Total knee arthroplasty in an ipsilateral below-knee amputee presents a unique challenge for orthopedic surgeons
Dr. Christopher E Marrero, Department of Orthopaedic Surgery, LSUHSC, 2021 Perdido St. 7th Floor, New Orleans, Louisiana 70112. E-mail: cmarre@lsuhsc.edu
Introduction: Total knee arthroplasty (TKA) has the highest annual incidence among all joint replacement surgeries. Below-knee amputation (BKA) is another common procedure to treat lower-limb-threatening pathologies. These two procedures are commonly performed individually, but an ipsilateral TKA performed on a BKA patient is rare. While ipsilateral amputation is not a contraindication for TKA, it presents orthopaedic surgeons with a unique case and necessitates thoughtful pre-operative planning regarding proper positioning, alignment determination, surgical technique, and rehabilitation for the best outcome.
Objectives: We present a case of a patient with a BKA who underwent ipsilateral TKA.
Case Report: This patient has a history of osteoarthritis (OA) of the right knee and diabetic neuropathy and underwent a right BKA after sustaining second-degree thermal burns to the bilateral forefeet. The patient was scheduled to undergo elective TKA prior to these injuries but was forced to postpone due to their severity. Following the BKA, the patient regained his ability to ambulate independently with prosthesis but continued to suffer from OA symptoms. The patient was then scheduled for surgery, and a TKA was performed.
conclusion: The patient underwent a TKA and tolerated the surgery well without complications. Appropriate positioning was achieved using a popliteal post. Alignment and tibial cut were checked using fluoroscopy. All components were cemented into position, and the patella was resurfaced. The patient did well postoperatively and was using his prosthesis and ambulating independently at the final follow-up.
Keywords: Below-knee amputation, total knee arthroplasty, osteoarthritis.
Osteoarthritis (OA) is the most common joint pathology worldwide, symptomatically affecting roughly 240 million individuals 60 years of age or older [1]. While OA can affect any joint, knee OA is the most common [2]. Non-surgical methods to manage knee OA include weight loss, activity modification, bracing, non-steroidal anti-inflammatory medications, viscosupplementation, corticosteroid injections, and other non-steroidal injections. If these conservative methods are unsuccessful, patients with end-stage knee OA are often treated via total knee arthroplasty (TKA). TKA and total hip arthroplasty are the most common joint replacement surgeries [3]. Currently, more than 670,000 TKA procedures are performed annually in the United States [4]. Lower-extremity amputation has an annual incidence of roughly 150,000 in the United States [5]. Below-knee amputation (BKA) is a common procedure for limb-threatening pathology in the lower extremity. Acute, urgent indications for BKA include necrotizing fasciitis and vascular injuries, while less acute indications include severe peripheral vascular disease, chronic non-healing ulcers, and persistent infections with a risk of sepsis [6]. These two procedures are commonly performed individually, but an ipsilateral TKA performed on a BKA patient is a rare occurrence. While ipsilateral amputation is not a contraindication for TKA, it presents orthopedic surgeons with a unique challenge. Focus on pre-operative planning, proper positioning, alignment techniques, and rehabilitation are crucial to obtaining the best outcome [7]. This case report presents a below-knee amputee who underwent an ipsilateral TKA.
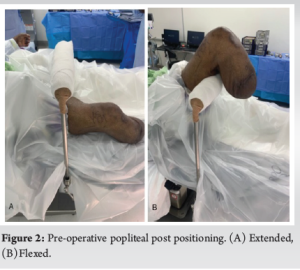
Informed consent was obtained before surgery from the patient to use case history, demographics, and photographs for publication of the case report. The patient is a 68-year-old male with a history of diabetic neuropathy and a BMI of 30.7 kg/m2 who presented complaining of worsening right knee pain for several years. The right knee had a mild varus deformity, a range of motion of 0° to 120°, and no instability. X-rays revealed moderate tricompartmental degenerative changes. After failing all non-operative treatments, he was scheduled for the right TKA. While awaiting his surgery, he sustained second-degree burns to both feet from a hot shower. The patient initially presented to a hospital emergency department after noticing fluid draining from his lower extremities, and this injury resulted in a right BKA and left transmetatarsal amputation. After the patient’s amputations, he regained his ability to ambulate using right below-knee prosthesis. The patient continued to suffer from right knee OA with pain, especially when weight-bearing. At 4 months post-operative, the patient’s right BKA and left transmetatarsal stumps were well healed. The right knee range of motion was 0° to 110°. The patient was again offered surgery and elected to undergo a right TKA. Standard pre-operative planning with templates was performed for an Ortho Development cruciate-retaining knee. On the day of surgery, informed consent was obtained, and the patient was taken to the operating room and placed on the operating table in the supine position. He underwent general anesthesia, and the right lower extremity was prepped and draped in the usual sterile fashion. A popliteal post was placed in the surgical field to achieve appropriate positioning during flexion. A timeout was done, a tourniquet was inflated, and a standard anteromedial approach was performed. The patella was flipped, and the knee was placed over the popliteal post to prepare the femur (Fig. 1 and 2).
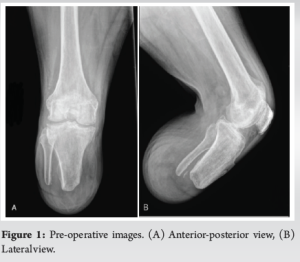
The femoral preparation was performed in a routine fashion with no special considerations. The bone quality was found to be normal. Next, the proximal tibia was prepared. An assistant’s hand was placed on the tibial crest to aid in anterior subluxation and adequate exposure of the proximal tibia (Fig. 3).
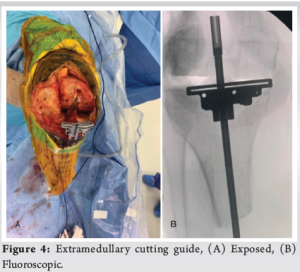
An extramedullary cutting guide was placed on the proximal tibia, and while holding the distal portion of the guide by hand, a stylus was used to position the cutting block for pinning in a position to remove 2 mm from the medial tibial plateau (Fig. 4a and b).
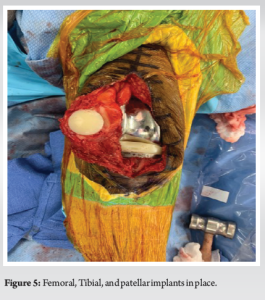
The alignment was estimated using the residual tibial crest and fluoroscopy. The tibial cut was made, and alignment was confirmed using fluoroscopy. Gap balancing and the rest of the tibial preparation, as well as the patella cut, were performed in a routine fashion. A trial reduction was performed and the knee was found to be stable throughout full range of motion. All components were cemented into position (Fig. 5).
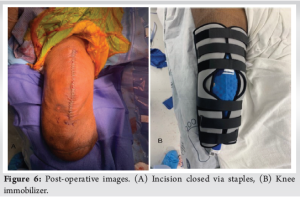
The medial parapatellar incision was closed using a running 1-0 ethibond suture. The subcutaneous tissue was closed using a 3-0 Vicryl interrupted suture. The skin was closed using staples (Fig. 6a). An occlusive dressing was applied as well as a knee immobilizer to be used while supine (Fig. 6b).
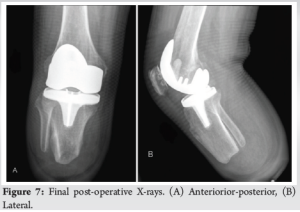
The patient was allowed to use his prosthesis and ambulate postoperatively with physical therapy. The patient did well postoperatively with no complications (Fig. 7a and b).
The patient’s post-operative course was uncomplicated; he progressed in physical therapy and was eventually able to ambulate independently with his prosthesis. At 6 months post-operative, the patient’s incision was doing well, the range of motion was 5° to 100° of flexion, and the patient was using his prosthesis without difficulty.
This patient’s BKA was a result of thermal burns to the bilateral forefeet complicated by diabetic neuropathy. Due to his history of diabetes, this patient had an increased risk for a lower extremity amputation [8]. The patient elected to undergo TKA due to a history of OA and the failure of conservative treatment options. The patient ultimately wished to remain physically active and preserve his lower extremity function as much as possible. The patient’s knee was preserved, making BKA the most appropriate definitive treatment in comparison to through-knee or above-knee amputation. Maximum functional recovery is achieved in BKA at higher rates than in through-knee or above-knee amputations [9]. Knee arthrodesis is another alternative definitive treatment to be considered but has been shown to result in significant changes in normal gait kinematics with no increase in knee flexion [10]. TKA is the most common definitive treatment for end-stage OA when conservative treatments such as NSAIDs, physical therapy, and injections provide little-to-no relief [5, 11]. Successful TKA is dependent on optimal alignment, which is a continuing controversy over a truly superior method [12]. Proper alignment, in this case, was achieved and checked via fluoroscopy, while other methods include the assistance of a robotic arm or computer navigation. Robotic-arm-assisted TKA (RATKA) has been shown to improve the accuracy of component positioning and patient-recorded outcomes; however, there is no proven difference in infection, wound dehiscence, arthrofibrosis, or overall complications between RATKA and manual TKA (mTKA) [13]. Computer navigation and custom implant guides have some evidence of improving cost-effectiveness but are not associated with any difference in patient-recorded satisfaction in comparison to mTKA [14]. In addition, navigation use for TKA improves accuracy but has resulted in higher failure rates in TKA patients with tibial malalignment [15]. In TKA, the use of cement and the decision to resurface the patella may vary depending on the comorbidities of the patient or the preference of the surgeon, both of which were performed in this case. Aseptic loosening, along with periprosthetic joint infection and periprosthetic fracture, are among the most common complications in TKA patients, often leading to a need for revision [16]. Patellar resurfacing has been shown to reduce post-operative reoperation incidence and noise and also increase knee score society and function score [17]. Rehabilitation is a key aspect of quality of life and functionality following TKA and BKA, but it is especially important for patients who undergo both procedures ipsilaterally. BKA is preferred over above-knee amputation due to its association with improved functional outcomes [7]. The use of an anti-gravity treadmill is one specific rehabilitation modality that has been found to be useful in achieving maximum prosthetic functionality after BKA [18]. Achieving maximum functionality in BKA patients requires a multidisciplinary team of physicians, nurses, therapists, and mental health professionals to assess and treat the holistic needs of each individual patient [19]. The rehabilitation team for TKA patients is similar, consisting of a multidisciplinary group of an orthopaedic surgeon, a physical therapist, a nurse, and a consumer [20]. Literature states that accelerated rehabilitation and painless recovery can be achieved through multimodal pain control with periarticular injections, along with effective patient education and a multidisciplinary team [21]. In this case, additional modifications included the use of a popliteal post for appropriate positioning and hand placement on the tibial crest during the tibial preparation. Fluoroscopy was used to ensure proper alignment of the tibial cutting jig and was also used to ensure the tibial cut was accurate. A successful result in a TKA in a below-knee amputee has previously been achieved using navigation assistance [22]. Similar to other cases, special consideration was given towards positioning techniques, alignment of implants, and the rehabilitation plan to maximize exposure, ensure stability, and achieve a successful outcome to satisfy the patient [7, 22–24]. In patients who undergo TKA after ipsilateral BKA, the timeline between the operation and weight-bearing varies case by case [7, 22–24]. This patient was allowed to immediately weight-bear using his BKA prosthesis. At the 6-month post-operative clinic visit, the patient showed no signs of effusion or instability and was ambulating using his prosthesis without difficulty with a range of motion of 5–100° of flexion. The patient was still undergoing physical therapy to try to increase his range of motion. A significant post-operative challenge for this patient was the prevention of a knee flexion contracture. Flexion contracture, a condition that reduces the range of motion, is a complication observed postoperatively in both BKA and TKA patients [25, 26]. In BKA patients, flexion contracture specifically affects successful prosthesis use and may hinder normal gait mechanics due to alignment distortion [25]. Literature shows that in TKA, older patients and men had higher incidences of flexion contracture [26]. Physical therapy in conjunction with stretching and dynamic splinting can result in an increase in the active range of motion [27]. During the rehabilitation of this patient, aggressive physical therapy was conducted. However, a 5° flexion contracture persisted at 6 months.
TKA after BKA is a rare combination in an ipsilateral lower extremity. These patients pose significant challenges to orthopaedic surgeons and other members of the multidisciplinary team providing care. However, with adequate education, careful planning, effective communication, and aggressive rehabilitation, a successful result can be obtained.
This case describes a below-knee amputee with a history of diabetic neuropathy and OA who underwent TKA after BKA. Patients who undergo TKA after BKA comprise a rare percentage of orthopaedic patients and pose significant challenges. However, with careful planning, a successful result can be obtained.
References
- 1.Allen KD, Thoma LM, Golightly YM. Epidemiology of osteoarthritis. Osteoarthritis Cartilage 2022;30:184-95. [Google Scholar]
- 2.Michael JW, Schlüter-Brust KU, Eysel P. The epidemiology, etiology, diagnosis, and treatment of osteoarthritis of the knee. Dtsch Arztebl Int 2010;107:152-62. Erratum in: Dtsch Arztebl Int 2010;107:294. [Google Scholar]
- 3.Canovas F, Dagneaux L. Quality of life after total knee arthroplasty. Orthop Traumatol Surg Res 2018;104:S41-6. [Google Scholar]
- 4.Bager CL, Karsdal M, Bihlet A, Thudium C, Byrjalsen I, Bay-Jensen AC. Incidence of total hip and total knee replacements from the prospective epidemiologic risk factor study: Considerations for event driven clinical trial design. BMC Musculoskelet Disord 2019;20:303. [Google Scholar]
- 5.Molina CS, Faulk J. Lower extremity amputation. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. [Google Scholar]
- 6.Adams CT, Lakra A. Below-knee amputation. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. [Google Scholar]
- 7.Dong K, Cohen-Rosenblum A, Hartzler M. Total knee arthroplasty after ipsilateral below-knee amputation: A review of the literature and surgical techniques. Arthroplast Today 2022;16:158-63. [Google Scholar]
- 8.Song K, Chambers AR. Diabetic foot care. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. [Google Scholar]
- 9.Crane H, Boam G, Carradice D, Vanicek N, Twiddy M, Smith GE. Through-knee versus above-knee amputation for vascular and non-vascular major lower limb amputations. Cochrane Database Syst Rev 2021;12:CD013839. [Google Scholar]
- 10.Hutchison RE, Lucas EM, Marro J, Gambon T, Bruneau KN, DesJardins JD. The effects of simulated knee arthrodesis on gait kinematics and kinetics. Proc Inst Mech Eng H 2019;233:723-34. [Google Scholar]
- 11.Kan HS, Chan PK, Chiu KY, Yan CH, Yeung SS, Ng YL, et al. Non-surgical treatment of knee osteoarthritis. Hong Kong Med J 2019;25:127-33. [Google Scholar]
- 12.Aflatooni JO, Wininger AE, Park KJ, Incavo SJ. Alignment options and robotics in total knee arthroplasty. Front Surg 2023;10:1106608. [Google Scholar]
- 13.Zhang J, Ndou WS, Ng N, Gaston P, Simpson PM, Macpherson GJ, et al. Robotic-arm assisted total knee arthroplasty is associated with improved accuracy and patient reported outcomes: A systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 2022;30:2677-95. Erratum in: Knee Surg Sports Traumatol Arthrosc 2021. [Google Scholar]
- 14.Beal MD, Delagramaticas D, Fitz D. Improving outcomes in total knee arthroplasty-do navigation or customized implants have a role? J Orthop Surg Res 2016;11:60. Erratum in: J Orthop Surg Res 2016;11:114. [Google Scholar]
- 15.Mayman D. Handheld navigation in total knee arthroplasty. Orthop Clin North Am 2014;45:185-90. [Google Scholar]
- 16.Postler A, Lützner C, Beyer F, Tille E, Lützner J. Analysis of total knee arthroplasty revision causes. BMC Musculoskelet Disord 2018;19:55. [Google Scholar]
- 17.Chen K, Dai X, Li L, Chen Z, Cui H, Lv S. Patellar resurfacing versus nonresurfacing in total knee arthroplasty: An updated meta-analysis of randomized controlled trials. J Orthop Surg Res 2021;16:83. [Google Scholar]
- 18.Mikami Y, Fukuhara K, Kawae T, Kimura H, Ochi M. The effect of anti-gravity treadmill training for prosthetic rehabilitation of a case with below-knee amputation. Prosthet Orthot Int 2015;39:502-6. [Google Scholar]
- 19.Meier RH 3rd, Melton D. Ideal functional outcomes for amputation levels. Phys Med Rehabil Clin N Am 2014;25:199-212. [Google Scholar]
- 20.Jette DU, Hunter SJ, Burkett L, Langham B, Logerstedt DS, Piuzzi NS, et al. Physical therapist management of total knee arthroplasty. Phys Ther 2020;100:1603-31. [Google Scholar]
- 21.Ranawat AS, Ranawat CS. Pain management and accelerated rehabilitation for total hip and total knee arthroplasty. J Arthroplasty 2007;22:12-5. [Google Scholar]
- 22.Putnis SE, Neri T, Coolican MR. Total knee arthroplasty in a transtibial amputee. J Orthop Case Rep 2020;10:15-8. [Google Scholar]
- 23.Konstantakos EK, Finnan RP, Krishnamurthy AB. Eight-year follow-up of total knee arthroplasty in a patient with an ipsilateral below-knee amputation. Am J Orthop (Belle Mead NJ) 2008;37:528-30. [Google Scholar]
- 24.Amanatullah DF, Trousdale RT, Sierra RJ. Total knee arthroplasty after lower extremity amputation: A review of 13 cases. J Arthroplasty 2014;29:1590-3. [Google Scholar]
- 25.Ghazali MF, Abd Razak NA, Abu Osman NA, Gholizadeh H. Awareness, potential factors, and post-amputation care of stump flexion contractures among transtibial amputees. Turk J Phys Med Rehabil 2018;64:268-76. [Google Scholar]
- 26.Goudie ST, Deakin AH, Ahmad A, Maheshwari R, Picard F. Flexion contracture following primary total knee arthroplasty: Risk factors and outcomes. Orthopedics 2011;34:e855-9. [Google Scholar]
- 27.Finger E, Willis FB. Dynamic splinting for knee flexion contracture following total knee arthroplasty: A case report. Cases J 2008;1:421. [Google Scholar]