This paper describes a minimally invasive approach for inserting magnetically controlled growing rods with robotic-assisted navigation in a pediatric patient with early-onset scoliosis.
Dr. Jessica H. Heyer, Department of Pediatric Orthopaedics, Hospital for Special Surgery, New York, United States of America. E-mail: heyerj@hss.edu
Introduction: Early-onset scoliosis (EOS) refers to spinal curvature exceeding ten degrees in the coronal plane in patients under 10 years old. When non-operative management fails to control the curvature, surgical intervention may be indicated. In younger patients, growth-friendly instrumentation may be necessary to allow for continued spinal growth while controlling the curve, which includes magnetically control growing rods (MCGR). This paper is the first description of robotic-assisted navigation in a patient with EOS undergoing MCGR insertion with the minimally invasive placement of pedicle screws. The benefits of a trans-muscular robotic-assisted technique include minimizing the risk of autofusion of the non-instrumented area.
Case Report: The 7-year-old female patient with vertebral, anal, cardiac, tracheoesophageal, renal, esophageal, and limb anomalies and a complex medical history, presented with progressive, early-onset syndromic scoliosis. She underwent various surgeries in infancy for imperforate anus, colonic atresia, and malrotation, among other issues. Over time her curve worsened, reaching 71° by age seven. Insertion of MCGR was recommended and successfully performed using robotic-assisted navigation for placement of pedicle screws. Immediately post-operatively, the patients’ major curve improved to 15°. She was discharged home without complications on post-operative day 4.
Conclusion: This case study exemplifies the success and safety of growth-friendly instrumentation using robotic-assisted navigation for the placement of pedicle screws.
Keywords: Magnetically controlled growing rods, early-onset scoliosis, robotic-assisted navigation.
Early onset scoliosis (EOS) is defined as coronal-plane spinal deformity >10° diagnosed in children under 10 years old [1]. Initial treatment often involves non-operative intervention such as casting or bracing. However, if these interventions do not slow curve progression, surgery may be necessary. The primary aim of surgery in patients with EOS is to improve curve magnitude while maintaining chest and spinal growth, so as to allow further development of the lungs. These procedures, which include traditional growing rods (TGRs), magnetically controlled growing rods (MCGRs), vertical expandable prosthetic titanium ribs, and the Shilla technique are deemed “growth friendly” techniques [2-4]. A well-described phenomenon seen with both TGR and MCGR is the law of diminishing returns, which is defined as smaller amounts of growth with subsequent lengthening [5,6]. This is thought to be due to progressive stiffening or autofusion of the portion of the spine that is spanned by the instrumentation. As such, growth-friendly constructs are limited in that they can only provide so much growth once they are implanted. This underscores the importance of making this surgery as minimally invasive as possible, so as to not disturb the periosteum, joints, and soft tissues, which can lead to this autofusion. Robotic-assisted navigation may facilitate less invasive surgery that avoids dissection of the paraspinal muscles off the midline, as well as allowing for trans-muscular minimally invasive pedicle screw placement, facetectomy, and fusion [7,8]. This is the first description of robotic-assisted navigation in the placement of growing rods in a pediatric patient with EOS. This paper describes the technique utilized at the authors’ institution for MCGR insertion using a minimally invasive approach with robotic-assisted navigation.
Preoperatively, the patient undergoes a computed tomography (CT) scan, localized to the areas of intended pedicle screw instrumentation. Anesthesia is rarely utilized for the CT scan due to its brevity but is used when necessary. The CT is uploaded to the robotic-navigation software and three plans are made at each level: (1) The pedicle screw (Fig. 1a), (2) burr trajectories for bony preparation of the screw insertion site (Fig. 1b), and (3) burr trajectories for the facetectomies, planning to remove the inferior articular process and the cartilage of the superior articular process (Fig. 1c). It is important to plan the bony preparation burr trajectories (2) in line with the pedicle screw trajectory (1) to allow for them both to be performed through the same trans-muscular pathway. Consideration should also be made to have the burr trajectories for the facetectomies (3) not be too convergent, as this may lead to a need for percutaneous/additional incisions instead of going through the initial incision. Of note, these trajectories can be adjusted intraoperatively to improve the insertion position of the tools.

The patient is positioned in the prone position on a standard radiolucent spine table. After prepping and draping, the proximal and distal anchor sites are localized using fluoroscopic imaging. A standard midline incision is made at the proximal and distal anchor sites, with dissection carried down to the level of the deep fascia. Skin and subcutaneous tissue are undermined to allow improved retraction for trans-muscular access. The tips of two adjacent spinous processes are exposed and a robotic clamp is attached to the spinous process, and the robot is attached to the clamp (Fig. 2).
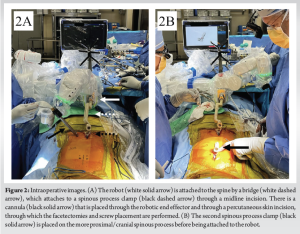
A two-shot fluoroscopy registration is performed for the pre-operative CT scan with the intraoperative position of the patient. At each level, the following sequence is performed: (1) the robotic arm is sent to the bony preparation burr trajectory, (2) a large knife is placed through the end-effector through the muscle and down to the bone, (3) a cannula with a navigated dilator is placed down to the bone, (4) the large navigated acorn-tip burr (7.5 × 10 mm) is placed through the end-effector and burrs down the bone that may impede accurate pedicle screw placement (i.e. minimize skive potential), (5) the robotic arm is sent to the pedicle screw trajectory, (6) a high-speed (3.0 × 30 mm) navigated burr/drill is placed through the end-effector into the pedicle, (7) a ball-tip probe is placed in the drill hole to confirm intrapedicular position, and then (8) a screw is placed through the end effector using a navigated screwdriver. After all, screws are placed, motor evoked potentials are obtained. Attention is then turned to the facetectomies. The end effector is sent to the facetectomy trajectory, followed by the placement of the large knife through the end effector down to the bone, a cannula is placed down to the bone using a navigated dilator, followed by the use of the acorn-tip burr in the pre-planned trajectory for the facetectomy through the cannula. Allograft bone graft mixed with vancomycin powder is then placed down the cannula and packed into the facetectomy. After the proximal levels are completed, the same process is carried out at the intended distal anchor sites. Following screw placement, MCGR are contoured and inserted submuscularly. Provisional fixation is performed distally with set screws, and the rods are reduced into the proximal screws bilaterally. Distraction is performed across the concavity of the deformity followed by provisional set screw tightening. Fluoroscopic images are obtained to confirm the appropriate positioning of pedicle screws and deformity correction. All incisions are then irrigated, the allograft is placed into the transmuscular incisions and then closed in a standard fashion.
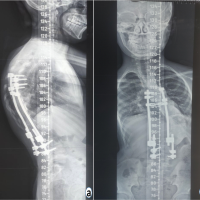
The patient is a 7-year-old female with vertebral, anal, cardiac, tracheoesophageal, renal, esophageal, and limb anomalies syndrome, and a complex medical history, who presented with progressive syndromic scoliosis. She was born through spontaneous vaginal delivery at 40 weeks gestation and was diagnosed at birth with imperforate anus, colonic atresia, and malrotation, requiring immediate ileocecectomy and ileostomy, followed by Ladd’s procedure at age two. Relevant medical history includes low cortisol levels, ventriculomegaly, cranial and ocular anomalies, and a leg length discrepancy of 3 cm (right > left). The patient demonstrated delayed gross motor skills, beginning walking at the age of 3 years. However, she did not develop cognitive delay and has been attending age-appropriate school as of October 2023. Her adrenal insufficiency resolved spontaneously. The patient was diagnosed with syndromic scoliosis of the thoracolumbar spine at 11 months old based on clinical examination and plain radiographs; magnetic resonance imaging demonstrated no intraspinal abnormalities. At age three, a Thoracolumbar Sacral Orthosis (TLSO) brace (Boston Orthotics and Prosthetics) was recommended for her 36° curve, with a minimum of 18 h of wear per day recommended. She had difficulty wearing her brace due to her colostomy and stopped wearing her brace consistently at age four, at which point she was lost to follow-up until age six. By 6 years old, her curve increased to 51°. She was recommended again for a new TLSO brace but did not wear it. By age 7, the curve had progressed to 71° and the insertion of growing rods was recommended as surgical treatment (Fig. 3).
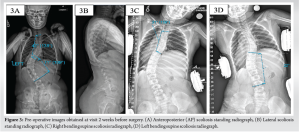
The patient underwent posterior spinal fusion of T3-T4 and L3-L4 with MCGR placement using the above surgical technique with robotic-assisted navigation. The procedure was tolerated well with no complications. On immediate prone post-operative radiographs, her major curve improved from 71° to 21°. Her first-erect radiograph before discharge demonstrated the major curve decreasing from 71 to 15° (Fig. 4). Her post-operative course was uncomplicated and she was discharged home on post-operative day 4, with pain controlled on acetaminophen and ibuprofen. Her first lengthening was performed in the office at 3-month postoperatively, which she tolerated well. She planned for lengthening at 3-month intervals.

Growing rods are often utilized in the treatment of EOS due to their ability to correct scoliotic curves while allowing growth of the spine. Furthermore, patients with idiopathic scoliosis have been identified to have asymmetrical intervertebral deformities in multiple planes, with varying pedicle widths on the concave and convex sides of the curve [9-16]. The three-dimensional asymmetry of pedicles can increase the challenges of pedicle screw insertion in small and/or dysplastic pedicles, as well as placing vital structures such as the spinal cord and aorta at risk [9,15,16]. Robotic-assisted navigation has been shown to facilitate more accurate and precise pedicle screw insertion both in vivo and in cadaver models [17-22]. We present a novel technique for minimally invasive pedicle screw placement in the setting of growing rods that minimizes exposure and allows for trans-muscular pedicle screw placement and facetectomies. The utilization of robotic navigation facilitates less invasive and accurate pedicle screw insertion as well as less invasive facetectomy.
Our example case illustrates the success of this procedure with minimal acute post-operative complications. We recommend utilizing robotic navigation to decrease the invasiveness of the procedure while allowing for highly accurate placement of pedicle screws.
Robotic-assisted navigation can be used for the safe placement of pedicle screws in EOS.
References
- 1.Ponseti IV, Friedman B. Prognosis in idiopathic scoliosis. J Bone Joint Surg Am 1950;32A:381-95. [Google Scholar | PubMed]
- 2.Akbarnia BA, Pawelek JB, Cheung KM, Demirkiran G, Elsebaie H, Emans JB, et al. Traditional growing rods versus magnetically controlled growing rods for the surgical treatment of early-onset scoliosis: A case-matched 2-year study. Spine Deform 2014;2:493-7. [Google Scholar | PubMed]
- 3.Lebon J, Batailler C, Wargny M, Choufani E, Violas P, Fron D, et al. Magnetically controlled growing rod in early onset scoliosis: A 30-case multicenter study. Eur Spine J 2017;26:1567-76. [Google Scholar | PubMed]
- 4.Skaggs DL, Choi PD, Rice C, Emans J, Song KM, Smith JT, et al. Efficacy of intraoperative neurologic monitoring in surgery involving a vertical expandable prosthetic titanium rib for early-onset spinal deformity. J Bone Joint Surg Am 2009;91:1657-63. [Google Scholar | PubMed]
- 5.Sankar WN, Skaggs DL, Yazici M, Johnston CE 2nd, Shah SA, Javidan P, et al. Lengthening of dual growing rods and the law of diminishing returns. Spine (Phila Pa 1976) 2011;36:806-9. [Google Scholar | PubMed]
- 6.Heyer JH, Anari JB, Baldwin KD, Mitchell SL, Luhmann SJ, Sturm PF, et al. Lengthening behavior of magnetically controlled growing rods in early-onset scoliosis: A multicenter study. J Bone Joint Surg Am 2022;104:2186-94. [Google Scholar | PubMed]
- 7.Zawar A, Chhabra HS, Mundra A, Sharma S, Kalidindi KK. Robotics and navigation in spine surgery: A narrative review. J Orthop 2023;44:36-46. [Google Scholar | PubMed]
- 8.Zhang Q, Han XG, Xu YF, Fan MX, Zhao JW, Liu YJ, et al. Robotic navigation during spine surgery. Expert Rev Med Devices 2020;17:27-32. [Google Scholar | PubMed]
- 9.Liljenqvist UR, Allkemper T, Hackenberg L, Link TM, Steinbeck J, Halm HF. Analysis of vertebral morphology in idiopathic scoliosis with use of magnetic resonance imaging and multiplanar reconstruction. J Bone Joint Surg Am 2002;84:359-68. [Google Scholar | PubMed]
- 10.Liljenqvist UR, Link TM, Halm HF. Morphometric analysis of thoracic and lumbar vertebrae in idiopathic scoliosis. Spine (Phila Pa 1976) 2000;25:1247-53. [Google Scholar | PubMed]
- 11.Smith RM, Pool RD, Butt WP, Dickson RA. The transverse plane deformity of structural scoliosis. Spine (Phila Pa 1976) 1991;16:1126-9. [Google Scholar | PubMed]
- 12.Xiong B, Sevastik B, Willers U, Sevastik J, Hedlund R. Structural vertebral changes in the horizontal plane in idiopathic scoliosis and the long-term corrective effect of spine instrumentation. Eur Spine J 1995;4:11-4. [Google Scholar | PubMed]
- 13.Upendra B, Meena D, Kandwal P, Ahmed A, Chowdhury B, Jayaswal A. Pedicle morphometry in patients with adolescent idiopathic scoliosis. Indian J Orthop 2010;44:169-76. [Google Scholar | PubMed]
- 14.Vaccaro AR, Rizzolo SJ, Allardyce TJ, Ramsey M, Salvo J, Balderston RA, et al. Placement of pedicle screws in the thoracic spine. Part I: Morphometric analysis of the thoracic vertebrae. J Bone Joint Surg Am 1995;77:1193-9. [Google Scholar | PubMed]
- 15.Vaccaro AR, Rizzolo SJ, Balderston RA, Allardyce TJ, Garfin SR, Dolinskas C, et al. Placement of pedicle screws in the thoracic spine. Part II: An anatomical and radiographic assessment. J Bone Joint Surg Am 1995;77:1200-6. [Google Scholar | PubMed]
- 16.Davis CM, Grant CA, Pearcy MJ, Askin GN, Labrom RD, Izatt MT, et al. Is there asymmetry between the concave and convex pedicles in adolescent idiopathic scoliosis? A CT investigation. Clin Orthop Relat Res 2017;475:884-93. [Google Scholar | PubMed]
- 17.Vardiman AB, Wallace DJ, Booher GA, Toossi N, Bucklen BS. Decreasing the pedicle screw misplacement rate in the thoracic spine with robot-guided navigation. Clin Spine Surg 2023;36:431-7. [Google Scholar | PubMed]
- 18.McCormick B, Asdourian PL, Johnson DC, Moatz BW, Duvall GT, Soda MT, et al. 100 Complex posterior spinal fusion cases performed with robotic instrumentation. J Robot Surg 2023;17:2749-56. [Google Scholar | PubMed]
- 19.Volk VL, Steele KA, Cinello-Smith M, Chua RV, Pollina J, Poulter G, et al. Pedicle screw placement accuracy in robot-assisted spinal fusion in a multicenter study. Ann Biomed Eng 2023;51:2518-27. [Google Scholar | PubMed]
- 20.Vaccaro AR, Harris JA, Hussain MM, Wadhwa R, Chang VW, Schroerlucke SR, et al. Assessment of surgical procedural time, pedicle screw accuracy, and clinician radiation exposure of a novel robotic navigation system compared with conventional open and percutaneous freehand techniques: A cadaveric investigation. Global Spine J 2020;10:814-25. [Google Scholar | PubMed]
- 21.Jiang B, Pennington Z, Zhu A, Matsoukas S, Ahmed AK, Ehresman J, et al. Three-dimensional assessment of robot-assisted pedicle screw placement accuracy and instrumentation reliability based on a preplanned trajectory. J Neurosurg Spine 2020;33:519-28. [Google Scholar | PubMed]
- 22.Oppermann M, Karapetyan V, Gupta S, Ramjist J, Oppermann P, Yang VX. The pedicle screw accuracy using a robotic system and measured by a novel three-dimensional method. J Orthop Surg Res 2023;18:706. [Google Scholar | PubMed]