The intent of this article is to demonstrate the following rare injury and its subsequent management by the orthopedic trauma team.
Dr. Guillermo Rodriguez, Resident Physician, Department of Orthopaedic Surgery and Sports Medicine, Detroit Medical Center, Detroit, MI, USA. 311 Mack Ave 5th Floor, Detroit, MI 48201, USA. E-mail: guillermo0390@gmail.com
Introduction: Surgical treatment of bilateral traumatic sternoclavicular (SC) joint dislocations has never been reported in the literature. In the acute setting, posterior dislocation can present with a host of comorbidities due to structures that lie in close proximity posterior to the medial clavicle.
Case Report: This study presents a case of bilateral traumatic posterior SC joint dislocation with associated brachiocephalic injury that was treated with open reduction and surgical stabilization.
Conclusion: This is a rare case of bilateral posterior sternoclavicular joint dislocation that underwent open surgical intervention. Treatment of this injury resulted in excellent radiographic and clinical outcomes at 2-year follow-up.
Keywords: Sternoclavicular joint, Fracture, Dislocation, Open Reduction
Traumatic sternoclavicular (SC) joint dislocations are uncommon, historically comprising about 3% of shoulder girdle injuries and accounting for only 1% of joint dislocations [1-3]. Bilateral traumatic SC joint dislocation is an exceedingly rare injury, with no existing reports of surgically treated cases in the literature [3,4]. Posterior SC joint dislocations have the potential for significant complications due to nearby vital structures; yet, there is a lack of surgeon experience in the management of this injury due to its low clinical occurrence. The purpose of this report is to review the very rare presentation of an injury and its corresponding imaging in the acute setting, as well as to discuss the surgical approach and technique chosen that ultimately led to an acceptable functional outcome for the patient. This patient was made aware that data concerning their case would be submitted for publication and the patient gave consent.
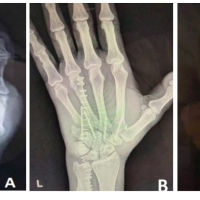
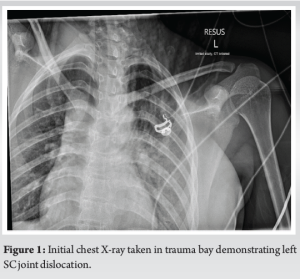
Patient is a 19-year-old female who arrived at the emergency department of a level one trauma center through ambulance as a “trauma code 2”. She was the restrained passenger in the back seat of a car that was rear-ended on the highway by a second car traveling at an unknown speed. The patient required extrication from the vehicle. In the emergency department, she was alert and oriented, had stable vital signs, and had a chief complaint of left shoulder pain, neck pain, and chest pain. On physical examination, she had tenderness over the left clavicle with mild swelling over the SC joint. Forward elevation of the left shoulder was limited to 45 degrees due to pain. She reported no discomfort to the right clavicle with a full range of motion of the right shoulder. Bilateral radial pulses were equal. There were no motor or sensory deficits noted in her bilateral upper extremities. Initial radiographs of the chest and right clavicle in the emergency department demonstrated an asymmetric appearance of the sternoclavicular joints and a possible mediastinal hematoma as demonstrated in Fig. 1. A thoracic computed tomography (CT) scan with intravenous contrast was subsequently obtained which revealed bilateral posterior SC joint dislocations. In addition, the CT scan demonstrated an indentation of the left brachiocephalic vein and a small hematoma in the upper mediastinum, as seen in Fig. 2. Cardiothoracic surgery was consulted which recommended observation due to low severity of vessel injury. The patient was deemed stable and transferred to the orthopedic floor before operative treatment of her injuries.

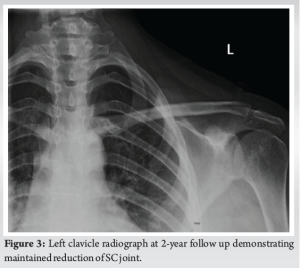
The next day, the patient was taken to the operating room. Once in the room, she was placed in a supine position on an Orthopedic Systems Inc. (OSI) table and anesthesia was induced successfully. Closed reduction under fluoroscopy was attempted on the left SC joint without success. An attempt at closed reduction was then performed without success on the right side. At this time, the decision was made to proceed with open reduction and surgical stabilization of her bilateral SC joint dislocation. An incision was made over the manubrium and clavicle over the SC joint. The border of the medial clavicle was exposed, and the sternocleidomastoid muscle (SCM) elevated off from its insertion. Exposure of the manubrium and SC joints was subsequently obtained. The SC joint was then successfully reduced using point to point reduction clamp while pulling traction on the ipsilateral arm. An intraosseous tunnel was then drilled through the medial clavicle. A slip of tendon from the medial SCM was cut in line with its fibers and oversewn with fiberloop tape. The slip of tendon was then passed through the previously drilled clavicular tunnel. An intraosseous tunnel was then drilled into the manubrium. The slip of tendon then passed through the intraosseous manubrium tunnel and sutured to itself using fiberloop tape. The reduction was then checked, remaining stable with stress testing. We then turned our attention to the right SC joint. Incision and exposure to the clavicle, SC joint, and manubrium were performed similarly to the contralateral side. Reduction of the joint was again obtained using towel clamps with traction being pulled on the ipsilateral arm. Holes were drilled in both the medial clavicle and manubrium. A slip of the medial SCM tendon was obtained and reinforced with fiberloop. The tendon was then passed through the clavicle, back through the manubrium, and sutured to itself with fiberloop. The joint was once again noted to be stable. Fluoroscopy was used to assess the quality of reduction. At this time, both SC joints were successfully reduced and stable on examination. The incision was irrigated and subsequently closed. Sterile dressings were applied, and the patient returned to the recovery area in stable condition. Postoperatively, the patient was instructed to be non-weight bearing in both her right and left upper extremities. Furthermore, her left upper extremity was placed in a sling for comfort. Follow-up clavicle radiographs taken at postoperative clinic visits demonstrated satisfactory healing of the clavicle and SC joint with no evidence of recurrent posterior dislocation bilaterally (Fig. 3). At 26-month postoperatively, the patient has 5/5 muscle strength to bilateral upper extremities without differences in the range of motion, and there were no motor or sensory abnormalities noted. She occasionally utilizes non-steroidal anti-inflammatories (NSAIDs) for pain relief and reports prominence and discomfort over the area of the left SC joint. She denies pain or symptoms on the right SC joint. A discussion was held with the patient regarding possible medial clavicle excision for comfort in the future.
SC joint dislocations are quite uncommon with fewer than 150 cases presented in the literature [1,2,5,6]. Posterior dislocations comprise about 12% of these injuries with the majority being dislocated anteriorly [7,8]. The patient presented in this study presented with bilateral posterior SC joint dislocations, which is an injury pattern that has not been reported in the literature. A dislocated SC joint can cause negative long-term results such as decreased function and post-traumatic arthritis [9,10]. Current recommendations suggest a closed reduction to be attempted for both anterior and posterior SC joint dislocations. However, they should be attempted within 72 h from injury and successful reduction is obtained in approximately 38% of cases [11]. If closed reduction fails, open reduction is recommended for posterior SC joint dislocation as clinical outcomes are significantly better. As closed reduction was unsuccessful in our patient, open-operative intervention was indicated. Interestingly, one report of bilateral SC joint dislocation involved a case where the right anteriorly dislocated joint was treated with closed reduction and the accompanying left posterior SC joint dislocation was discovered incidentally on CT imaging 6 months after injury. After lengthy discussions, the patient elected to continue with conservative treatment of the posterior SC dislocation [4]. In our patient, SC joint dislocations were evidenced by a thorough evaluation of CT imaging, ruling out possible physeal fractures and revealing a vascular injury. With regards to cardiothoracic involvement in cases of posterior SC dislocation, it is recommended for the cardiothoracic surgery team to remain available during open treatment of these cases due to the proximity to vital structures and high likelihood of vascular injury. Our patient was evaluated preoperatively by cardiothoracic surgery due to a vascular injury discovered on imaging upon admission. No intervention by cardiothoracic surgery was recommended at the time of injury. At the time of surgical intervention by the orthopedics team, cardiothoracic surgery was not present in the operating room; however, they were available throughout the procedure. Although historical guidelines do often recommend the presence of cardiothoracic surgery, one group recently reviewed 35 cases of open reduction of SC joint dislocation that has not required the cardiothoracic team in the operating room [3,9-12]. In younger patients, such as ours, there is a concern for posteriorly displaced fracture when evaluating a possible SC joint dislocation in considering that medial clavicular epiphysis is the last to close (ages 22–25). Some authors have referred to this injury as a pseudo-dislocation. It is important to make this distinction as the pathology is different; however, both presentations require prompt treatment, and the presentation is similar [8,13-15]. For example, the only previous report of bilateral SC joint dislocation in a young individual describes a bilateral traumatic posterior SC dislocation due to epiphyseal fracture where the terms are used interchangeably. Closed reduction was initially successful although the patient required open reduction and fixation a few days after the initial injury [16].
Posterior SC joint dislocations are extremely uncommon injuries and are associated with vascular injury. For the most favorable outcomes, unsuccessful closed reduction must be followed by open reduction and internal fixation to be completed within the first 72 h after injury. Bilateral SC dislocations were treated open in this case. There are multiple open approaches described in literature to treat this injury that is effective, and the chosen treatment is at the discretion of the surgeon. Further investigation is warranted to determine the most optimal operative protocol to address this rare injury.
This article describes the clinical experience of the authors and decision-making that resulted in the successful treatment of a bilateral posterior SC joint dislocation with open reduction internal fixation.
References
- 1.Cave ER, Burke JF, Boyd RJ. Trauma Management. Chicago, IL: Year Book Medical; 1974. p. 409-11. [Google Scholar | PubMed]
- 2.Cope R. Dislocations of the sternoclavicular joint. Skeletal Radiol 1993;22:233-8. [Google Scholar | PubMed]
- 3.Sernandez H, Riehl J. Sternoclavicular joint dislocation: A systematic review and meta-analysis. J Orthop Trauma 2019;33:e251-5. [Google Scholar | PubMed]
- 4.Albarrag MK. Bilateral asymmetrical traumatic sternoclavicular joint dislocations. Sultan Qaboos Univ Med J 2012;12:512-6. [Google Scholar | PubMed]
- 5.Rajaratnam S, Kerins M, Apthorp LJ. Posterior dislocation of the sternoclavicular joint: A case report and review of the clinical anatomy of the region. Clin Anat 2002;15:108-11. [Google Scholar | PubMed]
- 6.Kuzak N, Ishkanian A, Abu-Laban RB. Posterior sternoclavicular joint dislocation: Case report and discussion. CJEM 2006;8:355-7. [Google Scholar | PubMed]
- 7.Morell DJ, Thyagarajan DS. Sternoclavicular joint dislocation and its management: A review of the literature. World J Orthop 2006;7:244-50. [Google Scholar | PubMed]
- 8.Garg S, Alshameeri ZA, Wallace WA. Posterior sternoclavicular joint dislocation in a child: A case report with review of literature. J Shoulder Elbow Surg 2012;21:e11-6. [Google Scholar | PubMed]
- 9.Laffosse JM, Espié A, Bonnevialle N, Mansat P, Tricoire JL, Bonnevialle P, et al. Posterior dislocation of the sternoclavicular joint and epiphyseal disruption of the medial clavicle with posterior displacement in sports participants. J Bone Joint Surg Br 2010;92:103-9. [Google Scholar | PubMed]
- 10.Salgado RA, Ghysen D. Post-traumatic posterior sternoclavicular dislocation: Case report and review of the literature. Emerg Radiol 2002;9:323-5. [Google Scholar | PubMed]
- 11.Groh GI, Wirth MA, Rockwood CA Jr. Treatment of traumatic posterior sternoclavicular dislocations. J Shoulder Elbow Surg 2011;20:107-13. [Google Scholar | PubMed]
- 12.MacDonald PB, Lapointe P. Acromioclavicular and sternoclavicular joint injuries. Orthop Clin North Am 2008;39:535-45. [Google Scholar | PubMed]
- 13.Robinson CM, Jenkins PJ, Markham PE, Beggs I. Disorders of the sternoclavicular joint. J Bone Joint Surg Br 2008;90:685-96. [Google Scholar | PubMed]
- 14.Tornetta P 3rd, Ricci, W, McQueen, MM. Rockwood and Green’s Fractures in Adults. United States: Lippincott Williams and Wilkins; 2019. [Google Scholar | PubMed]
- 15.Carmichael KD, Longo A, Lick S, Swischuk L. Posterior sternoclavicular epiphyseal fracture-dislocation with delayed diagnosis. Skeletal Radiol 2006;35:608-12. [Google Scholar | PubMed]
- 16.Baumann M, Vogel T, Weise K, Muratore T, Trobisch P. Bilateral posterior sternoclavicular dislocation. Orthopedics 2010;33:510. [Google Scholar | PubMed]