The use of both modifications, Ilizarov and Catagni, to pelvic support osteotomy is a good therapeutic option for late-diagnosed patients with sequelae of developmental dysplasia of the hip.
Dr. María de la Luz Arenas-Sordo, Department of Genetics, National Institute of Rehabilitation “Luis Guillermo Ibarra Ibarra” Av México-Xochimilco 289. Arenal de Guadalupe, Tlalpan, México City. E-mail: mlarenassordo@hotmail.com; mlarenassordo@gmail.com
Introduction: The management of hip dislocation in patients older than 9 years of age is a challenge in terms of deciding which is the best treatment course to follow since the main sequelae are as follows: pain, discrepancy in the length of the pelvic extremities and lame gait, with the consequent disability for activities of daily living. In Ho Choi, Thabet A mention limited treatment options, including total hip arthroplasty and hip arthrodesis. These options have their benefits and limitations. The pelvic support osteotomy initially indicated for the treatment of septic arthritis of the hip and performed for the first time by Bavoier in 1838 and modified in 1970 by Ilizarov aims to improve the aforementioned sequelae. These cases report showed us the functional improvement with the treatment of dislocated hip dysplasia with pelvic support osteotomy with monolateral fixator and the 2nd osteotomy 4 cm distal to the hip. This was corroborated through the application of the modified Harris test.
Case report: A series of six female Mexican adolescent patients from 11 to 17 years of age who come to the clinic due to long-standing pain symptoms in the coxofemoral joint, three patients in the right and three in the left hip when walking. All were treated with pelvic support osteotomy. The six patients continued with mild positive Trendelenburg but all of them diminished the discrepancy in the pelvic extremities, the mobility arcs were preserved and pain was suppressed in all. The modified Harris test showed increased scores (103.3%) after the surgery. There was just a minor complication in a patient, and it was resolved with surgical lavage.
Conclusion: The modifications in the technique, monolateral fixator and second osteotomy 4 cm from the first one, allowed our patients to present functional improvement at the hip, which was assessed with the modified Harris scale. Patients achieved independent walking without pain and Trendelenburg less evident. The changes we found in our patients are evidence of the goodness and effectiveness of this type of osteotomy in patients older than 9 years of age, to improve the function of the hip.
Keywords: Pelvic support osteotomy, Hip instability, Hip dislocation, external fixator.
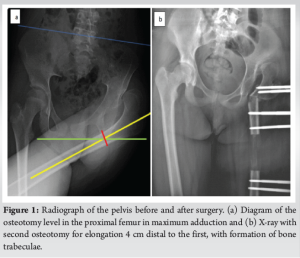
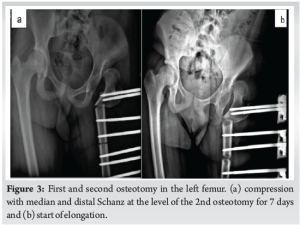
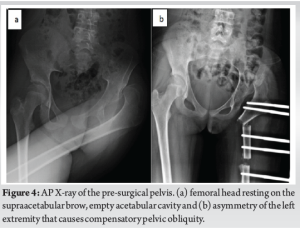
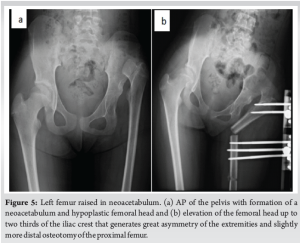
The management of hip dislocation in patients older than 9 years of age is a challenge in terms of deciding which is the best treatment to follow since the main sequelae are as follows: pain, discrepancy in the length of the pelvic extremities and limping gait, with the consequent disability for activities of daily living. In the current literature, limited treatment options are mentioned, including total hip arthroplasty (TCA) and hip arthrodesis [1,2]. The pelvic support osteotomy (PSO) has benefits and limitations [3]. It was performed for the first time by Bavoier [4] in 1838 and modified in 1970 by Ilizarov [1] aims to diminish a good number of the described sequelae in these patients, providing stability and a better arm lever to the hip, preserving the mobility arcs, pain reduction, and correcting the discrepancy of the pelvic extremities. In all cases, we perform a Schanz osteotomy which is performed by drawing a horizontal line at the level of the ischial tuberosity with the proximal femur in maximum adduction [2-6]. The modification to the Ilizarov technique was performed by Catagni and consists of performing the second osteotomy 4 cm distal to the first. This allowed correction of the distal femoral valgus and mechanical axis of the limb posterior to the first osteotomy. The second usual osteotomy is the one performed at the level of the CORA (angulation center of rotation) [5-7]. The procedure for this modification to the Ilizarov technique is, in addition to the second osteotomy 4 cm from the first in the femur, the use of a monolateral fixation system (Catagni, 1994) [7], with a ruler consisting of a rail and three straight heads, achieving proper alignment of the mechanical axis. Lengthening is performed through the second osteotomy site with ¼ turn starting on the 7th day. In accordance with the principles established by Ilizarov, excessive lengthening should be avoided as it is poorly tolerated in a hip that is already fully adducted [1,5]. The objective of this cases report is to show that pelvic support osteotomy with the Ilizarov and Catagni modifications are a good therapeutic option for patients older than 9 years of age with late diagnosis with sequelae of developmental hip dysplasia.
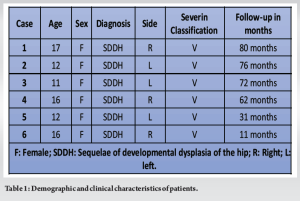
We study and carry out a surgical treatment in six Mexican adolescent patients between the ages of 11 and 17, who attended the clinic due to long-term pain in the coxofemoral joint, three in the right hip and three in the left when walking. All of them were in Severin’s V classification and were followed between 11 and 80 months (Table 1).
Case 1
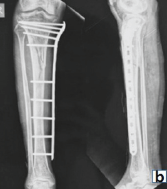
A 17-year-old female presented with the right hip pain. Background: Open reduction, acetabuloplasty and varoderotator osteotomy of the right hip, adductor myotomy, transcondylar traction at 4 years of age, without follow-up. Current physical examination: positive Trendelenburg, pain, claudication, ranges of motion: 90° flexion; extension 0°; internal rotation 20°; external rotation 35°; abduction 20°; 35° adduction, and Severin V. OSP was performed at 17 years of age with the described technique (Fig. 1). Start stretching on the 7th day with a ¼ turn every 6 h and periodic controls. At 3 months, a bone marrow aspirate from the left tibia is placed at the elongation site to promote new callus formation. Time with the fixative was 14 months, the modified Harris scale increased from 58 to 73 points (25.8%). Positive Trendelenburg, but less obvious when walking. With 80 months of follow-up, currently undergoing rehabilitation therapy, she does not report hip pain (Fig. 2).

Case 2
A 12-year-old woman presented with the left hip pain and lower extremity asymmetry. Background: Gait with claudication at one year of age. She consulted a doctor at 2 years of age who diagnosed her with dysplasia of the left hip. The family decided not to allow the proposed surgical treatment to be performed at that time. She started with pain at 12 years old. Physical examination: positive Trendelenburg, gait with claudication, left hip pain, range of motion: 70° flexion, 0° extension, 30° abduction, 25° adduction, 30° internal rotation, 15° external rotation, and Severin type V. The PSO was performed at 12 years of age with the previously described technique. Time with fixative 10 months. During follow-up, she presented valgus at the level of 18° in the left knee and pain in the medial compartment of the knee, for which a varus osteotomy was performed in the left femur with external fixation (Fig. 3). The modified Harris scale had an increase from 39 to 69 points (76.9%), during 76 months of follow-up, she did not present hip pain.
Case 3
A 11-year-old woman presented with the left hip pain. Background: The use of a Pavlik harness at 1 month of age. At 3 years of age, an open reduction of the dislocated left hip was performed, without subsequent check-ups. Physical examination: Positive Trendelenburg, limp gait, with ranges of motion: flexion 100°, extension 0°, abduction 25°, adduction 25°, internal rotation 20°, external rotation 30°, and Severin type V. OSP is performed at 11 years old, adductor revision, and psoas myotomy. Time with fixative 11 months, after fixative withdrawal consolidation, the modified Harris scale showed an increase from 37 to 76 points (48.8%). At present, at 72 months of follow-up, she presented slightly positive Trendelenburg and no pain in the operated hip (Fig. 4).
Case 4
A 13-year-old female presented with the right hip pain. Background: Unspecified surgery at 18 months of age without follow-up by parents. At 12 years of age, she started with pain and a limping gait for no apparent reason. Physical examination: Right hip pain, faltering gait, positive Trendelenburg, range of motion: 70° flexion, 0° extension, 30° abduction, 25° adduction, 30° internal rotation, 15° external rotation, and Severin type V (Fig. 5). The OSP surgery was carried out at 16 years of age. The use of fixative for 10 months. The modified Harris scale had an increase from 13 to 72 points (453%). At present, with 62 months of follow-up, there was less evident of Trendelenburg gait, and she mentioned that she did not have pain.
Case 5
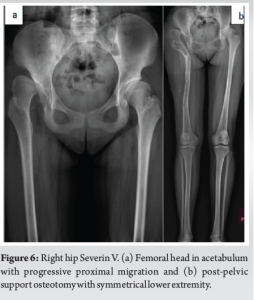
A 12-year-old female presented with pain and functional limitation of the left hip. Background: The use of insoles with elevation in the left pelvic limb, without specification at what age. Physical examination: Positive Trendelenburg, lower extremity asymmetry, and range of motion flexion 120°, extension 0°, internal rotation 10, external rotation 30°, abduction 40°, adduction 35°, and Severin type V. OSP surgery was performed at 12 years of age of age, bone marrow aspirate was placed at the elongation site at 8 months, fixative was withdrawn at 11 months (Fig. 6). The modified Harris scale showed increase from 48 to 73 points (52%). At present, with 31-month follow-up, independent walking without pain.
Case 6
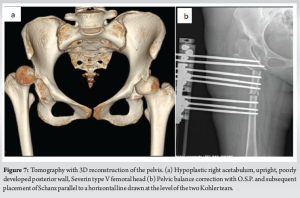
A 16-year-old female presented with the right hip pain. Background: Bilateral hip dysplasia at birth without follow-up until 11 years of age that she began with pain in the right hip, treated at that time with adductor myotomy, no follow-up (Fig. 7). Physical examination: Limp gait, lower extremity asymmetry, positive Trendelenburg, right hip pain, range of motion: 90° flexion, 0° extension, 30° abduction, 20° adduction, 20° internal rotation, 30° external rotation, and Severin V. OSP was performed at 16 years of age, after a month of follow-up, she presented volume increase and erythema at the level of the proximal Schanz, controlled with weekly dressings and oral antibiotic. At 3 months, she presented suture dehiscence and seropurulent exudate, surgical debridement was performed, continued elongation and antibiotic treatment. At present, with 11 months of follow-up, the modified Harris scale presented an increase from 17 to 68 points (300%). Fixative withdrawal is scheduled.
In all cases, we carried out the pelvic support osteotomy with the Ilizarov and Catagni modifications. The Schanz osteotomy is performed by drawing a horizontal line at the level of the ischial tuberosity with the proximal femur in maximum adduction [2,6]. The second osteotomy was at 4 cm distal to the first. This allowed correction of the distal femoral valgo; in addition to the second osteotomy, it is the use of a monolateral fixation system (Catagni 1994) [7], with a ruler consisting of a rail and three straight heads, achieving proper alignment of the mechanical axis. Lengthening is performed through the second osteotomy site with ¼ turn starting on the 7th day.
Modified Harris functional scale
We carried out the modified Harris scale, previously used by Paley for hips with severe sequelae of septic arthritis in children, to have an objective result from the goodness of the surgical technique. The modified Harris scale includes pain assessment; function of the distance walked; support function; mobility and muscle power; ability to enter and exit from vehicle; foot care, for example: washing and drying feet; claudication; and to have difficult or not to climb stairs. This scale has the following score to classify the function of the hip: 70 to 80 points = excellent, 60 to 69 points = good, 50 to 59 points = fair, and 49 points or less = poor. This scale assessed the patients before and after the pelvic support osteotomy surgery[8].
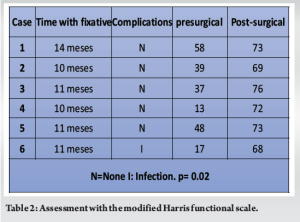
OSP is indicated in children older than 9 years as it was originally recommended for the treatment of septic arthritis by Bavoier and Bombelli [4,5], our patients were all older than 9 years, the mean age was 13.8 (SD 2.4) years, (range 11–17 years). The mean follow-up of 55.3 months is almost equal to the mean of 52.5 months reported in other studies [4]. The mean time to external fixation was 11 months versus 7 months (range 5.2–9.5 months) reported by other authors [4,9], having a minimal difference compared to our study. According to what was cited by most of the articles, in our series of cases, an osteotomy was performed in the proximal femur at the ischium level, keeping the limb in maximum adduction, to correct the muscular stability of the hip; however, the second osteotomy that was performed 4 cm distal to the initial one followed the Catagni principle [7,9] which allowed us to maintain the anatomy of the proximal femur, correcting the mechanical axis. Other authors insist on performing the second osteotomy at the CORA site to avoid valgus deformities [5]; however, we consider that the Catagni modification is better because it minimally modifies the proximal anatomy of the femur, which would facilitate future surgery if necessary does not invade the periphery of the knee joint to a great extent, does not restrict muscle function of the quadriceps femoris, and allows movement of the knee joint during treatment in addition to the use of a less cumbersome external fixator. Regarding functionality, in our series, we observed a significant difference between the pre-surgical and final follow-up means going from 35.3 (SD 17.4) to 71.8 (SD 2.9) equivalent to 103.3% improvement in the test of Harris (Z of Wilcoxon 2.2, p = 0.02), as it happened with the patients reported by Pieter and Muhammad et al. [4,10] (Table 2).
Several studies have confirmed the beneficial effects of OSP, both clinical and imaging studies and gait analysis, since it improves functionality, which has been attributed to the increase in hip abductor muscle mass after OSP that is documented with magnetic resonance studies [2].
The main adverse effect is the anatomical alteration of the proximal femur after OSP, both in the sagittal and frontal planes, which would significantly increase the difficulty of a possible future total hip replacement (THR). However, Thabet et al. [2] reported a successful THR 15 years after OSP and concluded that the altered anatomy of the proximal femur after OSP did not preclude subsequent THR. However, even with current surgical techniques and prosthetic designs, total hip replacement in young patients remains controversial [2,6]. The six patients in this study presented severe positive Trendelenburg (T) before surgery, which decreased considerably after surgical treatment, being less evident during walking (Fig. 8). The literature shows that an average of 30.3% (range 0–62.5%) of patients remains with a positive T sign after OPS, but with a decrease in severity in most cases [4,10,11]. This persistence may be due to abductor insufficiency related to atrophied abductor muscles before surgery, or loss of fulcrum during follow-up due to remodeling of the valgus angulation of the proximal femur, which is consistent with the results obtained in our study [1].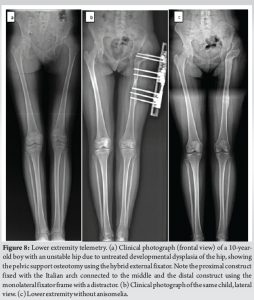
The only complication that occurred in our cases was infection at the entrance of the Schanz nails in one case, which was treated with surgical cleaning and antibiotics, as was also reported by Emara et al. [4,5,12], in a study conducted in 37 patients.
Based on the results and their comparison with other studies, we can conclude that pelvic support osteotomy with the Catagni modifications is a good option in patients older than 9 years of age with an initial diagnosis of hip dysplasia sequelae, since it allows reduce pain symptoms, preserve knee range of motion, and independent gait with less obvious Trendelenburg. The functional improvement they presented was objective through the assessment with the modified Harris scale, presenting an improvement of 103.3% in our case report.
Hip dysplasia that is frequently not treated early and, therefore, important sequelae develop, the main one being pain, as well as a significant difference in length that causes lameness. We consider that the combination of the Ilizarov and Catagni techniques to pelvic support osteotomy provides a very good answer. In this series of cases, we present our experience in six patients, all of them had a good evolution, especially because pain was eliminated and the difference in length of the two extremities was reduced, which allowed a more adequate gait.
References
- 1.Pontes DS, Bortolin PH, Batista J. Double femoral osteotomy for the treatment of severe sequelae of the immature hip. Acta Ortop Bras 2020;28:287-90. [Google Scholar | PubMed]
- 2.Thabet A, Catagni M, Guerreschi F. Total hip replacement fifteen years after pelvic support osteotomy (PSO): A case report and review of the literature. Musculoskelet Surg 2012;96:141-7. [Google Scholar | PubMed]
- 3.El-Mowafi H. Outcome of pelvic support osteotomy with the Ilizarov method in the treatment of the unstable hip joint. Acta Orthop Belg 2005;71:686-91. [Google Scholar | PubMed]
- 4.Inan M, Bowen R. A pelvic support osteotomy and femoral lengthening with monolateral fixator. Clin Orthop Relat Res 2005;440:192-8. [Google Scholar | PubMed]
- 5.Kocaoglu M, Eralp L, Sen C, Dinçyürek H. The Ilizarov hip reconstruction osteotomy for hip dislocation: Outcome after 4-7 years in 14 young patient. Acta Orthop Scand 2002;73:432-8. [Google Scholar | PubMed]
- 6.Pafilas D, Nayagam S. The pelvic support osteotomy: Indications and preoperative planning. Strat Traum Limb Recon 2008;3:83-92. [Google Scholar | PubMed]
- 7.Mahran MA, ElGebeily MA, Ghaly NA, Thakeb MF, Hefny HM. Pelvic support osteotomy by Ilizarov’s concept: Is it a valuable option in managing neglected hip problems in adolescents and young adults? Strat Traum Limb Recon 2011;6:13-20. [Google Scholar | PubMed]
- 8.Mahomed NN, Arndt DC, McGrory BJ, Harris WH. The Harris hip score: Comparison of patient self-report with surgeon assessment. J Arthroplasty 2001;16:575-80. [Google Scholar | PubMed]
- 9.Masquijo JJ, Miscione H, Goyeneche R, Primomo C. Pelvic support osteotomy and distal femoral lengthening with monolateral external fixator. Rev Asoc Argent Ortop Traumatol 2008;73:391-9. [Google Scholar | PubMed]
- 10.Reynders Frederix P, Reynders Frederix C, Wajid M. Pelvic support osteotomy; Salvage procedure in chronically dislocated hips case report: Technical note on the on-lay bone positioning of a lengthening nail and review of the literature. Open Orthop J 2016;10:232-40. [Google Scholar | PubMed]
- 11.Mandar A, Tong X, Song S, Park Y, Hong JH, Lee H, et al. Pelvic support osteotomy for unstable hips using hybrid external fixator: Case series and review of literature. J Orthop Sci 2012;17:9-17. [Google Scholar | PubMed]
- 12.Umer M, Rashid H, Umer HM, Raza H. Hip reconstruction osteotomy by Ilizarov method as a salvage option for abnormal hip joints. Biomed Res Int 2014;2014:835681. [Google Scholar | PubMed]