The rarity of surgical intervention in cases of degenerative atlantoaxial osteoarthritis highlights the importance of conservative management as the mainstay of treatment. Surgical intervention, although effective with a low rate of serious complications, should be considered only in cases where conservative approaches fail, and symptoms become incapacitating.
Dr. Bharat Dave, Department of Spine Surgery, Stavya Spine Hospital and Research Institute, Ahmedabad, Gujarat, India. E-mail: brd_172@yahoo.com
Introduction: Osteoarthritis of the atlantoaxial joint is a significant cause of occipitocervical pain, which is often missed and has an increasing prevalence with age. The patients typically present with occipitocervical pain and restricted and painful neck rotations. Despite the primary reliance on conservative management for this pathology, surgical intervention becomes crucial for those not responding to standard conservative treatment. The presented case series highlights the rarity of the requirement of surgical intervention in the management of Atlantoaxial osteoarthritis (AAOA) and the clinical outcomes of surgical management in AAOA.
Case Report: This paper presents a case series of four patients who were managed surgically with atlantoaxial fusion, from a database of 108 patients with AAOA. The case series includes three males and one female with a mean age of presentation being 67.5 years. All four patients presented with occipitocervical pain, and painful neck movements and were diagnosed with AAOA on the anteroposterior open mouth view radiographs showing changes of osteoarthritis such as bone erosions, sclerosis, osteophytes. The patients were managed conservatively with non-steroidal anti-inflammatory drugs, intra-articular steroid injections, and cervical collar immobilization. Those not responding to conservative management and with incapacitating pain were managed surgically with atlantoaxial fusion procedures.
Conclusion: In a group of patients with a painful and debilitating degenerative AAOA only a small proportion of cases require surgical intervention. In this cohort, only 3.70 % of patients required surgery, highlighting the rarity of surgical intervention required in the management of AAOA. Nevertheless, when conducted, atlantoaxial fusion has proved to be efficacious with a low rate of serious complications and the patient self-rated outcome in terms of post-operative visual analog scale score and neck disability index scores indicating a high degree of satisfaction with the procedures.
Keywords: Atlantoaxial, osteoarthritis, fusion, transarticular screws.
Osteoarthritis of the atlantoaxial joint has been recognized as a distinct cause of occipitocervical pain with a prevalence of 5.4% in the sixth decade to 18.2% in the ninth decade of life [1]. The patient presents with occipital or parietal headache, sometimes radiating toward the frontal bone into the eye. Patients occasionally also complain of visual problems and painful crepitation with head rotation and the patient having to support the head with his hands while rotating. Dreyfuss et al. showed that an experimental increase in pressure in the atlantoaxial joints by injections caused similar patterns of pain as seen in atlantoaxial osteoarthritis (AAOA), and thereby confirming the role of the atlantoaxial joint as a pain generator [2]. Conservative management is the mainstay of treatment which includes NSAIDs, soft cervical collar, and intra-articular injections. Patients not responding to conservative management and with incapacitating pain are managed surgically. Whitesides and McDonalds were the first to report successful surgical treatment with arthrodesis for degenerative AAOA [3]. Internal fixation of atlantoaxial segment is surgically challenging as the structures are small and the anatomic area is not very accessible. AAOA is mainly managed conservatively and surgical intervention is required in a very small proportion of cases. In this case series, we have described four cases from our database of 108 patients of AAOA, which were managed surgically, with different techniques for achieving atlantoaxial fusion. The objective of this case series is to describe the rarity of surgical intervention in cases of AAOA and the clinical improvement post-surgery.
This is a single-center retrospective study conducted on the Indian population. We conducted this study in compliance with the principles of the Declaration of Helsinki. Ethics committee approval was obtained from the Institutional Ethics Committee and registered with the Clinical Trial Registry India (CTRI/2021/04/032985). The study included patients presenting to our Institute from January 2006 to January 2021 with cervico-occipital pain and radiologically proven AAOA, who had failed conservative management and were managed surgically. Patients with complete 2-year follow-up were included in the study. Patients with traumatic or infective affection of the atlantoaxial joint, spondyloarthropathy including rheumatoid arthritis affection of the atlantoaxial joint, and patients with occipitalized C1 were excluded from the study. From a total of 108 patients from our database, four patients who fulfilled the inclusion criteria were included in the study. The demographic data of the patient and pre-treatment visual analogue scale (VAS) score and neck disability index (NDI) were recorded. Cervical spine anteroposterior open mouth view and lateral flexion and extension view radiographs were done. The diagnosis was confirmed by an open-mouth radiograph typically showing a reduction in atlantoaxial facet joint space and other changes of osteoarthritis such as erosions, subchondral sclerosis, and osteophytes. Cervical spine lateral, flexion-extension view radiographs were done to look for altantoaxial instability by measuring the atlantodental interval (distance between the anterior wall of the odontoid process and posterior border of the anterior arch of the atlas) using Medsynapse PACS 5.0.1.3. The patients were managed conservatively with NSAID’s, non-opioid analgesics, and soft cervical collar immobilization or intra-articular steroid injections. The patients not responding to the conservative line of management and with unbearable pain were managed surgically with atlantoaxial fusion using different modalities such as posterior atlantoaxial wiring and bone grafting, atlantoaxial transarticular screws or cervical lateral mass and pedicle screw and rod construct. The follow-up data of patients at 2 years was assessed and X-ray/CT of the cervical spine, post-operative VAS, and NDI were noted.
From our database of 108 patients, only four patients required surgical intervention which was about 3.70% of the total study population. Of the four patients, three were males and one was a female. The mean age of the patients was 67.5 years. The mean pre-operative VAS was 7.5 which improved to 2.5 postoperatively and the mean pre-operative NDI was 35.5 which improved to 12 postoperatively. There was significant improvement in the VAS and NDI scores with surgical management. None of the patients had any intra-operative or post-operative complications.
Case 1
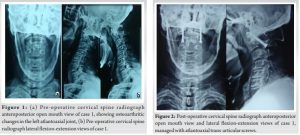
A 72-year-old male presented with complaints of left-sided neck pain and occipital pain with restricted neck rotations. Radiographs were suggestive of degenerative changes in the left atlantoaxial facet joint. Patient was managed conservatively with analgesics and a soft cervical collar. After 4 months of failed conservative trials, the patient was offered surgical management, and atlantoaxial fusion with bilateral transarticular screws and bone grafting was done. At 2-year follow-up, the patient reports a 75% improvement in neck pain. (Fig. 1a, b and 2) show the pre-operative and post-operative radiographs of this case.
Surgical procedure
Under general anesthesia, the patient is positioned prone and the neck is held in alignment by skull tongs. The posterior midline approach is taken and C1-C2 vertebrae are exposed up to the lateral margin of the C1-C2 joint complex. C1-C2 alignment checked under image intensifier and entry point for the transarticular screw made. The entry point for the transarticular screw lies in a straight sagittal line in the center of the isthmus at the inferior border of the caudal facet of C2, 2 mm cranial and lateral to the medial border and is directed toward the anterior arch of C1. The trajectory is tapped and a 3.5 mm screw is passed on both sides. Bone graft was obtained from the right posterior superior iliac spine and placed between the lamina of C1-C2 and in the C1-C2 joint space. Incision is closed in layers over a drain.
Case 2
A 72-year-old male presented with complaints of neck pain with heaviness in the occipital area for 2 months. Radiological investigations showed arthritic changes in the left atlantoaxial facet joint. The patient was managed conservatively with analgesics, a soft cervical collar, and a greater occipital nerve block but had no relief. The patient was managed surgically with posterior C1-C2 wiring and bone grafting. Postoperatively, the patient had some amount of residual neck pain, especially on neck extension movement which subsided with time at subsequent follow-ups. (Fig. 3a, b and 4) show the pre-operative and post-operative radiographs of this case.

Surgical procedure
Under general anesthesia, the patient is positioned prone and the neck is held in alignment by skull tongs. The posterior midline approach is taken and C1-C2 vertebrae are exposed up to the lateral margin of the C1-C2 joint complex. C1-C2 alignment was checked under the image intensifier and a loop of SS wire passed on either side of the posterior tubercle of C1 and the other end passed through the holes made in the base of C2 and the wire loops were tightened. Bone graft harvested from right posterior superior iliac spine and graft placed between C1-C2 lamina. Incision is closed in layers over a drain.
Case 3
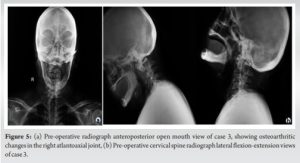
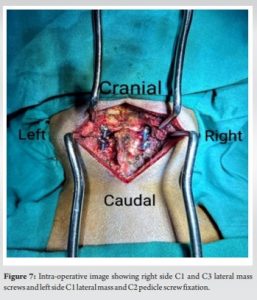
A 65-year-old female presented with complaints of neck pain for 6 months. The patient was on analgesics but had no relief. X-rays showed left-sided atlantoaxial facet joint osteoarthritis. The patient was given a trial of greater occipital nerve block following which the patient had pain relief but pain recurred after 3 weeks and hence the patient was advised surgery. The patient was managed with cervical lateral mass and pedicle screw rod construct with right-sided C1, C3 lateral mass screws and left C1 lateral mass and C2 pedicle screw fixation. At 3 months post-operative follow-up, the patient had complained of posterior skull numbness but had relief of the neck pain. At-2 year follow-up, the patient had complete relief of symptoms. (Fig. 5a, b and 6) show the pre-operative and post-operative radiographs of this case.

Surgical procedure
Under general anesthesia, the patient is positioned prone and the neck is held in alignment by skull tongs. The posterior midline approach is taken and C1-C3 vertebrae are exposed up to the lateral margin of cervical vertebrae. Bleeding typically arises from the venous plexus around the C1-C2 joint complex and should be effectively controlled with bipolar electrocautery, Gelfoam with thrombin, and cotton pledgets. The dorsal root ganglion of C2 is retracted in the caudal direction and the entry point for the C1 screw, which is the middle of the junction of the C1 posterior arch and the mid-point of the posterior inferior part of the C1 lateral mass. On the right side, C3 lateral mass screw was inserted. The entry point for the lateral mass screw is made in the infero-medial quadrant and the screw is directed laterally 25° and caudally along the line of an adjacent facet joint. On the left side, the C2 pedicle screw is placed. Entry point for the pedicle screw was made slightly lateral to the midpoint of the lateral mass and close to the inferior edge of the inferior facet joint of the caudally adjacent vertebra. The screw is angulated 25–45° medially and placed parallel to the adjacent facet joint in a sagittal plane. Rods connected on either side. Bone graft harvested from the right posterior superior iliac spine and graft placed around facet joints and between the lamina of C1-C2-C3. The incision is closed in layers over a drain. An intra-operative image from the procedure is provided in Fig. 7. Fig. 8 shows clinical photographs of the patient at follow-up.

Case 4
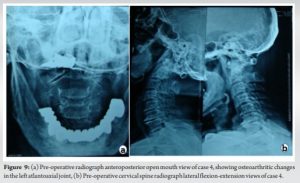
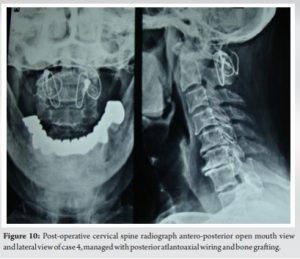
A 60-year-old male patient presented with a history of neck pain for 2 years and the patient demanded surgery at presentation to the clinic. Radiographs showed changes in AAOA on the left side. The patient was given a trial of conservative management with analgesics and a soft cervical collar. At 1-month follow-up, the patient reported a 25% improvement in pain but had partially restricted and painful neck movements. At subsequent follow-ups, the patient had persistent neck pain with gradually developing restriction of neck movements. An atlantoaxial facet block was given but the patient did not have much relief and hence was advised surgery. The patient was managed with atlantoaxial wiring and bone grafting. The patient had good pain relief post-surgery. (Fig. 9a, b and 10) show the pre-operative and post-operative radiographs of this case.
Surgical procedure
Under general anesthesia, the patient is positioned prone and the neck is held in alignment by skull tongs. The posterior midline approach is taken and C1-C2 vertebrae are exposed up to the lateral margin of the C1-C2 joint complex. C1-C2 alignment was checked under the image intensifier and a loop of SS wire passed on either side of the posterior tubercle of C1 and the other end passed through the holes made in the base of C2 and the wire loops were tightened. Bone graft harvested from right posterior superior iliac spine and graft placed between C1-C2 lamina. The incision is closed in layers over a drain.
AAOA remains an often unrecognized or misdiagnosed source of pain and the literature pertaining to AAOA has been limited. Conservative management has been the mainstay treatment of this condition but in the setting of incapacitating symptoms, surgical arthrodesis has become an accepted modality of treatment [4]. In this case series, we have described four cases of AAOA that were managed surgically (Table 1).
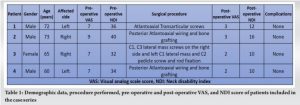
The mean age of the patients in our study was 67.5 years. The clinical symptoms in AAOA with very typical mostly unilateral occipitocervical pain aggravated by head rotation and restricted neck movement as reported in the literature were seen in all of our patients [5,6]. The diagnosis of AAOA was made on open-mouth radiographs and CT scans which showed reduced facet joint space, subchondral sclerosis, erosion, cystic degeneration, or osteophyte formation. All four patients in our series showed unilateral arthritis which has also been reported in other studies [7,8]. The posterior wiring technique which was the traditional method of fixation was associated with a high rate of pseudoarthrosis due to isolated posterior fixation [9-11]. The techniques of transarticular screw fixation and atlantoaxial lateral mass and pedicle screw and rod fixation have superior biomechanical stability and high fusion rates [12-14]. In our series, two patients were managed with posterior atlantoaxial wiring and bone grafting as we could achieve a stable construct and alignment with wiring in these patients, one patient was managed with atlantoaxial transarticular screws, one patient was managed with right-sided C1, C3 lateral mass screws and left side C1 lateral mass and C2 pedicle screw fixation. Although fusion between C1 and C2 reduces head rotation by 30–60 degrees, we found that all of our patients regained motion in the lower cervical spine once free of their pain. Only in patient number 4, neck extension was reduced postoperatively and was painful. The neck pain in this patient subsided gradually over the subsequent 4–6 weeks. Studies suggest that patients may experience significant pain relief post atlantoaxial fusion, with the typical paroxysmal occipital pain disappearing immediately after surgery [15]. In our study, a significant improvement in the post-operative VAS and NDI scores was noted at 2-year follow-up. The mean pre-operative VAS was 7.5 which improved to 2.5 postoperatively and the mean pre-operative NDI was 35.5 which improved to 12 postoperatively at 2-year follow-up. Thus, the mean difference in VAS score was 5, and the mean improvement in NDI was 23.5 which is clinically significant (the minimal clinically important difference of NDI is eight and VAS is one) [16,17]. In our study, four out of 108 patients required surgical intervention, which constituted around 3.70 % of the total patients. Similarly, in a study of 161 patients of C1-C2 transarticular screw fixation, only seven patients had degenerative AAOA as an indication for surgery which constituted 4.3% of the total study population [18]. None of the cases described in our case series had any major complications such as vertebral artery injury, neurological deficits, or risk to life. Several other studies have also reported no major complications with atlantoaxial fixation [19,20].
Only a small proportion of cases among patients with painful and debilitating degenerative AAOA requires surgical intervention. Atlantoaxial fusion has proved to be an effective treatment with a low rate of serious complications. The patients self-rated outcome in terms of mean improvement in the post-operative VAS and NDI scores indicate a high degree of satisfaction with the surgical mode of treatment.
AAOA is a rare entity and is often missed to be diagnosed by clinicians. Although occipitocervical pain is the classical presenting symptom, some may also present with visual problems, retro-orbital, or retro-mastoid pain. Conservative management is the mainstay treatment of this condition but surgical management may be indicated in very few cases who are not responding to conservative treatment.
References
- 1.Zapletal J, de Valois JC. Radiologic prevalence of advanced lateral C1- C2 osteoarthritis. Spine (Phila Pa 1976) 1997;22:2511-3. [Google Scholar | PubMed]
- 2.Dreyfuss P, Michaelsen M, Fletcher D. Atlanto-occipital and lateral atlanto-axial joint pain patterns. Spine (Phila Pa 1976) 1994;19:1125-31. [Google Scholar | PubMed]
- 3.Whitesides TE Jr., McDonald AP. Degenerative arthritis of the occipitocervical region-signs and symptoms. Orthop Trans 1978;2:32. [Google Scholar | PubMed]
- 4.Kuklo TR, Riew KD, Orchowski JR, Won DS, Schroeder TM, Gilula LA. Management of recalcitrant osteoarthritis of the atlanto-axial joint. Orthopedics 2006;29:633-8. [Google Scholar | PubMed]
- 5.Star MJ, Curd JG, Thorne RP. Atlantoaxial lateral mass osteoarthritis. A frequently overlooked cause of severe occipitocervical pain. Spine (Phila Pa 1976) 1992;17:S71-6. [Google Scholar | PubMed]
- 6.Halla JT, Hardin JG Jr. Atlantoaxial (C1-C2) facet joint osteoarthritis: A distinctive clinical syndrome. Arthritis Rheum 1987;30:577-82. [Google Scholar | PubMed]
- 7.Grob D, Magerl F. Surgical stabilization of C1 and C2 fractures. Orthopade 1987;16:46-54. [Google Scholar | PubMed]
- 8.Ehni G, Benner B. Occipital neuralgia and the C1-2 arthrosis syndrome. J Neurosurg 1984;61:961-5. [Google Scholar | PubMed]
- 9.Brooks AL, Jenkins EG. Atlantoaxial arthrodesis by the wedge compression method. J Bone Joint Surg 1978;60-A:279-84. [Google Scholar | PubMed]
- 10.Gallie WE. Fractures and dislocations of the cervical spine. Am J Surg 1939;46-A:495-9. [Google Scholar | PubMed]
- 11.Farey ID, Nadkarni S, Smith N. Modified Gallie technique versus transarticular screw fixation in C1-C2 fusion. Clin Orthop Relat Res 1999;359:126-35. [Google Scholar | PubMed]
- 12.Grob D, Crisco J, Panjabi M, Wang P, Dvorak J. Biomechanical evaluation of four different posterior atlantoaxial fixation techniques. Spine (Phila Pa 1976) 1992;17:480-90. [Google Scholar | PubMed]
- 13.Grob D. Surgery in the degenerative cervical spine. Spine (Phila Pa 1976) 1998;23:2674-83. [Google Scholar | PubMed]
- 14.Suchomel P, Stulik J, Klezl Z, Chrobok J, Lukas R, Krbec M, et al. Transarticular fixation of C1-C2: A multicenter retrospective study. Acta Chir Orthop Traumatol Cech 2004;71:6-12. [Google Scholar | PubMed]
- 15.Schaeren S, Jeanneret B. Atlantoaxial osteoarthritis: Case series and review of the literature. Eur Spine J 2005;14:501-6. [Google Scholar | PubMed]
- 16.Carreon LY, Glassman SD, Campbell MJ, Anderson PA. Neck disability index, short form-36 physical component summary, and pain scales for neck and arm pain: the minimum clinically important difference and substantial clinical benefit after cervical spine fusion. Spine J 2010;10:469-74. [Google Scholar | PubMed]
- 17.Myles PS, Myles DB, Galagher W, Boyd D, Chew C, MacDonald N, et al. Measuring acute postoperative pain using the visual analog scale: The minimal clinically important difference and patient acceptable symptom state. Br J Anaesth 2017;118:424-9. [Google Scholar | PubMed]
- 18.Grob D, Jeanneret B, Aebi M, Markwalder TM. Atlanto-axial fusion with transarticular screw fixation. J Bone Joint Surg Br 1991;73:972-6. [Google Scholar | PubMed]
- 19.Pakzaban P. Transarticular screw fixation of C1-2 for the treatment of arthropathy-associated occipital neuralgia. J Neurosurg Spine 2011;14:209-14. [Google Scholar | PubMed]
- 20.Harms J, Melcher RP: Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine (Phila Pa 1976) 2001;26:2467-71. [Google Scholar | PubMed]