In this article we look at current status of Robotic total knee replacement as it is rapidly introduced world wide with scant early evidence to support its use. We have carefully analyzed pros and cons of its use and attempted to advocate watchful introduction of the technology to minimize harm while maximizing its advantages. Robotics is a powerful tool which still needs integration with artificial intelligence using advanced data analytics to be able to improve current practices. Instead of rapid indiscriminate introduction for marketing benefits, we need to develop it diligently to be able to improve outcomes of Total Knee Replacement.
Dr. Munish Sood, Department of Orthopaedics, INHS Asvini, Mumbai - 500004, Maharashtra, India. E-mail: soodmunishafmc@gmail.com
Abstract: Today, the total knee replacement (TKR) is considered as one of the most successful orthopedics surgeries. The effective long-term pain relief, deformity correction, and restoration of function that it provides have resulted in a large number of these procedures being performed worldwide. It has been observed that 15–20% of patients are not satisfied even after successful TKR surgery. Various attempts such as careful patient selection, pre-operative education, optimization of patients before the surgery, expeditious and precise surgery, aggressive pain control, early return to home, and rehabilitation have been made to improve outcomes and satisfaction among patients. There are also attempts at designing newer implants and introducing smart technology like navigation and Robotics to improve the precision of surgery. In this letter, we look at the pros and cons of the rapid introduction of Robotics in the practice of total knee arthroplasty.
Keywords: Joint replacement, Robotics, Conventional knee replacement
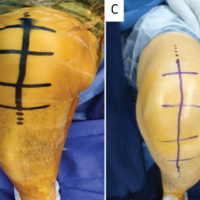
Joint replacement is one of the most successful surgical procedures till date; it remains a sought-after surgery as we seek an active long life [1]. While hip replacement achieves a very high patient satisfaction [2], total knee replacement (TKR) still leaves some patients (10–15%) dissatisfied [3]. While the reason for the same remains elusive, the industry continues to innovate and introduce tools to improve the precision of the procedure in an attempt to improve patient satisfaction. Contemporary technique of TKR using manual jigs and instrumentation coupled with modern design implants has assured reproducible results and excellent survival. The art and science of TKR are now well understood and ease of skill transfer has ensured a large proportion of young surgeons and even residents under supervision performing the procedure with reproducible results. However, with a proposed aim to minimize human error, there has been a push to introduce navigation and robotics into the field of TKR for the last three decades. Robotic surgery does increase precision and reduce outliers but the alignment goal is as per the inputs given by the surgeon and is still prone to human error of judgment. When the Robodoc [4] platform was introduced more than three decades back, most who used it, felt it was an expensive and futile endeavor. It had a cumbersome workflow with detailed pre-operative computed tomography (CT) image-based planning by the surgical team, a fully robotic arm (Active Robot) taking over controls but failing to reproduce the desired accuracy, extended surgical time, and the prohibitive cost of expendables with no perceived clinical benefits. The current generation of robots uses burrs and saws which are integrated with computers and graphics to give a visual representation of the thought process and surgical execution which allows the surgeon to perform the bone cuts while incorporating an active stop to improve accuracy (Semi Active Robot). Another option made available recently is a passive Robot arm which helps placing the bone-cutting jig in the right place in three dimensions. This will no doubt help surgeons in training and also invariably provide documentation of the surgery which can be stored on the cloud. However, there is a definite change in surgical workflow for surgeons used to doing conventional surgery. Robot-assisted total knee arthroplasty (TKA) requires unlearning certain steps and learning new ones to execute the procedure accurately. The surgeon deals with an extra person – the robot engineer and computer screen in his surgical field of vision. The numbers and graphs can be disorienting and can divert the attention from the feel of the soft-tissue balance. Chasing numbers and avoiding feel proprioception during various stages of a TKA can alienate the surgeon from the attention to soft tissue ligamentous envelope which plays a role in deformity obvious in long-standing degenerative osteoarthritis. The pre-operative planning tools and intraoperative use of a robotic arm are not intuitive to all and introduce a learning curve. On top of this, each company has introduced different surgical planning, workflow, and method of executing the surgery which makes cross-learning extremely challenging. It also locks the surgeon or institute to a given company robotic technique and use of its specific implants. This steals away the freedom of the operating surgeon and the institute to choose an implant or technique which could have an ethical and financial conflict of interests thus affecting patient care. An open platform Robot which allows use of any implant is only at present provided by a single manufacturer internationally. Two decades back Europe saw extensive research and training activities happening to develop navigation and robotic tools for fracture fixation surgery, the utility of those techniques using intraoperative 3D CT, image-free navigation, and robotic arms for fracture reduction in complex periarticular and pelvi-acetabular trauma was exciting. Navigation and robotics helped in complex fracture care but for certain commercial interests, Robotics and navigation have changed their focus onto TKR as the preferred area of interest trying to overengineer an already successful procedure. Till date, there is no clinical evidence to show the superiority of robotics in TKR [5,6]. There is some evidence to show that navigation and robotics can reduce outliers of implant alignment by performing the bone cuts in a precise manner as planned by the surgeon but does that translate into improved patient satisfaction and better longevity? Currently, no evidence exists. Some proponents of robotic TKR say that it can help restore the native anatomy, kinematics, and alignment which still remains elusive. Creating native anatomy or restoring pre-disease alignment needs customized implants, in addition to the restoration of capsuloligamentous tensions throughout the range of movement which is not possible with present robot-assisted TKR(RaTKR). Present-day RaTKR uses off the shelf prefabricated implants of defined design which evolved in the mechanical alignment era. The size range allows the best on table match for the patient. All the robotic systems presently available in the market use tracker-based optical evaluation of gaps throughout the range of movement with total disregard to ligamentous tension and joint loading. What would be helpful is pressure transducers which can give a number to the surgeon-induced “stress and feel” while taking the knee through its range of motion during various stages of the operation. These are being developed but still not integrated in any of the available systems. Incorporation of this data using machine learning and artificial intelligence (AI) algorithms with robotics will add more value and as more and more data gets captured the system can learn and evolve. An experienced surgeon putting data in would evolve the robot faster than a beginner surgeon would. If the robot has machine learning and AI embedded, then this big data over time would help the next surgery workflow more effectively. In spite of these shortcomings, there remains a constant thrust from the industry and institutes to introduce RaTKR where the need is not felt by most surgeons. It is still not understood that by merely ensuring precision in bone cuts how can the robotic arm increase patient satisfaction. The longevity of the implant is not only a function of alignment but is also affected by fixation and balance which robotics has no role to play in cementing and balancing as yet. In its present form, TKR is an easy-to-learn, reproducible surgery which has a very high success rate. As senior arthroplasty surgeons, the authors feel that while the enthusiasm and impatience of the industry and young technology-friendly surgeons are welcome, we need to titrate the introduction of this technology. RaTKR needs to establish credible evidence to justify the clinical need to be introduced on a large scale. The administrators need to look at socioeconomic benefits looking at the cost to the society vis-a-vis patient satisfaction and survival advantage provided by this technology. While this happens, we remain concerned that the rapid introduction of this technology with limited training and evidence could harm our unsuspecting clientele enamored by the media propaganda of robotic joint replacement surgery. The likely harm to patients undergoing RaTKR while surgeons are switching over and are in their learning curve is not improbable. Similarly, if the use of technology increases procedure-related complications such as infection, periprosthetic fractures, and instability, who will be answerable to the patients? This ethical issue to introduce robotics into TKR and risk increase in these complications is something to ponder about. The need of the hour is a gradual, vigilant, and scientific introduction of RaTKR, while concurrently creating evidence and support for this exciting technology which should be surgeon-driven and not industry-driven! At present, there are different philosophies of various industry-lead robotics systems and this innovation will not be available readily and cost-effectively for a few more years at least, so the impact will be only for a chosen few and not a vast populace. While robotics is here to stay and evolve let us ensure that at no point do we compromise patient’s interests and let us not throw the baby out with the bathwater!
References
- 1.Crowninshield RD, Rosenberg AG, Sporer SM. Changing demographics of patients with total joint replacement. Clin Orthop Related Res 2006;443:266-72. [Google Scholar | PubMed]
- 2.Mellon SJ, Liddle AD, Pandit H. Hip replacement: Landmark surgery in modern medical history. Maturitas 2013;75:221-6. [Google Scholar | PubMed]
- 3.Verhaar J. Patient satisfaction after total knee replacement-still a challenge. Acta Orthop 2020;91:241-2. [Google Scholar | PubMed]
- 4.Bargar W. Robotic hip surgery and current development with the Robodoc system. In: Navigation and Robotics in Total Joint and Spine Surgery. Berlin, Heidelberg: Springer; 2004. p. 119-22. [Google Scholar | PubMed]
- 5.Singh V, Fiedler B, Simcox T, Aggarwal VK, Schwarzkopf R, Meftah M. Does the use of intraoperative technology yield superior patient outcomes following total knee arthroplasty? J Arthroplasty 2021;36:S227-32. [Google Scholar | PubMed]
- 6.Kort N, Stirling P, Pilot P, Müller JH. Robot-assisted knee arthroplasty improves component positioning and alignment, but results are inconclusive on whether it improves clinical scores or reduces complications and revisions: A systematic overview of meta-analyses. Knee Surg Sports Traumatol Arthrosc 2021;30:2639-53. [Google Scholar | PubMed]