Irrespective of its size of posterior malleolus fragment, fixation is necessary along with syndesmotic screw, if syndesmosis is unstable.
Dr. Sanket Tanpure, Department of Orthopaedics, Dr. Vithalrao Vikhe Patil Medical College, Ahmednagar, Maharashtra, India. E-mail: sankettanpure55@gmail.com
Introduction: Syndesmotic injury in trimalleolar fracture is necessary to address intraoperatively by stability test, as it affects post-operative functional outcomes. Most of syndesmotic injuries are stable after fixation of the posterior malleolus, but in rare cases, syndesmosis is not stable after adequate fixation. In those rare conditions, we have to fix syndesmosis by corticocancellous (CC) screw throw lateral fibula plate. We emphasize this complex problem and offer solutions to overcome it.
Case Report: Case 1: A 45-year-old male suffered significant trauma to his right ankle from a slip and fall, resulting in a trimalleolar fracture. The open reduction and internal fixation (ORIF) throw posterolateral approach was performed after wrinkles were seen on the ankle. A four-hole Ellis plate was used in antiglide mode to reduce posterior malleolar fragments. The lateral malleolus is fixed with a 7-hole, 1/3-locking tubular plate with a tricortical syndesmotic CC screw. The medial malleolus was internally fixed by a 6-hole LC-DCP. Case 2: A 49-year-old female suffered significant trauma to her right ankle from a domestic fall, resulting in a trimalleolar fracture. The ORIF throw posterolateral approach was performed after wrinkles were seen on the ankle. A four-hole Ellis plate was used in antiglide mode to reduce posterior malleolar fragments. The lateral malleolus is fixed with an 8-hole, 1/3-locking tubular plate with a tricortical syndesmotic CC screw. The medial malleolus was internally fixed by a 2 CC screw with an 8-hole LC-DCP. The anterior distal tibia fragment was fixed with a 16-mm anteroposterior CC screw.
Conclusion: In a trimalleolar ankle fracture, fixation of the posterior malleolus is important for a better post-operative functional outcome, irrespective of the size of the posterior malleolus. The author recommends lateral fibula plate fixation by creating a window between the skin and the peroneus longus and brevis tendon, so we have a chance to put a syndesmotic screw into the lateral plate if syndesmosis is not stable.
Keywords: Trimalleolar ankle fracture, syndesmotic injury, posterolateral approach, ORIF.
In ankle fractures, posterior malleolar fracture prevalence is approximately 14–44% [1, 2]. The posteromedial tibial plafond or the posterior tubercle of the distal tibia is commonly involved [3]. A rotational ankle injury causes the most common type of posterior malleolar fracture, which involves the posterior tubercle and leads to a posterior inferior tibiofibular ligament (PITFL) avulsion [4]. When a larger fracture fragment of the posterior malleolus along with the posteromedial side is involved, it leads to axial loading on the ankle mortise, and also posterior shearing pressures are transmitted to it [3]. There has been much discussion on how to treat posterior malleolus fractures for a very long time. The size of the fragment on the lateral radiograph was used to determine whether fixation was necessary or not. The criteria for fixation stated that there should be a displacement of more than 2 mm and a quarter to a third involvement of the articular surface [5]. There has been a paradigm shift away from this way of thinking in recent years. The significance of fibular notch congruence and posterior syndesmosis stability has been emphasized [6]. The posterior malleolus can now be fixed using the posterolateral technique as a viable option [7]. Open reduction and internal fixation surgery is an approved method for treating fractures of the medial and lateral malleolus. Because it is anticipated that when open reduction of the lateral malleolus is carried out, posterior malleolus fractures will spontaneously reduce, they are commonly left untreated [8]. A posterior fragment makes it more difficult for surgeons to reduce the joint anatomically [2]. In this article, surgical techniques for fixing syndesmotic ligament injury along with posterior malleolus and fibula by posterolateral approach will be discussed.
We presented a short series of two patients who were operated at our institution in July 2022. All of us operated with a single posterolateral incision for fixation of the posterior and lateral malleolus, along with syndesmotic injury. Media malleolus is fixed by medial incision over distal tibia.
Case 1
A 45-year-old male suffered significant trauma to his right ankle by slip and fall resulting in a trimalleolar fracture of the distal tibia (Fig. 1). Below-knee slab applied to casualty. Local ice application, limb elevation over the BB frame, and medication are used to reduce swelling. The patient operated on day 7 after wrinkles were seen on the ankle. The ankle was approached from the posterolateral side (Fig. 2a) with the patient in a prone position for treating posterior malleolar fractures and other related fibular fractures. In this method, the muscles of the peroneus brevis and flexor halluces longus are dissected in the intermuscular plane, all the way to the tibia and fibula. To expose the syndesmosis and the posterior malleolus, the flexor halluces longus muscle belly is raised from behind the distal tibia. Anatomical reduction of the post-malleolar portion to the tibia was done. Typically, a four-hole ellis plate is used in antiglide mode to reduce posterior malleolar fragments. A window was created between the lateral skin flap and the peroneus longus and brevis tendon (Fig. 2b). Lateral malleolus fractures are exposed and reduced well by bone-holding forceps. The lateral malleolus is fixed with a 7-hole, 1/3-locking tubular plate. An external rotating stressor was applied to all syndesmoses before closure by the surgeon using a small Hohmann retractor placed in the interosseous region. Through direct observation and fluoroscopically distal tibiofibular articulation, stability was evaluated. Our criteria for determining appropriate stability was that under stress, the superior clear space deviation from the medial clear space never exceeded more than 1 mm and the tibiofibular articulation had diastasis <1 mm [9]. We observed that syndesmosis was not stable, which was not a usually happen after fixation of the posterior malleolus. The distal fragment 2nd screw was replaced by a tricortical syndesmotic screw, and stability was again confirmed under fluoroscopy. We believe that in terms of wound healing, this method is a more physiological way of dissecting, as the incision is sutured over muscle and not on bony or hard surfaces. In the supine position, a medial incision was taken over the medial malleolus. Fracture was exposed well, and the interfragmentary periosteum was excised. The medial malleolus was internally fixed by a 6-hole LC-DCP (Fig. 3).
Below-knee slab applied to casualty. Local ice application, limb elevation over the BB frame, and medication are used to reduce swelling. The patient operated on day 7 after wrinkles were seen on the ankle. The ankle was approached from the posterolateral side (Fig. 2a) with the patient in a prone position for treating posterior malleolar fractures and other related fibular fractures. In this method, the muscles of the peroneus brevis and flexor halluces longus are dissected in the intermuscular plane, all the way to the tibia and fibula. To expose the syndesmosis and the posterior malleolus, the flexor halluces longus muscle belly is raised from behind the distal tibia. Anatomical reduction of the post-malleolar portion to the tibia was done. Typically, a four-hole ellis plate is used in antiglide mode to reduce posterior malleolar fragments. A window was created between the lateral skin flap and the peroneus longus and brevis tendon (Fig. 2b). Lateral malleolus fractures are exposed and reduced well by bone-holding forceps. The lateral malleolus is fixed with a 7-hole, 1/3-locking tubular plate. An external rotating stressor was applied to all syndesmoses before closure by the surgeon using a small Hohmann retractor placed in the interosseous region. Through direct observation and fluoroscopically distal tibiofibular articulation, stability was evaluated. Our criteria for determining appropriate stability was that under stress, the superior clear space deviation from the medial clear space never exceeded more than 1 mm and the tibiofibular articulation had diastasis <1 mm [9]. We observed that syndesmosis was not stable, which was not a usually happen after fixation of the posterior malleolus. The distal fragment 2nd screw was replaced by a tricortical syndesmotic screw, and stability was again confirmed under fluoroscopy. We believe that in terms of wound healing, this method is a more physiological way of dissecting, as the incision is sutured over muscle and not on bony or hard surfaces. In the supine position, a medial incision was taken over the medial malleolus. Fracture was exposed well, and the interfragmentary periosteum was excised. The medial malleolus was internally fixed by a 6-hole LC-DCP (Fig. 3).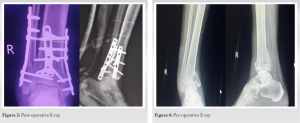
Case 2
A 49-year-old female suffered significant trauma to her right ankle from a domestic fall, resulting in a trimalleolar fracture of the distal tibia (Fig. 4). Below-knee slab was applied to the casualty. Local ice application, limb elevation over the BB frame, and medication are used to reduce swelling. The patient was operated on day 6 after wrinkles were seen on the ankle. The ankle was approached from the posterolateral side with the patient in a prone position for treating posterior malleolar fractures and other related fibular fractures. Anatomical reduction of the posterior malleolar portion to a tibia was done with a four-hole ellipse plate in antiglide mode (Fig. 5). A window was created between the lateral skin flap and the peroneus longus and brevis tendon. Lateral malleolus fracture is exposed and reduced well by bone-holding forceps. The lateral malleolus is fixed with an 8-hole, 1/3-locking tubular plate. We observed that syndesmosis was not stable, which was not a usually happen after fixation of the posterior malleolus. The distal fragment 4th screw was replaced by a tricortical syndesmotic screw, and stability was again confirmed under fluoroscopy. In the supine position, a medial incision was taken over the medial malleolus. Fracture was exposed well, and the interfragmentary periosteum was excised. The medial malleolus was internally fixed by two corticocancellous screws with an 8-hole LC-DCP. The anterior distal tibia fragment was fixed with a 16-mm anteroposterior CC screw (Fig. 6).
A window was created between the lateral skin flap and the peroneus longus and brevis tendon. Lateral malleolus fracture is exposed and reduced well by bone-holding forceps. The lateral malleolus is fixed with an 8-hole, 1/3-locking tubular plate. We observed that syndesmosis was not stable, which was not a usually happen after fixation of the posterior malleolus. The distal fragment 4th screw was replaced by a tricortical syndesmotic screw, and stability was again confirmed under fluoroscopy. In the supine position, a medial incision was taken over the medial malleolus. Fracture was exposed well, and the interfragmentary periosteum was excised. The medial malleolus was internally fixed by two corticocancellous screws with an 8-hole LC-DCP. The anterior distal tibia fragment was fixed with a 16-mm anteroposterior CC screw (Fig. 6).
Post-operative rehabilitation
Patients were told not to put any weight on their legs for 6 weeks after surgery and were required to wear a short-leg splint. Early after surgery, ROM exercises for the ankle and subtalar region were started.
Follow-up and outcome
Plain radiographs taken after surgery revealed a well-reduced fracture with the proper internal fixation. There were no orthopedic problems, such as infection, implant blackout, or worsening of the underlying illnesses, during the 12-month post-operative follow-up period. Six months following surgery, the fracture was seen to be healed. The AOFAS and Visual Analog Scale (VAS score) were 90% and 2 (mild pain) at 6 months, respectively, in both cases. The patient was able to fully bear his weight while walking and restored his pre-operative gait function.
Injury types involving supination-exorotation or pronation-exorotation are typically responsible for posterior malleolus involvement in ankle fractures. The mechanics of the event leading to the posterior malleolar fragment are PITFL rupture, which results in an avulsion fracture. Stabilization from the posterior side becomes crucial since the PITFL is primarily responsible for stabilizing ankle ring syndesmosis, and in such types of injuries, fibular fragment apex typically lies posterior or in some cases posterolateral. In the literature, various strategies and techniques for fixing the posterior malleolus have been documented. Conventionally, these fractures have been treated with anterior-to-posterior (A-to-P) screws and indirect reduction [10]. The criteria for fixing these fractures were when there was more than 25–33% involvement of the articular surface, and under this criteria, there was a suitable environment for AP screw fixation [5]. In this fracture, we are fixing a large fragment against a smaller one, so we do not recommend this method as (1) there is a possibility that appropriate reduction is not achieved sometimes and (2) it might result in a less stable construct as fracture site compression is a challenging part to achieve (3) smaller fragments of less than 15 mm are difficult to correct as smaller threads do not offer the required amount of compression, and in the case of a cancellous screw that is partially threaded, every thread will not reach the fracture site. (4) This traditional method cannot be used for fractures involving multiple fragments or comminuted fractures. This strategy has lost favor with the majority of surgeons as the indications for surgery have expanded over time. 29 ankle fractures were treated by Park et al. with a posterior malleolar fragment. In 15 cases, syndesmotic screws were employed for fixation, while in 14 cases, posterior malleolar fixation was used. The degree of ankle arthrosis, clinical scores, and reduction quality were not statistically different between groups [11]. 15 posterior malleolus fracture cases were treated by Chung et al., and 5 of the cases had excellent outcomes and 7 had good outcomes [12]. The hypothesis of Miller et al. [13] stated that there is a high probability of restoration of the stability of syndesmosis by fixing posterior malleolar fractures as compared to trans-syndesmotic fixation alone. According to a number of studies [14], syndesmotic injury is the primary factor influencing functional results. The necessity for independent trans-syndesmotic fixation may decrease as a result of PM fixation’s increased stability of syndesmotic complexes. Trans-syndesmotic fixation may be anatomically and biomechanically inferior as anatomical restoration of the syndesmosis is possible with the reduction and fixation of PM fragments. Behery et al. [15] reported why there was no residual instability under stress in 95% of cases where posterior malleolar fixation was carried out. In 2 out of 43 cases, he found out that syndesmosis was unstable despite PM fixation and that it required separate trans-syndesmotic screws; the reason is unknown. One theory is that the PITFL may have undergone severe iatrogenic stripping during fragment identification, causing the PITFL function to no longer be restored by reinstalling the PM fragment. Syndesmotic articulation was better. With PM fixation as compared to direct trans-syndesmotic screw fixation, this was the conclusion derived from a study in which post-operative CT scans of ankles in which PM fixation was done without considering the fragment size were compared with CT scans with only syndesmotic screws [16]. Furthermore, a cadaver investigation statistics show that stiffness of syndesmosis was restored in 70% of cases with posterior malleolar fixation as compared to only 40% with syndesmotic screws alone. This is in line with earlier data showing that when compared to the other syndesmotic ligaments, instability of the syndesmosis can be best predicted with a PITFL injury [17]. In addition, in contrast to a straight lateral fibular incision, PM fixation through an open, posterolateral technique was not linked to an elevated risk of wound complications. Our findings on the quality of fracture reduction, arthrosis formation, and wound healing are in line with those of prior research on the posterolateral approach. The worst results were obtained both radiologically and functionally when syndesmosis repair was not carried out and posterior malleolus fixation was not done.
For a satisfactory clinical and functional outcome of a trimalleolar fracture, a substantial amount of pre-operative imaging, a clear and complete idea of the anatomy and biomechanics of the fracture, a reasonable exposure for visualization, and a stable fixation of all three components are necessary. In a trimalleolar ankle fracture, fixation of the posterior malleolus is important for a better post-operative functional outcome, irrespective of the size of the posterior malleolus. If syndesmosis is not stable after fixation of the posterior malleolus, the author suggests syndesmosis CC screw fixation through the lateral fibula plate.
Lateral fibula plate fixation through a window between the skin and the peroneus longus and brevis tendon has an advantage as we can fix syndesmosis by the same approach through the same fibular plate by a corticocancellous screw.
References
- 1.Koval KJ, Lurie J, Zhou W, Sparks MB, Cantu RV, Sporer SM, et al. Ankle fractures in the elderly: What you get depends on where you live and who you see. J Orthop Trauma 2005;19:635-9. [Google Scholar]
- 2.Jaskulka RA, Ittner G, Schedl R. Fractures of the posterior tibial margin: Their role in the prognosis of malleolar fractures. J Trauma 1989;29:1565-70. [Google Scholar]
- 3.Bois AJ, Dust W. Posterior fracture dislocation of the ankle: Technique and clinical experience using a posteromedial surgical approach. J Orthop Trauma 2008;22:629-36. [Google Scholar]
- 4.Marsh JL, Saltzman CL. Ankle fractures. In: Bucholz RW, Heckman JD, Court-Brown CM, editors. Rockwood and Green’s Fractures in Adults. 6th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2005. p. 2147-235. [Google Scholar]
- 5.Nelson MC, Jensen NK. The treatment of trimalleolar fractures of the ankle. Surg Gynecol Obstet 1940;71:509-14. [Google Scholar]
- 6.Gardner MJ, Brodsky A, Briggs SM, Nielson JH, Lorich DG. Fixation of posterior malleolar fractures provides greater syndesmotic stability. Clin Orthop Relat Res 2006;447:165-71. [Google Scholar]
- 7.Verhage SM, Boot F, Schipper IB, Hoogendoorn JM. Open reduction and internal fixation of posterior malleolar fractures using the posterolateral approach. Bone Joint J 2016;98-B:812-7. [Google Scholar]
- 8.Talbot M, Steenblock TR, Cole PA. Posterolateral approach for open reduction and internal fixation of trimalleolar ankle fractures. Can J Surg 2005;48:487-90. [Google Scholar]
- 9.Beumer A, van Hemert WL, Niesing R, Entius CA, Ginai AZ, Mulder PG, et al. Radiographic measurement of the distal tibiofibular syndesmosis has limited use. Clin Orthop Relat Res 2004;423:227-34. [Google Scholar]
- 10.Bartoníček J, Rammelt S, Tuček M. Posterior malleolar fractures: Changing concepts and recent developments. Foot Ankle Clin 2017;22:125-45. [Google Scholar]
- 11.Park SJ, Jeong HJ, Shin HK, Seo DS, Choi YM, Kim E Results of syndesmotic screw fixation versus posterior malleolus fixation in syndesmotic injury at pronation external rotation stage IV ankle fracture with posterior malleolus fracture: Postoperative one year follow up. J Korean Foot Ankle Soc 2014;18:29-35. [Google Scholar]
- 12.Chung HW, Kim DH, Yoo SH, Suh JS. Treatment of the posterior malleolar fracture using posterior approach. J Korean Fract Soc 2010;23:50-6. [Google Scholar]
- 13.Miller AN, Carroll EA, Parker RJ, Helfet DL, Lorich DG. Posterior malleolar stabilization of syndesmotic injuries is equivalent to screw fixation. Clin Orthop Relat Res 2010;468:1129-35. [Google Scholar]
- 14.Weening B, Bhandari M. Predictors of functional outcome following transsyndesmotic screw fixation of ankle fractures. J Orthop Trauma 2005;19:102-8. [Google Scholar]
- 15.Behery OA, Narayanan R, Konda SR, Tejwani NC, Egol KA. Posterior malleolar fixation reduces the incidence of trans-syndesmotic fixation in rotational ankle fracture repair. Iowa Orthop J 2021;41:121-5. [Google Scholar]
- 16.Miller AN, Carroll EA, Parker RJ, Boraiah S, Helfet DL, Lorich DG. Direct visualization for syndesmotic stabilization of ankle fractures. Foot Ankle Int 2009;30:419-26. [Google Scholar]
- 17.Park YH, Yoon MA, Choi WS, Choi GW, Hong SJ, Kim HJ. The predictive value of MRI in the syndesmotic instability of ankle fracture. Skeletal Radiol 2017;47:533-40. [Google Scholar]










