In this case series, we have explored the importance of Phenol chemical neurolysis of stellate ganglion in Buerger’s disease of hands.
Dr. Rampal Singh, Department of Anaesthesiology, All India Institute of Medical Sciences, Raipur, Chhattisgarh, India. E-mail: lautikasingh@gmail.com
Introduction: Buerger’s disease is common in 74.70% of cases in the lower limb but in 20.20% of cases, it is found in the upper limb or hand. The disease usually starts from pain in the finger/thumb or hand and then to more centrally. Patients presented with pain in the hand with gangrene of fingers. Pain aggravated on lifting hand above the shoulder level or above heart level in upright or lying in the bed, respectively.
Case Report: In almost all patients, there was a history of smoking except one and all patients had involvement of digits of the right or left hand. Diagnosis of Buerger’s disease was made based on the history of smoking, weak or absent pulse, lack of bleeding, swelling, edema, blackening, stony hard fingers or thumb on clinical examination, and color Doppler study of the limb. In all patients, Stellate ganglion chemical neurolysis with 8% phenol was done at C7-T1 under fluoroscopic and radiocontrast dye (Iohexol 300) guidance. After successful neurolysis patients got excellent pain relief, their wounds started healing, the vascularity of the diseased part increased and the disease stopped progressing.
Conclusion: Stellate ganglion chemical neurolysis with phenol in Peripheral vascular disease or Buerger’s disease of hand is an effective method to stop the disease procession, promoting wound healing, controlling ischemic pain, and avoiding surgical amputation.
Keywords-: Hand and finger gangrene, stellate ganglion phenol chemical neurolysis, peripheral vascular disease of hand or Buerger’s disease of hand.
Thromboangiitis obliterans is a segmental occlusive inflammatory disease of arteries and veins, characterized by thrombus formation in vessels and recanalization of the affected vessels, is a non-atherosclerotic inflammatory disease affecting small and medium-sized arteries and veins of the upper and lower extremities. Disease is found worldwide, prevalence varies from low 0.5–5.6% in Western Europe and 45–63% in India, 16–66% in Japan and Korea, and 80% among Ashkenazi Jews [1]. Smoking is common in India and so is the incidence of Buerger’s disease among young male smokers [2]. The upper limb is involved in 20.2% of cases [3]. Men-to-women ratio is 100:1, but in recent years, more affected women have been reported in the medical literature, men-to-women ratio may be 10:1 [4]. There has been the involvement of radial and ulnar arteries, 11.4% and 11.5%, respectively. Different surgical treatments such as surgical bypass, surgical sympathectomy (49.5%), amputation (22.8%), and others have been suggested [5]. There is one article in which authors used Lignocaine and Bupivacaine with Ketamine but did not perform phenol chemical neurolysis of stellate ganglion for Buerger’s disease of hand [6]. In another report, authors used phenol chemical neurolysis in head-and-neck cancer pain but not in Burger’s disease of hand [7]. We could not find more information regarding the role of phenol chemical neurolysis in Buerger’s disease of hand. In this case series, we are discussing patients suffering from peripheral vascular disease (Buerger’s Disease) of the hand, aged between 35 and 65 years from October 2015 to March 2022. We tried to save their limb by percutaneous neurolysis of stellate ganglion with 8% phenol, a non-surgical minimally invasive pain and spine intervention (MIPSI) under C-Arm guidance.
Case no. 1
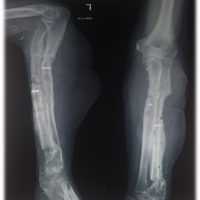
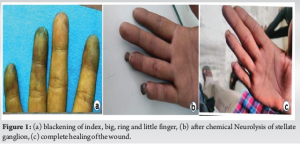
A gentleman (45 years) presented to us (October 2015) with complaints of blackening of fingers and thumb of the right hand, swelling, and burning pain for the past 2 months. On examination, there was swelling over all fingers, the skin was shiny black and painful to touch. Pulse was minimally palpable at the ulnar and radial artery at the wrist. There was nil bleeding at the affected site when checked with a needle. On the visual analogue score (VAS) scale, the pain was 9/10. The patient had a history of chronic smoking for at least 20 years (Table 1).
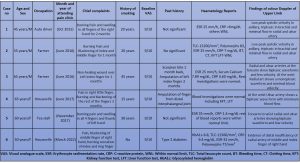
His blood investigations were within normal limits except for erythrocyte sedimentation rate (ESR) 25 mm/h and C-reactive protein (CRP) <6 mg/dL color Doppler of right hand shows low peak systolic velocity in axillary, triphasic in brachial, and minimal flow in the radial and ulnar artery (Table 1). After 3–4 blocks of the stellate ganglion with 0.25% of Bupivacaine, there was a line of demarcation between live and gangrenous tissue. Patient follow-up events are shown in Table 2. With due course of time, the gangrenous part of the fingers detached itself and there was no need for amputation (Fig. 1 a, b, c).
Case no. 2
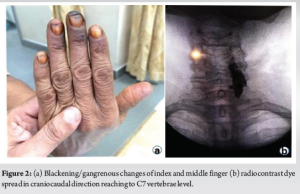
A gentleman (55-year, farmer) presented in the pain clinic (June 2016) with complaints of blackening and burning pain in the index and big finger of his right hand for the last 1 and half months (Table 1). The pain was associated with lifting the hand above the shoulder or heart level. Pain used to decrease while hanging the hand down by the side of the body. The patient had a chronic history of smoking for the past 25 years. The patient’s pain on the VAS scale (9/10) and haematology was within normal limits except for total leukocyte count (TLC)-15200/mm3, polymorphs 83%, ESR 25 mm/h, and CRP-7 mg/dL. The rest of the blood investigations were within normal range. Color Doppler of the right upper limb shows low peak systolic velocity in axillary vessels, very low and altered triphasic flow in the brachial artery, and minimum vein-like monophasic flow in the radial and ulnar artery (Table 1). After successful treatment with phenol (8%) chemical neurolysis of stellate ganglion, the patient’s finger was saved and the VAS score came down to 1/10 after 3 months and disappeared (0/10) after 4–5 months after chemical neurolysis (Table 2). The patient had proper antibiotic coverage to cover leukocytosis (Fig. 2 a and b).
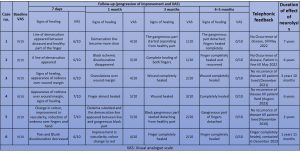
Case no. 3
A gentleman (65 years) farmer by occupation presented in our pain clinic (February 2017) with complaints of pain and a non-healing wound in the index finger of the left hand with a history of scorpion bite 2 months back. Although he had amputation of the finger 1 month back for blackening due to gangrene but remaining stump did not heal and again became black and was associated with severe pain. On the VAS scale, his pain was 9/10. The patient had a history of smoking for around 50 years. Radial and ulnar pulse was almost absent and difficult to palpate. Except for ESR (25 mm/h), blood reports were within normal limits. Color Doppler of the left hand shows biphasic waveforms and less velocity in radial and ulnar arteries at the forearm level. At the wrist, the radial artery shows a monophasic waveform and minimal blood velocity of blood. The rest of the investigations were within the normal range (Table 1). There was excellent pain relief and healing of the wound after chemical neurolysis with 8% phenol. The patient had complete healing of the wound and pain relief after 3 and 4–5 months of follow-up, VAS 1/10, and 0/10, respectively (Table 2). There was no recurrence of the disease till he lived (May 2022), the patient died due to age-related problems not associated with the disease.
Case no. 4
A woman aged 65 years presented (December 2017) with complaints of burning pain over her right little finger last 3 months. She had had an amputation of her finger 12 days back due to blackening. Even after amputation pain did not resolve and the remaining part of the finger again became black due to gangrene with pain. The patient had a long history of smoking and tobacco chewing. On the VAS her pain score was 9/10. Color Doppler study of the right arm revealed a biphasic wave at the ulnar artery with minimum blood flow. Her blood reports were within normal limits (Table 1). Her pain decreased to 7/10, 5/10/, 3/10, and 0/10 (VAS) at 7 days, 1, 3, and 4–5 months, respectively, after phenol chemical neurolysis. There was no recurrence of the disease in her finger till she lived (August 2023) when she died due to myocardial infarction as told by her relatives on telephonic contact.
Case no. 5
A female patient aged 60 years presented to us (June 2017) with complaints of burning pain, swelling, and blackening of all fingers including the thumb of the left hand for the past 3 months (Fig. 3a and b). She had a long history of “Bidi” smoking and tobacco chewing. On the VAS scale, her pain score was 9/10. On examination, fingers were gangrenous, dried stony hard, and black from fingertip to proximal interphalangeal joint. There was scarce bleeding proximal to gangrenous parts of the involved fingers. She used to hang her hand while sleeping in bed. Color Doppler study shows biphasic blood flow and low velocity in the radial and ulnar artery from forearm to wrist. Her blood investigations were within normal limits (Table 1). On the 7th day of neurolysis, there was a clearcut demarcation between the live and gangrenous part of the fingers and thumb (Fig. 3e). After 1 month, there was more improvement in the vascularity and clear demarcation (Fig. 3c) of the hand. After 3 months, the gangrenous part of the fingers started separating from the healthy part. After 4–5 months, the gangrenous part detached without surgical intervention (Fig. 3d and Table 2). Pain score came down to 2/10 from 9/10 after 3 months and there was no pain after 4–5 months. There was no recurrence of the disease till she lived (April 2022).

Case no. 6
A female patient 45 years old (house maker) presented to us (March 2022) with complaints of burning pain and blackening of the big and ring finger of the right hand for the past 25 days (Fig. 4 a and b). Her pain score (VAS) was 9/10. The patient had no history of smoking or tobacco chewing. The big finger was more affected than the ring finger. The patient was diabetic and was taking Metformin 500 mg once a day. Glycosylated haemoglobin (HbA1c) was 6.8, CRP 9.4 mg/dL, ESR 32 mm/h, and TLC was 11500/mm3. Color Doppler of right-hand shows evidence of distal insufficiency of radial artery of middle and index finger of right hand (Table 1). Her diabetes mellitus was well controlled. Metformin was continued and antibiotic coverage was given to control infection with Cefuroxime axetil 250 mg twice daily orally. After successful stellate ganglion neurolysis, the patient got excellent pain relief and her VAS score was 6/10, 4/10, 2/10, and no pain at 7 days, 1, 3, and 4–5 months. After 3 months, the gangrenous distal part of the finger detached from the proximal live part (Fig. 4 c and d; Table 2).

The total duration of the effect of chemical neurolysis with 8% phenol in individual patient is shown in Table 2. This case series was carried out at Rohilkhand Medical College and Hospital, Bareilly, Uttar Pradesh, India.
Stellate ganglion neurolysis
The night before the procedure patients were kept nil by mouth as per standard NPO guidelines. After shifting patients in the operation theatre, all anaesthesia machine, equipments, and monitors were checked. Patients were monitored according to ASA (American Standard of Anaesthesia) Monitoring. Eighteen Gauge (18G) intravenous cannula was secured in a healthy hand and Ringer’s Lactate solution was given except for 6th patient in which 0.9% Normal Saline due to having Diabetes Mellitus.
Position
Patients were kept supine on a C-Arm (fluoroscope/image intensifier) compatible table with a pillow under the shoulders and a roll was kept under the neck to bring the neck in the extended position to maximally expose the cervical area. The part was painted with an antiseptic solution and draped. Patients were under light sedation with 1 mg of midazolam during the procedure.
Technique
First of all, the cervical area was visualized under fluoroscopic anteroposterior view then vertebral end plates were aligned. After obtaining a proper anterolateral (AP) fluoroscopic view, the lateral mass of the sixth vertebra was marked with the help of a radio-opaque marker. Injection site on skin marked and infiltrated with 1 mL of 2% Lignocaine. After this, a, 22G spinal needle was placed on the infiltrated site and directed toward the lateral mass and body of the sixth cervical vertebrae under intermittent AP (Fig. 3e and 5a) and lateral fluoroscopic views (Fig. 5b).
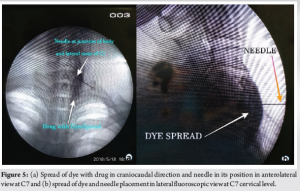
Patients were instructed not to deglutate during the procedure as this displaces the needle from the target site. After hitting the needle tip to the bony surface needle, it was retracted 1–2 mm. During the procedure, intermittent AP and lateral fluoroscopic images were taken to confirm the position and depth of the needle. Needle placement was confirmed with 1–2 ml of Iohexol 300 radio-opaque dye. Proper placement of the needle was confirmed with dye spread in the cranio-caudal direction. Then, 10 mL of 0.25% bupivacaine with 4 mg Dexamethasone was injected. Successful ganglion block was confirmed by redness of the eye or congestion of the conjunctiva, dropping of the eyelid, enophthalmos, 1–2° rise in temperature of the involved hand and vasodilation. In all patients, 4–5 such blocks were repeated on a daily or alternate day. When there was a clear line of demarcation, redness of the involved lived part, the disappearance of oedema, and good to excellent pain relief, chemical neurolysis was done with 3–4 mL of 8% phenol mixed with 1 mL of Iohexol 300 at C7 level under live fluoroscopic guidance to avoid intra-arterial injection of phenol. Before phenol injection, 1 mL of 2% lignocaine was injected as phenol causes pain on injection. In all patients, the procedure was accomplished uneventfully. After the procedure, patients were observed for at least 2 h in the post-anesthesia care unit. Patients received pharmacological treatment including Cilastazole 100 mg, Asprin 75 mg (blood thinners), Tramadol in combination with Paracetamol (pain relief), Isoxpurine 10–20 mg, Isosorbide mononitrate 10 mg (vasodilators), Pregabalin 75 mg (neuropathic pain) orally, and Methylcobalamine. For patients having wet gangrene, pus was sent for culture and sensitivity and antibiotics coverage was given accordingly.
Buerger’s disease is a nonatherosclerotic, segmental, inflammatory disease that most commonly affects the small to medium-sized arteries and veins of the extremities [8]. It usually affects males more than females with a ratio of 100:1 [4]. Aetiology remains unknown but involves tobacco exposure (sine qua non), hereditary susceptibility, immune response, and coagulation change [3]. Patients presented to our pain clinic belonging to low socioeconomic status and labour class and almost all except one (Case no. 6) had a history of “Bidi” (tobacco is wrapped in the leaf of Tendu plants [Diospyros melanoxylon]) smoking [9], native to India and Sri Lanka. In India’s low socioeconomic strata, the labour class takes tobacco as smoking in the form of “Bidi” [10]. The disease usually begins with ischemia of the distal small vessels of the arms, legs, hands, and feet. Patients may present with claudication of the hands, arms, legs, and feet. In peripheral vascular disease including Buerger’s disease pain typically begins in the extremities. As the disease progresses, ischemic pain at rest and ischemic ulcerations [1] on the fingers or thumb may develop. All patients had complaints of rest pain especially while lifting the arm above shoulder level in an upright position or above heart level while lying in the bed. Some patients had dry gangrene showing an ischemic nature of pain which was associated with a burning pain indicating ischemia leading to injury of tissue and nerves causing pain along with neuropathic complaints in the form of burning sensation. This all happens because of impaired circulation to the limb due to complete or partial blockage of vessels. Color Doppler of the affected limb shows low peak systolic velocity in the axillary artery and biphasic in the radial or ulnar artery. The affected fingers and hands were cold and calm due to the blockade of vessels by inflammation and thrombus. In this case series, one patient (Case no. 3) had a history of scorpion bite 2 months back along with smoking and presented to us with amputation of a finger. This patient had double risk factors causing gangrene. In literature, authors have found gangrene following scorpion bite. Scorpion venom is it self a significant factor causing gangrene by the formation of thrombus in arteries [11,12]. Quitting smoking and tobacco products in any form is the mainstay of treatment. Many authors have described different treatment options in the literature. Stellate ganglion block (STGB) with ketamine (NMDA receptor blocker) has been used for the treatment of peripheral vascular disease in the hands [6]. Spinal cord stimulation has been used for Buerger’s and Raynaud’s disease of the upper limb by Ertilav and Aydin; Ryu et al. [13,14]. We decided to do chemical neurolysis of the stellate ganglion as sympathetic supply to the head, neck, and upper limb is derived from T1-9 segments, and passes through the stellate ganglion (C5-T1). The stellate ganglion (2.5 cm × 1 cm × 0.5 cm) lies over the neck of the first rib, between C7 and T1. The most common approach for STGB is paratracheal, at the level of C6th Chassaignac’s tubercle. The somatic branches from the stellate ganglion are the grey rami communicants providing sympathetic fibres to the anterior rami of the C7, C8, and T1. It gives off sympathetic nerve branches to the brachial plexus, which lies laterally, as well as tributaries to the subclavian and vertebral arteries and the brachiocephalic trunk [15]. Angiogenesis or neovascularization takes place in response to hypoxia to tissue resulting in collateral formation; necessary for wound healing and is a physiological response to tissue hypoxia during ischemia [16]. As pain is a sympathetically mediated phenomenon, blockade of ganglion produces pain relief, vasodilation, rise in temperature 1–2° centigrade, and other signs such as miosis, enophthalmos, redness of the conjunctiva, and dropping of the eyelid. Serial blockade of ganglion on daily or alternate days in peripheral vascular disease promotes pain relief and increases vascularity and wound healing. Blockade of ganglion promotes vasodilation of collaterals developed following ischemia. The effect of blockade with 0.5% Bupivacaine lasts for at least 7 days [17], so 4–5 serial blocks were given under C-Arm guidance followed by chemical neurolysis with 3–4 mL of 8% Phenol mixed with 0.25% Bupivacaine and 4mg Dexamethasone. Phenol denatures the protein of neural structure when injected, leading to loss of cellular fatty content, separating myelin sheath from the axon, followed by axonal edema [18]. Small amounts of steroid were added to reduce neuritis caused by phenol. The preganglionic axons leave the T1 and T2 ventral roots, pass through the white communicating rami, join the sympathetic chain, and ultimately synapse at the inferior (stellate), middle, or superior cervical ganglion [19]. Racz and Holubec used a solution of 2.5 mL of 6% phenol in saline, 1 mL of 80 mg methylprednisolone, and 1.5 mL of 0.5% bupivacaine (giving a 3% phenol solution) to perform a neurolytic block of the stellate ganglion [20]. We used 5–6 mL of drug volume consisting of 3–4 mL of 8% Phenol instead of 6%, 1 mL of Dexamethasone, and 1 mL of 0.25% Bupivacaine and did not find any adverse event in any patient. Phenol has been used in different concentrations ranging from 3% to 12% for neurolysis in different studies [18]. Aspirin is a drug with antiplatelet and anti-inflammatory properties useful to prevent further arterial occlusion and has been recommended in different dosages ranging from 75 to 325 mg orally after meals. On the other hand, Cilastazole is also an antiplatelet drug and was approved for peripheral vascular diseases by the food and drug administration in 1999. Cilostazol inhibits specifically Type III cellular phosphodiesterase, which affects reversible inhibition of platelet aggregation and has a “steal” phenomenon (diverting blood to the ischemic limb by unequal vasodilation). The dose ranges from 50 to 200 mg/day [3]. Isosorbide mononitrate belongs to the nitrate group causing vasodilation by releasing nitric oxide (NO), an endothelium-derived relaxing factor. Nitric Oxide is endogenously produced in the endothelium to dilate the blood vessels. Collaterals that have developed secondary to ischemia, get dilated by sympathetic cut-down and vasodilators such as isosorbide dinitrate or mononitrates [21]. Pregabalin (75 mg) successfully alleviates symptoms of neuropathic pain and is an antagonist of voltage-gated Ca2+ channels which binds to the alpha-2-delta subunit to produce antiepileptic and analgesic actions [21,22].
Stellate ganglion chemical neurolysis with a neurolytic agent such as phenol (3–4 mL of 8%) with 0.25% bupivacaine is an effective treatment method to stop pain, promoting healing of digital ulcer and increasing vascular supply in the affected area in patients suffering from peripheral vascular disease or Buerger’s disease for a maximum of 7 years. Ganglion neurolysis is a cost-effective technique. Fluoroscopic guidance and the use of radiocontrast dye during the procedure increase the effectiveness and safety of the procedure.
Chemical neurolysis of stellate ganglion by phenol in patients suffering from Buerger’s disease or peripheral vascular disease of hand is a cost-effective MIPSI. The procedure’s safety and efficacy are increased with contrast use and fluoroscopy guidance.
References
- 1.Arkkila PE. Thromboangiitis obliterans (Buerger’s disease). Orphanet J Rare Dis 2006;1:14. [Google Scholar | PubMed]
- 2.Singh R, Shukla A, Kang LS, Verma AP. Chemical lumbar sympathetic plexus block in Buerger’s disease: Current scenario. Indian J Pain 2014;28:24-8. [Google Scholar | PubMed]
- 3.Cacione DG. Buerger’s disease: Clinical aspects and evidence-based treatments. In: Vasculitis in Practice-an Update on Special Situations-Clinical and Therapeutic Considerations. London: Intech Open; 2018. [Google Scholar | PubMed]
- 4.Rare Diseases Archive-NORD National Organization for Rare Disorders. Danbury: NORD National Organization for Rare Disorders; 2019. Available from: https://rarediseases.org/rare-diseases [Last assessed: 2007 Sep 23] [Google Scholar | PubMed]
- 5.Salimi J, Cheraghali R, Omrani Z, Farshidmehr P, Afghani R. Surgical treatment options for Buerger’s disease (Experience with 315 cases in Iran). Med J Islam Repub Iran 2022;36:134. [Google Scholar | PubMed]
- 6.Kulkarni KR, Kadam AI, Namazi IJ. Efficacy of stellate ganglion block with an adjuvant ketamine for peripheral vascular disease of the upper limbs. Indian J Anaesth 2010;54:546-51. [Google Scholar | PubMed]
- 7.Ghai A, Kaushik T, Kumar R, Wadhera S. Chemical ablation of stellate ganglion for head and neck cancer pain. Acta Anaesthesiol Belg 2016;67:6-8 [Google Scholar | PubMed]
- 8.Piazza G, Creager MA. Thromboangiitis obliterans. Circulation 2010;121:1858-61. [Google Scholar | PubMed]
- 9.Sharma OP, Prasad V. Plant species used as ‘Bidi Leaves’ in India: A Non-timber forest product. Asian Reson 2015;4:120-1. [Google Scholar | PubMed]
- 10.Kothari R, Maharaj A, Tomar T, Agarwal P, Sharma D. Percutaneous chemical lumbar sympathectomy for Buerger’s disease: Results in 147 patients. Indian J Vasc Endovasc Surg 2017;4:185-90. [Google Scholar | PubMed]
- 11.Halbhavi SN, Karikazi MA, Mallapur AS, Manjula R, Vishwanath G, Kolhar BA. Case series local gangrene due to scorpion sting. Med Innov 2017;6:39-43. [Google Scholar | PubMed]
- 12.Ansari MY. Gangrene after scorpion sting. Br Med J 1948;2:388. [Google Scholar | PubMed]
- 13.Ertilav E, Aydin ON. Spinal cord stimulator for the treatment of ischemic pain-Burger’s disease and Raynaud’s disease: A report of two cases and literature review. Agri 2022;34:316-21. [Google Scholar | PubMed]
- 14.Ryu SW, Jeon HJ, Cho SS, Choi RM, Yoon JS, Ko HS, et al. Treatment of digit ulcers in a patient with Buerger’s disease by using cervical spinal cord stimulation-a case report. Korean J Anesthesiol 2013;65:167-71. [Google Scholar | PubMed]
- 15.Mehrotra M, Reddy V, Singh P. Neuroanatomy, stellate ganglion. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539807 [Last accessed on 2023 Jul 24]. [Google Scholar | PubMed]
- 16.Tsai SH, Huang PH, Chang WC, Tsai HY, Lin CP, Leu HB, et al. Zoledronate inhibits ischemia-induced neovascularization by impairing the mobilization and function of endothelial progenitor cells. PLoS One 2012;7:e41065. [Google Scholar | PubMed]
- 17.Ferrillo MG. Treatment of complex regional pain syndrome with stellate ganglion local anesthetic blockade: A case report of one patient’s experiences with traditional bupivacaine HCl and liposome bupivacaine. Clin Case Rep 2016;4:861-5. [Google Scholar | PubMed]
- 18.D’souza RS, Warner NS. Phenol Nerve Block Continuing Education Activity. Available from: https://www.ncbi.nlm.nih.gov/books/NBK525978 [Last Assessed: 2023 Aug 28] [Google Scholar | PubMed]
- 19.Raj PP, Erdine S. Interventional pain procedures in the neck. In: Pain‐Relieving Procedures: The Illustrated Guide. United Kingdom: John Wiley and Sons, Ltd.; 2012. p. 208. [Google Scholar | PubMed]
- 20.Racz GB, Holubec JT. Stellate ganglion phenol neurolysis. In: Racz GB, editor. Techniques of Neurolysis. Current Management of Pain. Vol 4. Boston, MA: Springer; 1989. [Google Scholar | PubMed]
- 21.Balasubramanian S, Chowdhury YS. Isosorbide. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557839 [Last accessed on 2023 May 16]. [Google Scholar | PubMed]
- 22.Essmat N, Galambos AR, Lakatos PP, Karádi DÁ, Mohammadzadeh A, Abbood SK, et al. Pregabalin-Tolperisone combination to treat neuropathic pain: Improved analgesia and reduced side effects in rats. Pharmaceuticals (Basel) 2023;16:1115. [Google Scholar | PubMed]