The article emphasizes prompt diagnosis and effective surgical intervention for Pellegrini–Stieda syndrome, particularly with a massive lesion, showcasing its success in improving pain relief, range of motion, and overall quality of life, especially in cases with massive lesions.
Dr. Deepanjan Das, Department of Orthopaedics, All India Institute of Medical Sciences, Nagpur, Maharashtra, India. E-mail: somdeepd@gmail.com
Introduction: Pellegrini–Stieda syndrome, characterized by medial collateral ligament (MCL) calcification or ossification, often follows a history of trauma. While rare, its distinct radiographic features pose diagnostic challenges. Conservative treatments are effective for many, but surgical intervention is necessary when they fail.
Case Report: A 31-year-old male with knee pain and stiffness, an inability to extend his knee, and a fixed flexion deformity. Radiological examinations confirmed heterotopic ossification along the MCL, indicating post-traumatic Pellegrini–Stieda syndrome. Despite 3 months of conservative treatment, the patient’s pain persisted, leading to surgical excision. The surgical approach involved diagnostic arthroscopy, revealing arthritic changes and adhesions. Arthroscopic adhesiolysis and open excision of the ossified mass significantly improved the patient’s range of motion. Histopathological examination confirmed heterotopic bone formation. Follow-up appointments at 1, 3, and 6 months showed a pain-free and mobile knee joint, with the Pellegrini–Stieda lesion disappearing from radiographs.
Conclusion: This case underscores the effectiveness of surgical intervention for refractory Pellegrini–Stieda syndrome, offering hope for improved patient outcomes and highlighting the importance of early diagnosis and tailored treatment in managing this rare condition.
Keywords: Pellegrini–stieda syndrome, massive lesion, heterotopic ossification, arthroscopic adhesiolysis, medial collateral ligament.
Pellegrini–Stieda syndrome, initially reported by Pellegrini [1] and Stieda [2], is rare but painful, resulting from medial collateral ligament (MCL) calcification due to trauma, causing knee pain and restricted movement. Despite its rarity, distinctive radiographic features enable diagnosis. When conservative treatments fail, surgery is essential. This article presents a successful case treated with arthroscopic adhesiolysis and en bloc excision of the calcified MCL mass, leading to a favorable outcome without recurrence during follow-up.
A 31-year-old male presented with persistent right knee pain and stiffness for a year following a road traffic accident that led to intramedullary nailing of his right femur and tibia. Despite initiating physiotherapy and transitioning to full weight-bearing, he developed knee pain accompanied by a significant inability to fully extend the right knee. Physical examination showed tenderness around the medial aspect of the right knee but no instability or effusion or local warmth. A fixed flexion deformity of 30° was observed, with active and passive range of motion limited to 30–80° of flexion due to pain. The surgical incision from the prior operation appeared healthy. A palpable, fixed bony prominence was identified over the right medial femoral condyle, and no neurological deficits were detected. Plain X-ray imaging unveiled a curvilinear opacity within the soft tissue, originating from the medial femoral condyle and extending distally (Fig. 1).

Magnetic resonance imaging (MRI) revealed a curvilinear calcification with small osteophytes along the posteromedial aspect of the femoral condyle. This calcification extended along the path of the MCL, indicative of a calcified hematoma, suggesting a probable diagnosis of post-traumatic Pellegrini–Stieda syndrome (Fig. 2). 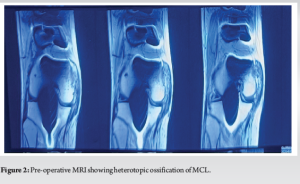
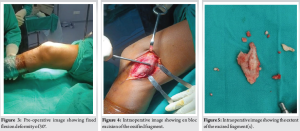
Initial conservative treatment, including oral analgesics, physiotherapy, and corticosteroid injections, was provided temporary relief, leading to surgical intervention. On the table, examination revealed a fixed flexion deformity of 30° that did not correct even after giving spinal anesthesia and adequate muscle relaxant (Fig. 3). Diagnostic arthroscopy exposed early arthritic changes and joint adhesions, which were addressed through arthroscopic adhesiolysis. Subsequently, a 10 cm incision was made along the medial knee, extending from the medial femoral condyle to the medial tibial condyle, exposing the ossified mass (Fig. 4). The pinkish, bony hard, rough mass measuring approximately 7.5 cm × 4.5cm × 1 cm was en bloc resected (Fig. 5) using osteotome and mallet, significantly improving the patient’s range of motion (Fig. 6). Intraoperatively, clinical assessments for laxity were performed. There was no significant valgus laxity noted at the knee. It was decided to forgo the reconstruction of the MCL.
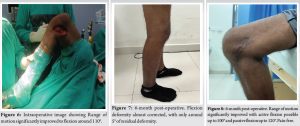
Histopathological examination revealed abundant peripheral fibro collagenous tissue with the central area showing many trabeculae composed of laminar bone. Intertrabecular area showing adipose tissue. Surrounding the bony tissue, mature cartilage was seen. Features confirmed heterotopic bone formation. Post-surgery, the patient began a range of motion exercises and full weight-bearing mobilization. Follow-up assessments at 2 weeks and 1-, 3-, and 6-month post-surgery revealed no pain, substantial range of motion improvement, and only 5° of fixed flexion deformity (Fig. 7). Active flexion reached 100°, passive flexion was 120° without pain (Fig. 8), and radiographs showed no Pellegrini–Stieda lesion (Fig. 9).

Pellegrini–Stieda syndrome is a rare knee condition characterized by calcification or ossification of the MCL, typically occurring at its proximal attachment [3]. The exact location of the Pellegrini–Stieda lesion remains debated, with possibilities including the MCL origin, medial to the gastrocnemius medial head muscle origin, and involvement of the adductor magnus tendon and posterior attachment of the medial patellofemoral ligament [1, 2, 4, 5, 6]. Mendes et al. described four types of ossification: I: Beak shaped with inferior orientation and union to the femur, II: Drop shaped with inferior orientation and parallel to the femur, III: Elongated with superior orientation, and IV: With superior orientation and inferior attached to the femur [4]. This condition typically affects individuals aged 25–40, with a higher incidence in males [7]. This condition typically stems from direct or indirect trauma, including post-surgical rehabilitation or therapeutic knee joint manipulation [8], leading to hydroxyapatite deposition occurring within the injured tissue. There is a likely calcification of a post-traumatic hematoma. Other factors have also been suggested, including metaplasia of the ligamentous tissue, periosteal proliferation, and a type of myositis ossificans [9]. Most patients are asymptomatic [10]. Others may present with symptoms such as pain and tenderness on the medial aspect of the knee, flexion deformity, and restricted range of motion [7]. Plain X-rays reveal typical ossification along the MCL [11]. T2-weighted MRI provides precise information about the osseous fragment’s extent relative to the ligament, whereas T1-weighted imaging indicates matured fragments with high signal fatty marrow [12]. Conservative treatment for mild-to-moderate cases includes local corticosteroid injections and range of motion exercises [11]. However, when conservative approaches fail, surgical intervention is recommended. Surgical removal of the ossified fragment, along with MCL repair, is the preferred method [13]. An emerging alternative involves ultrasound-guided percutaneous calcific lavage, followed by autologous platelet-rich plasma infiltration [14]. What made our case unique was the unusually large size of the ossified mass. Such a size is seldom documented in existing medical literature. The unusually large ossified mass necessitated surgical removal. Post-surgery, the patient experienced improved range of motion, complete pain relief, and reduced deformities, demonstrating the effectiveness of surgical intervention. Another noteworthy observation about our case was that despite the excision of such a large mass, there was no significant valgus laxity noted at the knee, leading to the decision to forgo the reconstruction of the MCL. The timing of the surgery, after over a year since the onset, was appropriate, considering that the procedure’s success depends on the maturity of the heterotopic ossification. Immature and younger lesions have a higher recurrence rate [5]. Arthroscopic adhesiolysis addressed intra-articular adhesions resulting from the traumatic injury, contributing to the positive outcome. This case highlights that surgical intervention can effectively manage refractory Pellegrini-Stieda syndrome, offering enhanced quality of life for affected individuals.
Pellegrini–Stieda syndrome may be rare, but its impact on individuals with knee issues cannot be underestimated. With its distinctive radiographic, MRI, and histopathological features, early diagnosis is crucial. While conservative management is effective for many, our case report sheds light on a successful surgical approach for refractory cases-arthroscopic adhesiolysis followed by open excision of the ossified mass. This procedure offers a ray of hope for those suffering from this condition, providing a path toward a satisfactory outcome and improved quality of life. As we add our findings to the limited literature available, we underscore the importance of continued research and knowledge sharing in the pursuit of better management strategies for Pellegrini–Stieda syndrome.
This article highlights the successful surgical management of Pellegrini–Stieda syndrome with a massive lesion in a 31-year-old male patient suffering from persistent knee pain and stiffness. The surgical procedure not only removed the troublesome mass but also significantly improved the patient’s range of motion and quality of life. The article underscores the effectiveness of surgical intervention in refractory Pellegrini–Stieda syndrome, offering hope for improved outcomes and quality of life for affected individuals.
References
- 1.Pellegrini: Ossificazione Traumatica Del Ligamento. Available from: [Last accessed on 2023 Sep 19]. [Google Scholar]
- 2.Stieda: Uber Eine Typische Verletzung am Unteren Femurende. Available from: [Last accessed on 2023 Sep 19]. [Google Scholar]
- 3.Somford MP, Janssen RP, Meijer D, Roeling TA, Brown C Jr., Eygendaal D. The Pellegrini-Stieda lesion of the knee: An anatomical and radiological review. J Knee Surg 2019;32:637-41. [Google Scholar]
- 4.Mendes LF, Pretterklieber ML, Cho JH, Garcia GM, Resnick DL, Chung CB. Pellegrini-Stieda disease: A heterogeneous disorder not synonymous with ossification/calcification of the tibial collateral ligament-anatomic and imaging investigation. Skeletal Radiol 2006;35:916-22. [Google Scholar]
- 5.Theivendran K, Lever CJ, Hart WJ. Good result after surgical treatment of Pellegrini-Stieda syndrome. Knee Surg Sports Traumatol Arthrosc 2009;17:1231-3. [Google Scholar]
- 6.McArthur TA, Pitt MJ, Garth WP Jr., Narducci CA Jr. Pellegrini-Stieda ossification can also involve the posterior attachment of the MPFL. Clin Imaging 2016;40:1014-7. [Google Scholar]
- 7.Scheib JS, Quinet RJ. Pellegrini-Stieda syndrome mimicking acute septic arthritis. South Med J 1989;82:90-1. [Google Scholar]
- 8.Yildiz N, Ardic F, Sabir N, Ercidogan O. Pellegrini-Stieda disease in traumatic brain injury rehabilitation. Am J Phys Med Rehabil 2008;87:514. [Google Scholar]
- 9.Majjhoo A, Sagar H. Pellegrini-Stieda disease: Calcification of the medial collateral ligament. J Clin Rheumatol 2011;17:456. [Google Scholar]
- 10.Ploumis A, Petropoulos O, Balta AΑ, Manolis I, Vasileiadis GΙ, Varvarousis DΝ. Pellegrini-Stieda disease in a severely injured patient with spinal cord injury. J Musculoskelet Neuronal Interact 2023;23:365-7. [Google Scholar]
- 11.Altschuler EL, Bryce TN. Images in clinical medicine. Pellegrini-Stieda syndrome. N Engl J Med 2006;354:e1. [Google Scholar]
- 12.Niitsu M, Ikeda K, Iijima T, Ochiai N, Noguchi M, Itai Y. MR imaging of Pellegrini-Stieda disease. Radiat Med 1999;17:405-9. [Google Scholar]
- 13.Wang JC, Shapiro MS. Pellegrini-Stieda syndrome. Am J Orthop (Belle Mead NJ) 1995;24:493-7. [Google Scholar]
- 14.Rizky DA, Lee K, Sulaeman WS, Butarbutar JC, Suginawan ET. Ultrasound-guided percutaneous lavage as treatment for Pellegrini-Stieda syndrome with suspected same patho-mechanism as rotator cuff syndrome: A case report. J Orthop Case Rep 2023;13:27-32. [Google Scholar]











