This article proposes a surgical algorithm for early multi-ligament knee injury reconstruction in patients with ipsilateral floating knee injuries.
Dr. Samuel Eaddy, Department of Orthopaedics and Sports Medicine, Mercy Health St. Vincent Medical Center, Toledo, Ohio 43608, USA. E-mail: seaddy@mercy.com
Introduction: Ipsilateral fracture of the femur and tibia, known by the moniker “floating knee,” is a serious injury that primarily results from high-energy trauma. Up to 53% of patients with floating knee injuries have concurrent ligamentous injuries, with the anterior cruciate ligament (ACL) as the most commonly affected ligament. Approximately 10% of multi-ligament knee injuries consist of injuries to both the ACL and posterolateral corner (PLC); however, the literature reporting the management of this patient population is sparse, particularly, with a lack of consensus on the timing and protocol of surgical treatment. Well-characterized treatment guidelines are needed for patients with concomitant floating knee and multi-ligament knee injuries.
Case Report: A 26-year-old, previously healthy male involved in a high-speed motor vehicle collision presented with upper and lower extremity, skull, and facial fractures, sacropelvic dissociation, and epidural hematoma. Here we describe a rare instance of a floating knee with a multi-ligament knee injury treated through early reconstruction of the ACL, PLC, and anterolateral ligament following stabilization of long bone fractures. Post-injury day 18, the patient underwent single-stage reconstruction of his multi-ligament knee injury. The timing of this was chosen to allow for capsular scar formation to aid in arthroscopy.
Conclusion: Our surgical algorithm consists of allograft reconstruction using an all-inside ACL technique and a modified anatomical PLC technique. We recommend early (1–3 weeks) surgical treatment of multi-ligament knee injuries for patients without a closed head injury; however, an individualized treatment approach should be sought, considering the severity of ligamentous injuries, pre-injury activity level, extent of soft-tissue damage, and the activity goals of the patient post-injury. In patients with floating knee injuries, the proposed surgical algorithm here may be utilized for successful multi-ligament knee injury reconstruction.
Keywords: Multiligament knee injuries, floating knee, multiligament knee reconstruction, allograft, arthroscopy.
Ipsilateral fracture of the femur and tibia, known by the moniker “floating knee,” is a serious injury that primarily results from high-energy trauma [1,2]. Up to 53% of patients with floating knee injuries have concurrent ligamentous injuries [3], with the anterior cruciate ligament (ACL) as the most commonly affected ligament [4]. When a floating knee is associated with multi-ligament knee injuries (MKIs), defined as injury to two or more of the main ligaments of the knee, diagnostic and therapeutic challenges arise [5] due to a high incidence of concurrent life-threatening injuries and limb-threatening complications and morbidity [2,6]. Moreover, approximately 10% of MKIs consist of injuries to both the ACL and posterolateral corner (PLC) [7]. However, the literature reporting the management of this patient population is sparse, particularly with a lack of consensus on the timing and protocol of surgical treatment. Well-characterized treatment guidelines are needed for patients with concomitant floating knee and MKI. Here, we describe a surgical algorithm in a patient with MKIs involving the ACL, PLC, and anterolateral ligament (ALL).
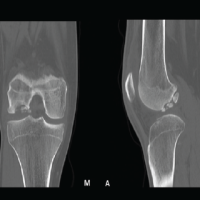
A 26-year-old, previously healthy male involved in a high-speed motor vehicle collision presented with upper and lower extremity, skull, and facial fractures, sacropelvic dissociation, and epidural hematoma. The patient was intubated on the scene. The patient underwent external fixation of bilateral femoral and tibial fractures, followed nine days later by retrograde femoral and tibial intramedullary nail (IMN) placement on the right side for fixation of his floating knee. Intraoperative radiographs demonstrated >10 mm of ligamentous laxity revealed by lateral gapping with varus stress in the anteroposterior plane [8]. Hyperextension of the knee in the sagittal plane was seen as well (Fig. 1). On magnetic resonance imaging, tears of the ACL, posterior cruciate ligament, lateral collateral ligament (LCL), popliteus tendon, and popliteofibular ligament, and slight attenuation of the medial collateral ligament were seen. Treatment for the left leg consisted of a retrograde femoral IMN and placement of an Ilizarov frame of the tibia. Table 1 summarizes the timing of surgical intervention for his bilateral lower extremity injuries.
On magnetic resonance imaging, tears of the ACL, posterior cruciate ligament, lateral collateral ligament (LCL), popliteus tendon, and popliteofibular ligament, and slight attenuation of the medial collateral ligament were seen. Treatment for the left leg consisted of a retrograde femoral IMN and placement of an Ilizarov frame of the tibia. Table 1 summarizes the timing of surgical intervention for his bilateral lower extremity injuries.
Multiligament knee reconstruction technique
On post-injury day 18, the patient underwent single-stage reconstruction of his MKI of the right knee. The timing of this was chosen to allow for capsular scar formation to aid in arthroscopy. Under anesthesia, the right knee was passively ranged 0–80°. After manipulation, a full range of motion was achieved. A grade 3 posterolateral instability of the knee, grade 3 Lachman’s [9], and a grade 3 pivot shift were also observed [10,11]. A lateral surgical approach was conducted, with tibial and fibular tunnels drilled according to LaPrade’s technique for PLC reconstruction [12]. Standard anterolateral and anteromedial arthroscopy portals were created for diagnostic purposes. Scarring of the superior pouch, grade 1 chondromalacia of the medial tibial plateau, and ACL avulsion at the tibial insertion site were noted. Any adhesions seen were lysed and ACL remnants were removed. For ACL reconstruction, an Arthrex FlipCutter (Arthrex Inc, Naples, FL, USA) guide was utilized to create a full-length tibial socket. This technique, however, was unsuccessful for a femoral socket due to the distal locking screws of the IMN. Therefore, an accessory medial portal technique was performed [13], through which a +7-mm Arthrex transportal guide was introduced to drill an independent femoral tunnel. This femoral tunnel was then reamed with a 9-mm reamer to a depth of 25-mm, dilated, and tapped with a 9.5-mm tap, creating a final tunnel of 9-mm × 25-mm. These dimensions were appropriate based on the 8.5-mm × 62-mm GraftLink (Arthrex Inc, Naples, FL, USA) that was going to be utilized as a graft. At this point, we proceeded with the lateral femoral dissection to address the PLC, and LaPrade’s technique [12] was continued for the dissection of the lateral femur. Of note, the ALL was found to be avulsed off its tibial insertion site. Two guide pins were placed: one at the LCL origin and one at the proximal fifth of the popliteus sulcus, 18-mm distal to the LCL origin. These pins were aimed anteromedially to avoid the femoral IMN. The popliteal tendon tunnel was placed at 30° in axial and coronal planes and the LCL tunnel was placed at 30° and 0° in axial and coronal planes, respectively [14]. A 6-mm reamer was used on the LCL origin, whereas a 5.5-mm reamer was used on the popliteus origin. These were key deviations from LaPrade’s technique [12], in which larger bone tunnels are normally created to allow for the placement of allograft and bone blocks. For this procedure, soft tissue grafts were used, allowing smaller tunnels to be created to avoid implants and other tunnels. As evidenced on arthroscopy, the lateral tunnels did not violate the femoral ACL tunnel. A tibialis anterior allograft was split longitudinally for use for both the LCL and the ALL, to avoid adding additional tunnels for an ALL graft. A semitendinosus allograft was then prepared for popliteus insertion (Fig. 2).  The tibialis anterior graft was docked in the previously created LCL tunnel using a biocomposite interference screw (Arthrex Inc, Naples, FL, USA). The semitendinosus graft was docked in the previously created popliteus tunnel utilizing the same method. Using standard graft-passing techniques, the LCL and popliteal graft arms were passed through their respective tunnels. The ACL was passed using the anteromedial portal passing technique [13], provisionally fixed with adjustable loop fixation buttons on both the femoral and tibial sides, and then tensioned at 30° of flexion. The LCL graft was also tensioned at 30° and a biocomposite interference screw was placed into the fibular tunnel for fixation. The semitendinosus graft and the remaining tibialis anterior graft from the LCL arm were passed from posterior to anterior through the tibial tunnel, recreating the popliteofibular and popliteus ligaments. The knee was then flexed to 60°, standard valgus stress was applied, and a 9-mm peek TunneLoc (Biomet, Warsaw, IN, USA) was inserted to achieve tibial fixation. Next, the ALL graft was passed superficially to the lateral structures proximally and attached to Gerdy’s tubercle using an 8-mm × 20-mm bone staple (Arthrex Inc, Naples, FL, USA) in a posteromedial direction. Throughout placement of the allograft, extreme care was taken to avoid violation of the articular surface and PLC tunnel (Fig. 3). All wounds were closed in standard fashion.
The tibialis anterior graft was docked in the previously created LCL tunnel using a biocomposite interference screw (Arthrex Inc, Naples, FL, USA). The semitendinosus graft was docked in the previously created popliteus tunnel utilizing the same method. Using standard graft-passing techniques, the LCL and popliteal graft arms were passed through their respective tunnels. The ACL was passed using the anteromedial portal passing technique [13], provisionally fixed with adjustable loop fixation buttons on both the femoral and tibial sides, and then tensioned at 30° of flexion. The LCL graft was also tensioned at 30° and a biocomposite interference screw was placed into the fibular tunnel for fixation. The semitendinosus graft and the remaining tibialis anterior graft from the LCL arm were passed from posterior to anterior through the tibial tunnel, recreating the popliteofibular and popliteus ligaments. The knee was then flexed to 60°, standard valgus stress was applied, and a 9-mm peek TunneLoc (Biomet, Warsaw, IN, USA) was inserted to achieve tibial fixation. Next, the ALL graft was passed superficially to the lateral structures proximally and attached to Gerdy’s tubercle using an 8-mm × 20-mm bone staple (Arthrex Inc, Naples, FL, USA) in a posteromedial direction. Throughout placement of the allograft, extreme care was taken to avoid violation of the articular surface and PLC tunnel (Fig. 3). All wounds were closed in standard fashion.
Here, we describe early ligamentous reconstruction in a rare case of a polytrauma patient presenting with fractures of the distal femoral and tibial shaft with concomitant MKI of the ipsilateral knee consisting of grade III ACL and PLC tears. The key features of our treatment approach include an early MKI reconstruction after long bone fracture stabilization using allograft in an all-inside ACL technique and a modified anatomical PLC technique. Our surgical algorithm for early MKI reconstruction is outlined in Fig. 4. The first step consists of tibial preparation using a lateral approach to drill tibial and fibular tunnels for PLC reconstruction. This is followed by diagnostic arthroscopy in which the ACL femoral socket is created using an accessory medial portal technique. An ACL tibial socket is created followed by LCL, ALL, and popliteus femoral tunnels. Femoral graft fixation is then performed. With the tibialis anterior autograft docked in the femoral LCL socket, the LCL graft is split to utilize a two-tailed technique to create LCL and ALL limbs. A semitendinosus autograft is docked in the femoral popliteus socket. During tibial graft fixation, ACL graft is passed through both the femur and tibia and fixed; the LCL graft is docked in the fibular tunnel; the popliteus and remaining LCL grafts are passed through the tibia and fixed; the ALL graft is fixed. Previous studies have reported a delay of up to 12–24 months in the diagnosis of knee ligamentous injury after the initial traumatic event in patients with ipsilateral femoral fracture, tibial fracture, or both [15-18]. Thus, a delay in the diagnosis of MKI may further delay treatment, negatively impacting the patient’s prognosis. Our treatment approach involved diagnostic imaging of ligamentous injury a few days after initial fracture stabilization. This allowed for the determination of the exact knee ligamentous lesions to devise a surgical treatment plan early. Currently, there is no consensus regarding the appropriate timing for the treatment of knee ligament injuries. A systematic review by Levy et al. compared early versus late surgery of damaged knee ligaments and reported that early treatment resulted in a higher mean Lysholm score (90 vs. 82, respectively), higher percentage of excellent/good International Knee Documentation Committee scores (45% vs. 31%, respectively), and higher sports activity scores based on the Knee Outcome Survey (89 vs. 69, respectively) [19-21]. In contrast, Sabesan et al. recommend delaying the treatment of MKI until the tibial fracture is healed [22]. Moreover, they found that nonoperative treatment can provide good patient satisfaction and adequate functional outcomes in the absence of symptoms of ligamentous instability. We recommend early (1–3 weeks) surgical treatment of MKI for patients without a closed head injury; however, an individualized treatment approach should be sought, considering the severity of ligamentous injuries, pre-injury activity level, extent of soft-tissue damage, and the activity goals of the patient post-injury [22,23]. Our surgical algorithm involves reconstruction of the ALL which is often debated. However, a recent biomechanical analysis by Spencer et al. [24] demonstrated that the ALL is a clinically significant secondary stabilizer along with the ACL, the primary stabilizer to anterolateral rotation. In this case, ALL reconstruction was performed considering our patient’s significant pivot shift test results and Segond fracture. In this patient, we used allograft to reconstruct the ACL and PLC due to the large variety of sizes and types of allografts available and its ability to reduce operative time and site morbidity during MKI reconstruction [25-27]. Some studies suggest a higher risk of failure, rejection, and infection with the use of allografts compared to autografts, yet both types have resulted in comparable outcomes post-MKI treatment [28,29]. The main limitation of this study is the lack of reported long-term follow-up and outcome results. Nonetheless, we believe that our treatment algorithm may improve outcomes in appropriately selected patients.
Our treatment approach involved diagnostic imaging of ligamentous injury a few days after initial fracture stabilization. This allowed for the determination of the exact knee ligamentous lesions to devise a surgical treatment plan early. Currently, there is no consensus regarding the appropriate timing for the treatment of knee ligament injuries. A systematic review by Levy et al. compared early versus late surgery of damaged knee ligaments and reported that early treatment resulted in a higher mean Lysholm score (90 vs. 82, respectively), higher percentage of excellent/good International Knee Documentation Committee scores (45% vs. 31%, respectively), and higher sports activity scores based on the Knee Outcome Survey (89 vs. 69, respectively) [19-21]. In contrast, Sabesan et al. recommend delaying the treatment of MKI until the tibial fracture is healed [22]. Moreover, they found that nonoperative treatment can provide good patient satisfaction and adequate functional outcomes in the absence of symptoms of ligamentous instability. We recommend early (1–3 weeks) surgical treatment of MKI for patients without a closed head injury; however, an individualized treatment approach should be sought, considering the severity of ligamentous injuries, pre-injury activity level, extent of soft-tissue damage, and the activity goals of the patient post-injury [22,23]. Our surgical algorithm involves reconstruction of the ALL which is often debated. However, a recent biomechanical analysis by Spencer et al. [24] demonstrated that the ALL is a clinically significant secondary stabilizer along with the ACL, the primary stabilizer to anterolateral rotation. In this case, ALL reconstruction was performed considering our patient’s significant pivot shift test results and Segond fracture. In this patient, we used allograft to reconstruct the ACL and PLC due to the large variety of sizes and types of allografts available and its ability to reduce operative time and site morbidity during MKI reconstruction [25-27]. Some studies suggest a higher risk of failure, rejection, and infection with the use of allografts compared to autografts, yet both types have resulted in comparable outcomes post-MKI treatment [28,29]. The main limitation of this study is the lack of reported long-term follow-up and outcome results. Nonetheless, we believe that our treatment algorithm may improve outcomes in appropriately selected patients.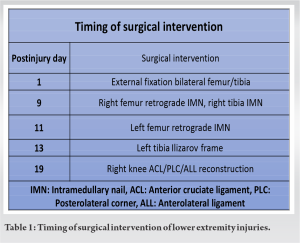
Here, we describe a rare instance of a floating knee with multi-ligament knee injury treated with reconstruction of the ACL, PLC, and ALL following stabilization of long bone fractures. We recommend early (1–3 weeks) surgical treatment of multi-ligament knee injuries for patients without a closed head injury; however, an individualized treatment approach should be sought, considering the severity of ligamentous injuries, pre-injury activity level, extent of soft-tissue damage, and the activity goals of the patient post-injury. Our proposed surgical algorithm consists of allograft reconstruction using an all-inside ACL technique and a modified anatomical PLC technique. In patients with floating knee injuries, the proposed surgical algorithm here may be utilized for successful multi-ligament knee injury reconstruction.
Well-characterized treatment guidelines are needed for patients with concomitant floating knee and multi-ligament knee injuries. In this case report, we describe a surgical algorithm for a patient with ipsilateral floating knee and multi-ligament knee injuries involving early reconstruction of the ACL, PLC, and ALL following fixation of the femur and tibia fractures.
References
- 1.Veith RG, Winquist RA, Hansen ST Jr. Ipsilateral fractures of the femur and tibia. A report of fifty-seven consecutive cases. J Bone Joint Surg Am 1984;66:991-1002. [Google Scholar | PubMed]
- 2.Nouraei MH, Hosseini A, Zarezadeh A, Zahiri M. Floating knee injuries: Results of treatment and outcomes. J Res Med Sci 2013;18:1087-91. [Google Scholar | PubMed]
- 3.Vallier HA, Manzano GW. Management of the floating knee: Ipsilateral fractures of the femur and tibia. J Am Acad Orthop Surg 2020;28:e47-54. [Google Scholar | PubMed]
- 4.Bertrand ML, Andrés-Cano P. Management of the floating knee in polytrauma patients. Open Orthop J 2015;9:347-55. [Google Scholar | PubMed]
- 5.Ng JW, Myint Y, Ali FM. Management of multiligament knee injuries. EFORT Open Rev 2020;5:145-55. [Google Scholar | PubMed]
- 6.Goyal A, Tanwar M, Joshi D, Chaudhary D. Practice guidelines for the management of multiligamentous injuries of the knee. Indian J Orthop 2017;51:537-44. [Google Scholar | PubMed]
- 7.Munoz Vives J, Bel JC, Capel Agundez A, Chana Rodriguez F, Palomo Traver J, Schultz-Larsen M, et al. The floating knee: A review on ipsilateral femoral and tibial fractures. EFORT Open Rev 2016;1:375-82. [Google Scholar | PubMed]
- 8.Manske RC, Prohaska D. Physical examination and imaging of the acute multiple ligament knee injury. N Am J Sports Phys Ther 2008;3:191-7. [Google Scholar | PubMed]
- 9.Torg JS, Conrad W, Kalen V. Clinical diagnosis of anterior cruciate ligament instability in the athlete. Am J Sports Med 1976;4:84-93. [Google Scholar | PubMed]
- 10.Galway HR, MacIntosh DL. The lateral pivot shift: A symptom and sign of anterior cruciate ligament insufficiency. Clin Orthop Relat Res 1980;147:45-50. [Google Scholar | PubMed]
- 11.Larson RL. Physical examination in the diagnosis of rotatory instability. Clin Orthop Relat Res 1983;172:38-44. [Google Scholar | PubMed]
- 12.LaPrade RF, Johansen S, Wentorf FA, Engebretsen L, Esterberg JL, Tso A. An analysis of an anatomical posterolateral knee reconstruction: An in vitro biomechanical study and development of a surgical technique. Am J Sports Med 2004;32:1405-14. [Google Scholar | PubMed]
- 13.Lubowitz JH, Ahmad CS, Anderson K. All-inside anterior cruciate ligament graft-link technique: Second-generation, no-incision anterior cruciate ligament reconstruction. Arthroscopy 2011;27:717-27. [Google Scholar | PubMed]
- 14.Gelber PE, Erquicia JI, Sosa G, Ferrer G, Abat F, Rodriguez-Baeza A, et al. Femoral tunnel drilling angles for the posterolateral corner in multiligamentary knee reconstructions: Computed tomography evaluation in a cadaveric model. Arthroscopy 2013;29:257-65. [Google Scholar | PubMed]
- 15.Walker DM, Kennedy JC. Occult knee ligament injuries associated with femoral shaft fractures. Am J Sports Med 1980;8:172-4. [Google Scholar | PubMed]
- 16.Chahal J, Dhotar HS, Zahrai A, Whelan DB. PCL reconstruction with the tibial inlay technique following intra-medullary nail fixation of an ipsilateral tibial shaft fracture: A treatment algorithm. Knee Surg Sports Traumatol Arthrosc 2010;18:777-80. [Google Scholar | PubMed]
- 17.Thiagarajan P, Ang KC, Das De S, Bose K. Ipsilateral knee ligament injuries and open tibial diaphyseal fractures: Incidence and nature of knee ligament injuries sustained. Injury 1997;28:87-90. [Google Scholar | PubMed]
- 18.Van Raay JJ, Raaymakers EL, Dupree HW. Knee ligament injuries combined with ipsilateral tibial and femoral diaphyseal fractures: The “floating knee”. Arch Orthop Trauma Surg 1991;110:75-7. [Google Scholar | PubMed]
- 19.Levy BA, Dajani KA, Whelan DB, Stannard JP, Fanelli GC, Stuart MJ, et al. Decision making in the multiligament-injured knee: An evidence-based systematic review. Arthroscopy 2009;25:430-8. [Google Scholar | PubMed]
- 20.Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med 1982;10:150-4. [Google Scholar | PubMed]
- 21.Agel J, LaPrade RF. Assessment of differences between the modified Cincinnati and international knee documentation committee patient outcome scores: A prospective study. Am J Sports Med 2009;37:2151-7. [Google Scholar | PubMed]
- 22.Sabesan VJ, Danielsky PJ, Childs A, Valikodath T. Multiligament knee injuries with associated tibial plateau fractures: A report of two cases. World J Orthop 2015;6:363-8. [Google Scholar | PubMed]
- 23.Skendzel JG, Sekiya JK, Wojtys EM. Diagnosis and management of the multiligament-injured knee. J Orthop Sports Phys Ther 2012;42:234-42. [Google Scholar | PubMed]
- 24.Spencer L, Burkhart TA, Tran MN, Rezansoff AJ, Deo S, Caterine S, et al. Biomechanical analysis of simulated clinical testing and reconstruction of the anterolateral ligament of the knee. Am J Sports Med 2015;43:2189-97. [Google Scholar | PubMed]
- 25.Fanelli GC, Tomaszewski DJ. Allograft use in the treatment of the multiple ligament injured knee. Sports Med Arthrosc Rev 2007;15:139-48. [Google Scholar | PubMed]
- 26.Harner CD, Olson E, Irrgang JJ, Silverstein S, Fu FH, Silbey M. Allograft versus autograft anterior cruciate ligament reconstruction: 3-to 5-year outcome. Clin Orthop Relat Res 1996:134-44. [Google Scholar | PubMed]
- 27.Sun K, Tian SQ, Zhang JH, Xia CS, Zhang CL, Yu TB. Anterior cruciate ligament reconstruction with bone-patellar tendon-bone autograft versus allograft. Arthroscopy 2009;25:750-9. [Google Scholar | PubMed]
- 28.Mariscalco MW, Magnussen RA, Mehta D, Hewett TE, Flanigan DC, Kaeding CC. Autograft versus nonirradiated allograft tissue for anterior cruciate ligament reconstruction: A systematic review. Am J Sports Med 2014;42:492-9. [Google Scholar | PubMed]
- 29.Zeng C, Gao SG, Li H, Yang T, Luo W, Li YS, et al. Autograft versus allograft in anterior cruciate ligament reconstruction: A meta-analysis of randomized controlled trials and systematic review of overlapping systematic reviews. Arthroscopy 2016;32:153-63.e18. [Google Scholar | PubMed]