Interposition arthroplasty provides a viable treatment option for post-traumatic elbow stiffness in young patients with heavy demands in whom total elbow arthroplasty and elbow fusion would fail to provide satisfactory outcomes
Dr. Swastik Nakade, Department of Orthopaedics, Gleneagles Hospital, Parel-400012, Mumbai, India. E-mail: swastik1901@gmail.com
Introduction: Post-traumatic arthritis of elbow is a crippling condition that frequently develops after a serious joint injury. The condition is characterized by pain, rigidity, and diminished functionality, considerably affecting the quality of life of those impacted. Despite advancements in surgical and conservative management, the optimal treatment strategy remains elusive.
Case Report: A 31-year-old male presented to us with post-traumatic elbow arthritis with loss of function affecting his activities of daily living, 2 years post a road traffic accident. Radiographs showed a malunited right proximal humerus fracture with arthritic right elbow joints with implants present in situ. As he was a young person with high functional demands, we decided to take him up for elbow interposition arthroplasty. Fascia lata graft was taken and interposed between the prepared ends of the distal humerus and proximal ulna. Interoperative range of 20–120 degree was possible. One year post-surgery after undergoing rehabilitation therapy, the patient had good clinical function with elbow range of motion between 15 and 110° of flexion.
Conclusion: Interposition elbow arthroplasty provides satisfactory functional results in young patients with post-traumatic elbow arthritis.
Keywords: Post-traumatic elbow stiffness, elbow arthritis, fascia lata autograft, interposition arthroplasty.
Post-traumatic arthritis of the elbow is a crippling condition that frequently develops after a serious joint injury. The condition is characterized by pain, rigidity, and diminished functionality, considerably affecting the quality of life of those impacted. The first traumatic injury starts a chain reaction of inflammatory reactions and cartilage degradation that makes up the pathogenesis [1]. Despite advancements in surgical and conservative management, the optimal treatment strategy remains elusive. Inaccurate reduction combined with articular cartilage incongruity may eventually lead to secondary osteoarthritis accompanied by discomfort and functional disruption [2]. In the early stages of treating post-traumatic elbow arthritis, non-operative measures such as intra-articular corticosteroid injections, non-steroidal anti-inflammatory drugs, and elbow wraps are still the standard. Patients who have elbow pain and a considerable loss of mobility, which impairs upper extremity function and limits everyday activities, may consider surgical intervention. Due to the increased demands placed on the implant over the course of a patient’s lifetime, total elbow arthroplasty (TEA), while a good first-line treatment for older and low-demand patient populations, should only be considered a salvage option for young, active patients. These demands might result from a failure or refusal to follow the activity restrictions stipulated with TEA, which would otherwise result in high rates of mechanical failure. Therefore, the objectives of surgery for this patient population are to preserve future salvage alternatives while providing a minimally painful and functional elbow articulation. Interposition arthroplasty provides a satisfactory surgical alternative in the young population [3]. We present a case of a 31-year-old male who presented to us with post-traumatic elbow arthritis with loss of function affecting his activities of daily living and was subsequently taken up for interposition arthroplasty.
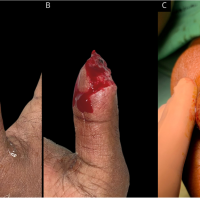
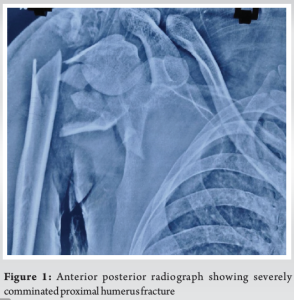
A 31-year-old male visited our outpatient department with complaints of right elbow pain on movement and restricted movements affecting his activities of daily living. He gave a history of road traffic accident 2 years before in which he had sustained a right-sided severely comminated proximal humerus fracture (Fig. 1) and right-side compound ulna proximal third shaft fracture with olecranon comminated fracture (Fig. 2). He underwent open reduction and fixation for proximal humerus (Fig. 3), olecranon and ulna fracture. 12 months post-surgery the proximal humerus implants were removed and the fracture was malunited (Fig. 4).
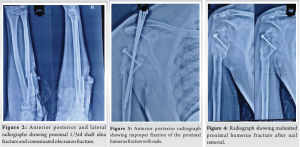
On presenting to us his range of motion in the elbow was restricted to 70–80° of elbow flexion and forearm fixed in mid pronation. He had restricted shoulder movements but his main concern was restricted movement of the right elbow affecting his activities of daily living. His radiographs showed post-traumatic arthritic changes in the right elbow with implants in situ (Fig. 5). Looking at his functional demands we decide to take him up for interposition arthroplasty of the right elbow once he was medically cleared for surgery.

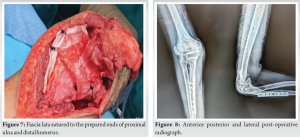
The surgery was done in a lateral decubitus position with a posterior approach to the elbow. Ulnar nerve was exposed and freed. Mediolateral subperiosteal dissection was done followed by a triceps turn-down flap (Fig. 6). Olecranon fossa was burr holed and the radial head was excised. Anterior bony hinge broken was broken and bony ankylosis freed posteroanterior. Intraoperative elbow range of motion of 20–120° was possible. Fascia lata graft was taken, interposed in between curetted articular ends of the distal humerus and proximal ulna and sutured to the ends (Fig. 7). Final range of movement on operating table of 20–120° was achieved with free pronation and supination. Thorough wash was given and closure done in layers. He was uneventful postoperatively. On 2 weeks follow up, suture removal was done, and was given hinged elbow brace. After significant post-operative rehabilitative physiotherapy, he had a good functional and radiographic (Fig. 8) outcome at 1 year follow-up. Elbow range of motion was 15–110° of flexion with terminal 5° restriction of pronation and supination.
Managing elbow arthropathy in younger patients presents a unique set of challenges. It might be difficult to make up for the functional loss caused by elbow pain and stiffness, which can be incapacitating. Surgical treatment is based on finding a long-lasting remedy that does not interfere with an active lifestyle in cases when non-operative management fails. Options include interposition arthroplasty, release of contractures, fusion surgeries, debridement and contracture release with the help of arthroscopy and prosthetic replacement [4]. Interposition arthroplasty, which initially originated from the idea of the addition of a local tissue or skin to prevent painful contact between the ends of the resection, was historically a variation on simple resection arthroplasty of a joint. The idea was creating a biological membrane over an arthritic joint surface that might otherwise be considered for prosthetic replacement [4]. Both post-traumatic and inflammatory arthritis respond well to interposition arthroplasty. Gross deformity or instability, presence of active infection, open physis and the loss of flexor motor function are among the contraindications for this procedure. In addition, elbow pain at rest and insufficient elbow bone stock are linked to less-than-ideal results [5,6]. An alternative to TEA for young, in-demand patients is interposition arthroplasty, which resurfaces the elbow articulating surface using autograft (such as fascia lata, cutis) or allograft (such as Achilles tendon, dermis) [3]. In particular, because interposition does not impose the weight-bearing and post-operative use restrictions advised following TEA, its proponents view it as a feasible treatment choice for this population. Furthermore, and maybe more importantly, there are other alternatives for reconstruction following interposition arthroplasty, such as TEA or another interposition arthroplasty [7,8]. It is recommended to obtain traditional X-rays with contralateral films. Key features available on conventional imaging are the degree of angular deformity, quantification of joint narrowing, heterotopic ossification if present and its location, the quality of the articular surface, instability of the joint, and location of bone loss. When a complex deformity is present and a reliable measurement of the rotational, sagittal, or coronal deformity is needed, computed tomography (CT)/3D CT may be helpful in some circumstances [4]. Celli and Morrey in between 1982 and 2003 performed 133 interposition arthroplasties at the Mayo clinic out of which 71% were performed for post-traumatic elbow stiffness [9]. Cheng and Morrey treated 13 patients with mobile arthritic elbows between 1986 and 1994 with distraction interposition arthroplasty using fascia lata. Eight patients (62%) achieved an outstanding or good result based on the objective criteria of the Mayo Elbow Performance score, while nine patients (69%) experienced satisfactory pain reduction [6]. Nolla et al. in their retrospective case series of 13 patients who underwent interposition arthroplasty with temporary external fixator application had their mean flexion arc improved from 48° to 110° postoperatively [10]. Larson and Morrey treated 69 elbows with interposition arthroplasty using Achilles tendon allograft. Postoperatively the mean flexion arc improved from 51 to 97°. After surgery, the mean Mayo score increased from 41 to 65 points. Seven patients required a revision, whereas thirteen patients had exceptional or excellent results, fourteen had fair results, and eleven had poor results. The authors concluded that interposition elbow arthroplasty may be beneficial for young, active patients with severe arthritis who have reduced elbow motion but no associated elbow instability, despite the operation’s status as a salvage procedure that neither fully restores function nor eliminates pain [5]. Even though the literature reports rather low results, one of the most appealing aspects of interposition arthroplasty is that it does not interfere with further salvage treatments. Larson et al. in his study on revision interposition arthroplasties of the elbow revised nine patients of a failed interposition arthroplasty with another interposition arthroplasty using Achilles tendon allograft. Five patients felt satisfied after the revision while one patient reported a poor result [8]. Blaine et al. in his study revised a failed interposition arthroplasty by converting it to a TEA. Out of the 12 revisions that he carried out, 10 patients reported a satisfactory outcome with mild or no pain at mean 9.9 years of post-operative follow-up [7].
Interposition arthroplasty provides a satisfactory functional outcome in young patients suffering from post-traumatic elbow arthritis. In young patients in whom functional demands are high, TEA is not a good option due to significant post-operative restrictions. Interposition arthroplasty also offers a chance of salvage even in cases of failure in the form of revision interposition arthroplasty and TEA.
Post-traumatic arthritis causes significant disability and restriction in activities of daily living. Interposition arthroplasty provides a good surgical alternative once conservative treatment fails in young patients of elbow arthritis.
References
- 1.Gallo RA, Payatakes A, Sotereanos DG. Surgical options for the arthritic elbow. J Hand Surg 2008;33:746-59. [Google Scholar | PubMed]
- 2.Wysocki RW, Cohen MS. Primary osteoarthritis and posttraumatic arthritis of the elbow. Hand Clin 2011;27:131-7, v. [Google Scholar | PubMed]
- 3.Sears BW, Puskas GJ, Morrey ME, Sanchez-Sotelo J, Morrey BF. Posttraumatic elbow arthritis in the young adult: Evaluation and management. J Am Acad Orthop Surg 2012;20:704-14. [Google Scholar | PubMed]
- 4.Morrey M, Dutta A, Whitney I, Morrey B. Interposition arthroplasty: Current indications, technique and expectations. J Clin Orthop Trauma 2021;19:175-82. [Google Scholar | PubMed]
- 5.Larson AN, Morrey BF. Interposition arthroplasty with an Achilles tendon allograft as a salvage procedure for the elbow. J Bone Joint Surg Am 2008;90:2714-23. [Google Scholar | PubMed]
- 6.Cheng SL, Morrey BF. Treatment of the mobile, painful arthritic elbow by distraction interposition arthroplasty. J Bone Joint Surg Br 2000;82:233-8. [Google Scholar | PubMed]
- 7.Blaine TA, Adams R, Morrey BF. Total elbow arthroplasty after interposition arthroplasty for elbow arthritis. J Bone Joint Surg Am 2005;87:286-92. [Google Scholar | PubMed]
- 8.Larson AN, Adams RA, Morrey BF. Revision interposition arthroplasty of the elbow. J Bone Joint Surg Br 2010;92:1273-7. [Google Scholar | PubMed]
- 9.Celli A, Morrey BF. Total elbow arthroplasty in patients forty years of age or less. J Bone Joint Surg Am 2009;91:1414-8. [Google Scholar | PubMed]
- 10.Nolla J, Ring D, Lozano-JB. Calderon S, Jupiter interposition arthroplasty of the elbow with hinged external fixation for post-traumatic arthritis. J Shoulder Elbow Surg 2008;17:459-64. [Google Scholar | PubMed]