This case report highlights the importance of considering lower cervical root compression as a potential cause of cervicogenic headache which can be improved with surgical intervention.
Dr. Jephtah F L Tobing, Faculty of Medicine, Universitas Pelita Harapan, Tangerang, Indonesia/Departement of Orthopaedics and Traumatology, Siloam Hospitals Lippo Village, Tangerang, Indonesia. E-mail: jephtah.tobing@uph.edu
Introduction: Commonly, cervicogenic headache (CGH) pathology originates from the upper cervical nerve ranging from C1–C3, with C2–C3 most frequently involved. The pathophysiology and etiology of this syndrome have been the subject of ongoing controversy in the past decade. Most literature regarding CGH, mainly research about relationship between upper cranial nerves (C1–C3) indicating that the possibility it originates from other cervical levels is poorly understood.
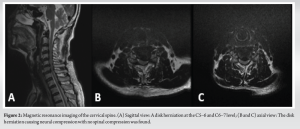
Case Report: A 64-year-old man arrived with a 6-month history of occiput pain, followed by severe shooting pain in both arms, with a greater intensity on the right side. A cervical spine magnetic resonance imaging reveals disk herniations at the C5–6 and C6–C7 levels, producing neural compression. The operation involved an anterior cervical discectomy and fusion. Six months of follow-up revealed that the patient was headache-free; ultimately, the diagnosis was CGH caused by a herniated lower cervical disk.
Conclusion: Through reporting this unusual case, we emphasized the potential correlation between lower cervical disk herniation and CGH.
Keywords: Cervicogenic headache, lower cervical segment herniation, anterior discectomy and fusion.
Cervicogenic headache (CGH) is recognized for causing a unilateral, non-throbbing headache. This pain is believed to be referred from the cranium in either osseous structures or soft tissues located in the cervical region [1-3]. This condition is first postulated by Sjaastad in 1983 and frequently observed as a chronic and recurring headache, typically exacerbated by movements of the neck, and often accompanied by a diminished neck range of motion (ROM) [1]. It is frequently mistaken for a migraine, tension-type headache (TTH), and cluster headache [4]. CGH has been identified in studies as manifesting with various severities from moderate-to-severe in cranium and orbita regions except parietal [2]. The occurrence rate of CGH within the population varies between 1% and 4.1%, while it may escalate to as much as 17.5% among individuals experiencing severe headaches [5]. The pathological mechanism of CGH is hypothesized to originate from the upper cervical C1–C3 spinal nerves [1-3,6]. Hence, it is plausible that any anatomical arrangement innervated by the spinal nerves C1–C3 could potentially serve as the etiology for a CGH [1,7,8]. Most cases of CGH are commonly associated with the C2–3 zygapophyseal joint, accounting for around 70% of cases [6]. It remains uncommon for abnormality of these structures, particularly prolapse of the lower cervical disk, to induce CGH [7]. One study by Diener et al., revealed that CGH due to lower cervical disk prolapse that was treated with surgery, was shown to improve with 11 out of 12 patients reported either being headache-free or dramatic improvement in their headache [9]. In this case report, we present an atypical case of chronic persistent occipital headache with bilateral arm discomfort resulting from a lower cervical disk prolapse (C5–C6 and C6–C7) that was successfully treated surgically [10].
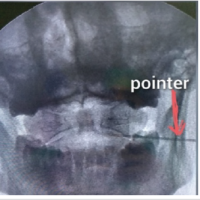
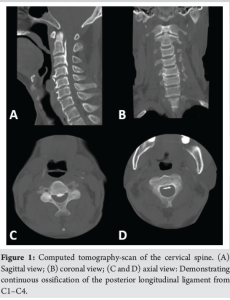
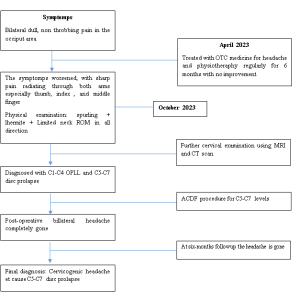
The patient, a 64-year-old man, granted written authorization for the dissemination of the data included in this report. He presented with a 6-month history of persistent, aching pain at the occiput. The headache is localized and described as a dull, constant discomfort. The patient also reported a sharp shooting pain in both arms, with a stronger intensity on the right side. The pain radiates from his neck and shoulders down to the finger, predominantly affecting the thumb, index, and middle fingers. His symptoms have been progressively worsening over the past 6 months, significantly impacting his daily activities, including sleeping and performing simple task. The patient had taken oral non-steroidal anti-inflammatory drug for his headache and doing some physiotherapy for long time but none worked. The patient has a history of hypertension, which is well-controlled with medication. He does not possess any documented medical records indicating the presence of musculoskeletal or neurological diseases in their past. The family history does not contribute to the current condition. On physical examination, the patient demonstrated limited neck mobility, with discomfort experienced during flexion, extension, and rotation. Neurological examination revealed no motor deficits or sensory abnormalities in both extremities. The Spurling test was positive, indicating cervical radiculopathy. The Lhermitte sign was also positive. Deep tendon reflexes, including the Hoffman sign, were negative. Sensory and motor function of the cervical plexus was excellent, with no deficits observed. Numerous diagnostic investigations have been conducted on the patient. A CT scan of the cervical spine confirms the presence of ossification of the posterior longitudinal ligament (OPLL) at the C1–4 levels, classified as K-line positive, as shown in Fig. 1. An magnetic resonance imaging (MRI) of the cervical spine was also done to confirm disk herniations at the C5–6 and C6–C7 levels causing neural compression but without evident spinal cord compression (Fig. 2.), with electromyography findings consistent with bilateral radiculopathy at C5 and C7, further confirming the nerve root involvement.
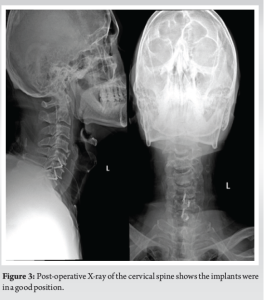
The patient was diagnosed with concurrent OPLL at C1–C4 and cervical disk herniations at C5–6 and C6–7, then underwent anterior cervical discectomy and fusion (ACDF) surgery at C5–6 and C6–7 levels. There were no complications encountered intraoperatively. Post-operative cervical radiograph was done; implants were in a good position (Fig. 3). One day after the procedure, the patient reported that his headache was almost completely gone with pain level of visual analog scale (VAS) 1–2. The patient was discharged 2 days following the surgery without any post-operative complication postoperatively. At the 6 months follow-up, the patient was headache free, the final diagnosis made was CGH due to lower cervical disk herniation.
Timeline
Significant advancements have been achieved since the initial identification of CGH cases [1]. Particularly in the past decade, there has been substantial progress in the characterization of the clinical presentation, establishment of diagnostic criteria, and development of therapeutic strategies [2,11,12]. As per definition, CGH is considered a syndrome which is “final universal pathway” for pain stemming from several neck disorders. These may involve such structures as nerves, nerve root ganglia, uncovertebral joints, intervertebral disks, facet joints, ligaments, and muscle [1,13]. Latest diagnostic guide for CGH was established by the International Classification of Headache Disorder 3rd edition that comprised several points, as shown on Table 1.

Our patient had disk herniations at the C5–6 and C6–7 levels, as well as OPLL at the C1–4 levels, as observed on the cervical spine MRI. This was accompanied by pain in the occipital region and restricted neck mobility. Following ACDF procedure, the pain in the occipital region resolved immediately, thus fulfilling criteria for CGH. The potential mechanism behind CGH has been proposed to involve the role of the spinal nucleus of the fifth cranial nerve. Trigeminocervical nucleus is a region of the upper cervical spinal cord where sensory nerve fibers in the descending tract of the trigeminal nerve are believed to interact with sensory fibers from the upper cervical roots. The nociceptive nucleus of the head and neck, known as the trigeminocervical nucleus, receives pain signals from the C1–C3 nerves. The aforementioned association is believed to be the underlying factor contributing to the occurrence of referred pain in the occipital region and/or the eyes. The pain experienced in a CGH is believed to be exacerbated by aseptic inflammation and neurotransmission occurring inside the C-fibers, which is attributed to cervical disk pathology [6]. In accordance with the hypothesis of CGH, the surgeon would prioritize resolving the issue in the upper cervical area in this particular patient, since no precise anatomical characteristics have been identified. In this present case, it was seen that concurrent occurrences of a cervical disk herniation at the C5–6 and C6–7 levels, as well as an upper cervical disorder such as OPLL at the C1–4 level, were identified. OPLL often manifests as myelopathy and is frequently associated with reported alterations in balance and dexterity, such as deteriorating handwriting and challenges in buttoning garments [7]. No indications of myelopathy or radiculopathy were seen in the upper cervical area of this patient; however, radiculopathy was present from the lower cervical region. Our primary attention lies in addressing the issue pertaining to the lower cervical region. To the best of our knowledge, there have been no recorded cases of this particular instance linking this specific trait to the occurrence of CGH. Several studies have documented CGH induced by disk herniation below the level of spinal nucleus of trigeminal nerve or lower cervical problems [9,14]. Precise mechanism underlying the relationship between lower cervical spine diseases and their impact on the trigeminocervical nucleus is not yet fully understood, as there is presently no proven neuroanatomical link between afferent pathways originating from the middle-lower cervical region and the trigeminocervical nucleus. Shimohata et al. have put out hypotheses suggesting that some nociceptive input may go across the ipsilateral spinocervicothalamic tract [3]. In addition, it is plausible that there is communication between the spinocervicothalamic tract and trigeminal spinal complex through anastomosis. An alternative theory is the presence of excessive increases in ROM of the upper cervical spine as a compensatory response to kinesthetic impairment in the lower cervical spine. This compensatory action may lead to overstimulation of the trigeminocervical nucleus, ultimately generating a CGH. The utilization of manipulative therapy and therapeutic exercise routine is widely recognized as the primary treatment approach for effectively managing CGHs [15]. According to a study by Jull and Richardson, 72% of patients had achieved a reduction of 50% or more in headache frequency at the 12-month follow-up. However, it may initially worsen the headache. Interventional therapy presents an alternative approach for managing CGHs, with the specific treatment modality varying based on the underlying cause. Examples of such interventions include occipital nerve block, epidural steroid injection, and radiofrequency ablation. Previous study by Park et al., found that the utilization of radiofrequency neurotomy on the medial branches of the lower cervical (C4–7) region resulted in reduction of VAS at 6 months which is statistically significant. Through retrospective study, Deiner et al., found that only one in 12 patients underwent disk prolapse removal surgery reported no difference in headache. Surgical intervention is typically reserved as a final recourse [10]. In this case, the patient has suffered a headache for 6 months and have tried pharmacological and physiotherapy but none worked. Weighing the current status of the patient, we proceeded with an ACDF procedure. Following the procedure and at 6-months follow-up, the patient was headache free.
This case study reported that, in patient with lower cervical root compression, CGH might arise which can be improved by surgical removal of the underlying disease. In addition, further research regarding association of lower cervical and cervicogenic is encouraged.
CGH can be caused by a herniated lower cervical disk. We highlighted the probable correlation between lower cervical disk herniation and CGH by presenting this rare case.
References
- 1.Sjaastad O, Saunte C, Hovdahl H, Breivik H, Grønbâk E. “Cervicogenic” headache. An hypothesis. Cephalalgia 1983;3:249-56. [Google Scholar | PubMed]
- 2.Berk T, Ashina S, Martin V, Newman L, Vij B. Diagnosis and treatment of primary headache disorders in older adults. J Am Geriatr Soc 2018;66:2408-16. [Google Scholar | PubMed]
- 3.Sjaastad O, Fredriksen TA, Pfaffenrath V. Cervicogenic headache: Diagnostic criteria. Headache 1998;38:442-5. [Google Scholar | PubMed]
- 4.Sjaastad O, Bakketeig LS. Prevalence of cervicogenic headache: Vågå study of headache epidemiology. Acta Neurol Scand 2008;117:173-80. [Google Scholar | PubMed]
- 5.Bogduk N. The anatomy and pathophysiology of neck pain. Phys Med Rehabil Clin N Am 2011;22:367-82. [Google Scholar | PubMed]
- 6.Silverberg ND, Martin P, Panenka WJ. Headache trigger sensitivity and avoidance after mild traumatic brain injury. J Neurotrauma 2019;36:1544-50. [Google Scholar | PubMed]
- 7.Al Khalili Y, Ly N, Murphy PB. Cervicogenic headache. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507862 [Last accessed 2022). [Google Scholar | PubMed]
- 8.Diener HC, Kaminski M, Stappert G, Stolke D, Schoch B. Lower cervical disc prolapse may cause cervicogenic headache: Prospective study in patients undergoing surgery. Cephalalgia 2007;27:1050-4. [Google Scholar | PubMed]
- 9.Zhou L, Hud-Shakoor Z, Hennessey C, Ashkenazi A. Upper cervical facet joint and spinal rami blocks for the treatment of cervicogenic headache. Headache 2010;50:657-63. [Google Scholar | PubMed]
- 10.Headache Classification Committee of the International Headache Society (IHS). The International Classification of headache disorders, 3rd edition (beta version). Cephalalgia 2013;33:629-808. [Google Scholar | PubMed]
- 11.Sheng P. Headache Classification Subcommittee of the International Headache Society. The International Classification of headache disorders: 2nd edition. Cephalalgia 2004;24 Suppl (1):9-160. [Google Scholar | PubMed]
- 12.Sjaastad O, Salvesen R, Jansen J, Fredriksen TA. Cervicogenic headache a critical view on pathogenesis. Funct Neurol 1998;13:71-4. [Google Scholar | PubMed]
- 13.Gondo G, Watanabe T, Kawada J, Tanaka M, Yamamoto K, Tanaka S, et al. A case of cervicogenic headache caused by C5 nerve root derived shwannoma: Case report. Cephalalgia 2017;37:902-5. [Google Scholar | PubMed]
- 14.Shimohata K, Hasegawa K, Onodera O, Nishizawa M, Shimohata T. The clinical features, risk factors, and surgical treatment of cervicogenic headache in patients with cervical spine disorders requiring surgery. Headache 2017;57:1109-17. [Google Scholar | PubMed]
- 15.Jull G, Trott PP, Potter H, Zito G, Shirley D, Emberson J, et al. A randomized controlled trial of exercise and manipulative therapy for cervicogenic headache. Spine (Phila Pa 1976) 2002;27:1835-43. [Google Scholar | PubMed]