanotechnology and quantum science enabled advances in neurological medical applications: Diagnostics and treatments. Med Biol Eng Comput 2022;60:3341-56. [Google Scholar | PubMed]
- 16.Jahed Z, Yang Y, Tsai CT, Foster EP, McGuire AF, Yang H, et al, Nanocrown electrodes for parallel and robust intracellular recording of cardiomyocytes. Nat Commun 2022;13:2253. [Google Scholar | PubMed]







