This article emphasizes the importance of clear communication and thorough documentation when dealing with uncommon medical cases, facilitating learning, knowledge sharing, and improved patient care among medical professionals.
Dr. Naveen Sathiyaseelan, Department of Orthopaedics, Saveetha Medical College and Hospital, Chennai, Tamil Nadu, India. E-mail: spnaveen17@gmail.com
Introduction: Children, especially those under the age of five, seldom get hip dislocations. Young children may sustain dislocations from minor accidents such as slips or falls from low heights, whereas adolescents typically do so from high-intensity events such as car crashes or collision sports. Posterior dislocation occurs 8–9 times more frequently than those in the anterior. Here, we describe about the acute posterior hip dislocation suffered by a 5-year-old boy in this case report.
Case Report: A 5-year-old girl reported to ER with left hip pain and difficulty to walk after slipping and falling while playing football at home. About 90 min after the fall, she presented at the hospital. The injured hip showed internal rotation, adduction, and flexion. An immediate pelvis X-ray revealed a right hip posterior dislocation. Under intravenous anesthesia, the dislocation was successfully reduced utilizing the Allis technique in the emergency room 3 h after the accident. Post-reduction radiographs verified that the reduction was successful. After 15 days of immobilization and 2 weeks of bilateral skin traction, the youngster was able to resume full weight-bearing walking with excellent tolerance.
Conclusion: To reduce the risk of avascular necrosis (AVN), pediatric hip dislocations require prompt reduction within 6 h. Soft-tissue injuries are found using post-reduction magnetic resource imaging. AVN requires constant observation for at least 2 years. Since traumatic hip dislocations in children under the age of five are rare, prompt diagnosis and treatment are essential.
Keywords: Pediatric dislocation, posterior hip dislocation, Allis technique.
Hip dislocations in children are infrequent, particularly in those under the age of five. Hip dislocations can occur in younger children as a result of minor accidents such as slips or falls from low heights, whereas hip dislocations in adolescents typically result from high-energy events such as collision sports or driving accidents. Children’s periosteum is thick, and their bones are supple and elastic, allowing them to withstand large forces since they are spongy [1]. Case reports of such dislocations in children under the age of five are extremely rare. The prevalence of posterior dislocations is roughly eight to nine times higher than that of anterior dislocations [2]. The affected limb typically adopts a position of adduction, flexion, and internal rotation in posterior hip dislocations, which frequently results in observable leg shortening in comparison to the unaffected leg [3]. A case study of a 5-year-old child who had a severe posterior hip dislocation is presented here. We also want to look at the literature that has already been written and talk about how our experience fits into what is already known about this subject.
A 5-year-old child who had fallen while playing football at home was sent to the emergency room complaining of left hip pain and being unable to walk. About 90 min after the fall, the child was admitted to the hospital. The infant was found to have a posterior hip dislocation after a clinical examination. Hip flexion, adduction, and internal rotation were all present in the injured hip (Fig. 1). No evidence of sciatic nerve damage was found during a neurological assessment. A posterior dislocation of the right hip was confirmed by an urgent pelvic X-ray (Fig. 2).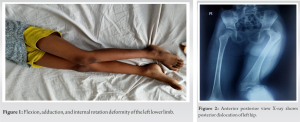 Using the Allis procedure (Fig. 3), the dislocation was effectively minimized in the emergency room within 3 h after the accident and with the help of intravenous sedation. To verify that the reduction was successful, post-reduction radiographs (Fig. 4) were taken.
Using the Allis procedure (Fig. 3), the dislocation was effectively minimized in the emergency room within 3 h after the accident and with the help of intravenous sedation. To verify that the reduction was successful, post-reduction radiographs (Fig. 4) were taken. Bilateral skin traction was used for 2 weeks following the reduction surgery. To rule out ligament injuries, a magnetic resource imaging (MRI) of the pelvis and both hips (Fig. 5 and 6) was performed, but only edematous alterations surrounding the hip joint were seen. The child was able to walk with full weight bearing and tolerated it remarkably well after a 15-day period of immobility.
Bilateral skin traction was used for 2 weeks following the reduction surgery. To rule out ligament injuries, a magnetic resource imaging (MRI) of the pelvis and both hips (Fig. 5 and 6) was performed, but only edematous alterations surrounding the hip joint were seen. The child was able to walk with full weight bearing and tolerated it remarkably well after a 15-day period of immobility.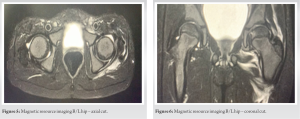
In children under the age of five, hip dislocation is still relatively uncommon. In children under the age of ten, traumatic hip dislocations (THD) commonly result from low-energy events such as falls or sports injuries. On the other hand, children older than ten are more likely to experience high-intensity traumas such as falls from great heights or car accidents. The more youthful the child, the less force is often needed to cause a dislocation, presumably because their soft tissues and bone structure are more elastic than those of adults [4]. There are four different forms of THD: Inferior, central, posterior, and anterior. THD is more frequently seen in boys than in girls, occurring three to four times more frequently in them [5]. The most frequent type of THD in pediatric age group is posterior dislocation. A quick closed reduction is the main course of treatment for THD, and it is normally carried out while the patient is sedated or under general anesthesia. The Allis procedure is the easiest, most popular, and most efficient way to achieve closure reduction of a posterior dislocation. The Bigelow, Stimson, and this procedure all rely on flexing the hip joint to loosen the iliofemoral ligament. The Allis technique, however, stands out as the most straightforward and widely used of the bunch. It is frequently stressed in numerous papers that rapid reduction within the “golden period” (about 6 h) is essential for the best results [6]. Open reduction should be taken into consideration if THD cannot be decreased using closed techniques. Closed reduction requires extreme vigilance to prevent forceful manipulation, which greatly increases the danger of iatrogenic physeal separation. In our situation, mild traction and little rotation were adequate to successfully decrease the joint [7]. A comprehensive physical examination should be performed after closed reduction to determine the hip’s stability. In addition, X-ray imaging should be done to verify that concentric reduction has been achieved. While MRI outperforms computed tomography (CT) in detecting soft tissues trapped within the joint, capsular lesions, and the health of surrounding muscles and tendons, CT is superior in evaluating bone and osteochondral lesions [8]. Regarding the immobilization technique, authors take a variety of approaches, using everything from skin traction to plaster casts. With the exception of recurrent dislocation, THD-related complications are less common in children than in adults. Children who experience recurrent dislocation frequently do so because of a deficiency or a slack joint capsule. Recurrent dislocations are more frequently observed in children who have endured <2 weeks of immobilization or who have been permitted early ambulation, according to the body of existing literature. THD can result in a number of problems in children, including coxa magna, sciatic nerve injury, post-traumatic arthritis, and femoral head avascular necrosis (AVN). More frequent complication is injury to sciatic nerve, according to recent studies. However, AVN has the worst prognosis of all complications [9]. The correlation between AVN and delayed reduction has long been known; prior studies showed that rates of AVN were 58% when reduction was done after 6 h, compared to 4.8% when it was done within 6 h [10]. Despite the fact that our study is limited to a single case with a limited follow-up, it offers important insights for the future research. Furthermore, we did not take functional or radiological outcome scores into account. We wanted to share our story and talk about how it related to the body of current material, but it is important to stress that this injury is uncommon in children.
AVN risk is reduced by lowering pediatric hip dislocations within 6 h, which is a medical emergency. In an operating room with visual guidance, closed reduction should first be tried; if it is unsuccessful, open reduction may be considered. The identification of related soft-tissue injuries depends heavily on post-reduction MRI. A minimum of 2 years of follow-up are required to check for AVN. In conclusion, although THDs in children under the age of five are uncommon, early detection and intervention are crucial.
The case report underscores the significance of immediate reduction of the dislocation within 6 h to minimize the risk of AVN, a severe complication that can arise from disrupted blood supply.
References
- 1.Balasubramanian N, Babu NG, Sindhuja P. Traumatic hip dislocation in a child younger than 3 years- a rare case report and review of literature. J Orthop Case Rep 2015;5:69-71. [Google Scholar | PubMed]
- 2.Yuksel S, Albay C. Early reduction of pediatric traumatic posterior hip dislocation is much more important than the treatment procedure. Pediatr Emerg Care 2019;35:e206-8. [Google Scholar | PubMed]
- 3.Archer JE, Balakumar B, Odeh A, Bache CE, Dimitriou R. Traumatic hip dislocation in the paediatric population: A case series from a specialist center. Injury 2021;52:3660-5. [Google Scholar | PubMed]
- 4.Salisbury RD, Eastwood DM. Traumatic dislocation of the hip in children. Clin Orthop Relat Res 2000;377:106-11. [Google Scholar | PubMed]
- 5.Mehlman CT, Hubbard GW, Crawford AH, Roy DR, Wall EJ. Traumatic hip dislocation in children. Long-term followup of 42 patients. Clin Orthop Relat Res 2000;376:68-79. [Google Scholar | PubMed]
- 6.Swiontkowski MF, Li M. Fractures and dislocations about the hip and pelvis. In: Green’s Skeletal Trauma in Children. Netherlands: Elsevier; 2015. p. 311-64. [Google Scholar | PubMed]
- 7.Vialle R, Odent T, Pannier S, Pauthier F, Laumonier F, Glorion C. Traumatic hip dislocation in childhood. J Pediatr Orthop 2005;25:138-44. [Google Scholar | PubMed]
- 8.Başaran SH, Bilgili MG, Erçin E, Bayrak A, Öneş HN, Avkan MC. Treatment and results in pediatric traumatic hip dislocation: Case series and review of the literature. Ulus Travma Acil Cerrahi Derg 2014;20:437-42. [Google Scholar | PubMed]
- 9.Pearson DE, Mann RJ. Traumatic hip dislocation in children. Clin Orthop Relat Res 1973;92:189-94. [Google Scholar | PubMed]
- 10.Hougaard K, Thomsen PB. Traumatic posterior dislocation of the hip--prognostic factors influencing the incidence of avascular necrosis of the femoral head. Arch Orthop Trauma Surg (1978) 1986;106:32-5. [Google Scholar | PubMed]










