Primary tuberculosis of a rib is a very uncommon presentation of musculoskeletal TB that clinicians must be aware for proper diagnosis and timely treatment.
Dr. Mantu Jain, Department of Orthopedics, AIIMS, Bhubaneswar, Odisha, India. E-mail: montu_jn@yahoo.com
Introduction: Primary tuberculosis (TB) of a rib is a very uncommon presentation and accounts for <1% of musculoskeletal TB.
Case Report: This case report studies a 34-year-old immunocompetent individual who presented with dull-aching right-side lower chest wall pain and swelling with constitutional symptoms. A routine X-ray of the chest was performed, which revealed no abnormality. Therefore, magnetic resonance imaging was performed given soft-tissue swelling, which suggested an extra-pulmonary swelling with lytic 9th rib lesion TB. The diagnosis was confirmed using a gene-expert of ultrasound-guided aspirated material. A drug susceptibility test was done, and it was found to be rifampicin sensitive. Hence, the patient was started on anti-tubercular therapy. The patient responded to it remarkably and was symptom-free at the end of 1 year.
Conclusion: The case illustrates that a high degree of suspicion, early diagnosis, and timely intervention are the key to management.
Keywords: Tuberculosis, ribs, antitubercular therapy.
India is the tuberculosis (TB) capital of the world, and therefore, the disease is a considerable public health problem [1]. Several reasons are attributable to this: Dense population, extensive immigration, and malnutrition in the lower socioeconomic class [2]. Osteoarticular TB (OATB) is a 15% burden of all forms of extra-pulmonary TB (EPTB) [3]. Primary TB of a rib is a very uncommon presentation and accounts for <1% of OATB [4]. TB of rib is seen in both immunocompetent and immunocompromised individuals [5]. As its diagnosis is difficult, especially in its early stages, a high index of suspicion is mandatory, along with imaging and other relevant studies to differentiate it from other diagnoses. Hence, we report an uncommon case of TB of the rib in an immunocompetent individual, its presentation, diagnosis, and treatment.
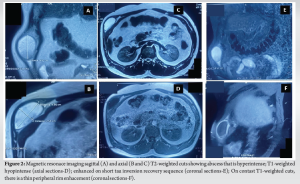
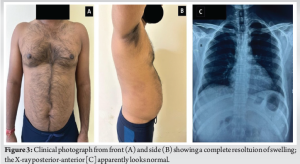
A 34-year-old male laborer by profession (belonging to lower socioeconomic status) presented with chief complaints of dull-aching pain associated with a swelling over the right-side lower chest wall, low-grade evening fever, and unintentional weight loss for 2 months. He denied any other joint pain or any history of trauma. His past history was insignificant, though his father had pulmonary TB 20 years back, for which he had taken anti-tubercular therapy (ATT) and was relieved. Upon physical examination, there was no lymphadenopathy or abnormality in the spine or other joints. However, there was tender swelling of 5 × 3 cm over the lateral side of the right lower chest wall, which was soft, non-compressible, and did not trigger a cough impulse (Fig. 1a and b). His complete blood count was within normal limits, but the erythrocyte sedimentation rate (ESR) was 90 mm/h, and C-reactive protein was reactive. Liver and renal function tests were normal, and he was negative for HIV. Radiological investigations such as X-ray chest were normal (Fig. 1c and d). A magnetic resonance imaging (MRI) was ordered given soft-tissue swelling, which showed a lytic lesion in the right 9th rib with a superficial cold abscess that was peripherally enhancing with thin walls. The spine, lung, and pleura were normal (Fig. 2a, b, c, d, e, f). An ultrasound (USG)-guided aspiration was done and was sent for routine microscopy, culture sensitivity, and geneXpert. The results showed positivity for Mycobacterium tuberculosis, which was rifampicin sensitive.

The patient was advised 1 year of ATT as per index TB guidelines for OATB. He started to show improvement. By 2 weeks, his fever had subsided, and his appetite improved; he gradually regained weight. The pain disappeared, and the cold abscess diminished in size progressively and disappeared within 3 months without sinuses, scars, or the need for surgery. The patient was then followed up regularly and was symptom-free at 12 months on completion of ATT. (Fig. 3).
OATB is the most common form of EPTB, accounting for 10–15% of all the TB burden in developing countries, unlike the Western world, where it accounts for only 1–2% of cases [3]. Among OATB, the vertebral column encompasses 50%, followed by the hip (15%) and the knees (5%). However, the involvement of ribs in TB is relatively infrequent. TB localization in the thoracic cage is rare [6,7]. Among the 980 patients suffering from OATB, 19 (2%) had lesions in the ribs and 14 (1.5%) in the sternum [8]. Nearly one-third of these patients had detectable TB lesions in other parts of the skeleton or the lungs [8]. TB is also considered the second most common cause of rib destruction after metastasis. TB rib usually forms a contagious spread from nearby pleuro-pulmonary foci or sometimes hematogenous from a distant focus [7]. About 50% of patients with rib TB have associated pulmonary presentation, but this was not seen in our patients [9]. TB destroys bone, producing caseous necrosis by granulation tissue, which may be pathognomonic [7]. The cold abscess can track along the chest wall to form a visible swelling and further can progress to form a sinus tract. However, overall, the symptoms are slow, indicated by local pain, unexplained low-grade fever, and reduced range of movement, especially if extensive involvement of the thoracic cage can herald even systemic complications. This makes the diagnosis delayed, complex, and dependent on radiological and microbiological/pathological investigations. Positive X-ray findings appear much later than usual clinical presentation, like swelling (due to cold abscess) and sinuses. The involved rib may show expansion with punched-out erosions, sometimes thickening, and rarely, there may be sequestrum formation [9,10]. Possible differentials of a lytic lesion in the rib are primary malignancy, TB (second most common), primary and secondary bone tumors, multiple myeloma, lymphoma, granulomatous diseases such as sarcoidosis, eosinophilic granulomas, and infections with fungi or amoeba [11-13]. In our patient, the contact history, socioeconomic status, constitutional symptoms, presence of a cold abscess, very high ESR, and positive geneXpert favored TB. M. tuberculosis geneXpert test has become an invariable and speedy tool if the biopsy is unsuccessful or unavailable [14]. In most cases, X-rays are normal in the early stages of the disease, as in our patients. Therefore, a high degree of suspicion is warranted. Computed tomography is sensitive and enables diagnosis and management planning [15]. Further MRI is helpful in soft-tissue extension. The classical TB cold abscesses had low-attenuated centers with a rim-enhancing periphery. Newer tests for the diagnosis of EPTB are also applicable to rib TB, which include the T-SPOT™ (Oxford Immunotec, Abingdon, Oxford, UK) TB test, a T cell-based assay, and a quantitative polymerase chain reaction of formalin-fixed paraffin-embedded skeletal specimens, and 18-fluorodeoxyglucose positron emission tomography imaging [16-18]. An MRI was done given soft-tissue swelling in our patient, and it was diagnosed as rib tubercular cold abscess. It was confirmed by aspiration and treated. USG-guided aspiration can be a valuable technique for diagnosing and starting ATT [15]. TB rib is essentially a medicinal disease. Singh et al. and similarly Nakiyingi et al. reported case of rib TB involving who had excellent response to medical therapy similar to our patient [5,7]. There was a need for more clarity regarding the duration of treatment, but recent recommendations from the index TB guidelines clarify that treatment for all forms of OATB should be one full year [19,20]. Surgical treatment may be rarely justified for doubtful diagnosis, a non-responsive case, or removal of large sequestrum, as in our patient [10,12,20].
Isolated TB rib is rare. Hence, early diagnosis and ATT will improve outcomes and prevent complications and recurrences. This case report suggests that TB is to be considered a differential even for atypical skeletal presentations. As TB rib cases are so few, randomized studies are impossible. Hence, we report this case as it can be applied to a more extensive study and will help better manage this rare condition of a common disease.
Isolated TB rib is rare and therefore it requires a high degree of suspicion, timely diagnosis after ruling out differentials and proper medical treatment with occasional surgical intervention.
References
- 1.Ministry of Health and Family Welfare. India TB Report. New Delhi; 2022. Available from: https://tbcindia.gov.in/writereaddata/indiatbreport2022/tbannaulreport2022.pdf. last assessed 10th Jan 2025. [Google Scholar | PubMed]
- 2.Gaude GS, Reyas A. Tuberculosis of the chest wall without pulmonary involvement. Lung India 2008;25:135-7. [Google Scholar | PubMed]
- 3.Shah BA, Splain S. Multifocal osteoarticular tuberculosis. Orthopedics 2005;28:329-32. [Google Scholar | PubMed]
- 4.Ghanta PR, Phatak SV, Parihar PS, Dhande RP, Reddy NG. Radiological evaluation of a rare case of rib caries and cold abscess in a young male patient with miliary tuberculosis: A case report with review of literature. Cureus 2023;15:e35075. [Google Scholar | PubMed]
- 5.Nakiyingi L, Bwanika JM, Lukande R, Kirenga B, Mwambu TP, Worodria W, et al. Destructive rib lesions in an HIV sero-negative male: An unusual presentation of tuberculosis in a high tuberculosis prevalence setting. Trop Doct 2012;42:217-8. [Google Scholar | PubMed]
- 6.Khan SA, Varshney MK, Hasan AS, Kumar A, Trikha V. Tuberculosis of the sternum: A clinical study. J Bone Joint Surg Br 2007;89:817-20. [Google Scholar | PubMed]
- 7.Singh SK, Gupta V, Ahmad Z, Bhargava R, Pandey DK, Sachdeva S. Tubercular osteomyelitis of rib-case report. Respir Med CME 2009;2:128-9. [Google Scholar | PubMed]
- 8.Tuli S, Sinha G. Skeletal tuberculosis-unusual lesions. Indian J Orthop 1969;3:5-18. [Google Scholar | PubMed]
- 9.Morris BS, Maheshwari M, Chalwa A. Chest wall tuberculosis: A review of CT appearances. Br J Radiol 2004;77:449-57. [Google Scholar | PubMed]
- 10.Chang JH, Kim SK, Lee WY. Diagnostic issues in tuberculosis of the ribs with a review of 12 surgically proven cases. Respirology 1999;4:249-53. [Google Scholar | PubMed]
- 11.Ozol D, Köktener A, Uyar ME. Active pulmonary tuberculosis with vertebra and rib involvement: Case report. South Med J 2006;99:171-3. [Google Scholar | PubMed]
- 12.Rajkumar V. Isolated tuberculosis of the ribs in an immunocompetent adult. Infect Dis (Auckl) 2022;1:39. [Google Scholar | PubMed]
- 13.Tang M, Huang J, Zeng W, Huang Y, Lei Y, Qiu Y, et al. Retrospective analysis of 10 cases of disseminated nontuberculous mycobacterial disease with osteolytic lesions. Infect Drug Resist 2021;14:4667-79. [Google Scholar | PubMed]
- 14.Mohanty M, Mishra B, Jain M, Karaniveed Puthiyapura L. Diagnostic role of Xpert-MTB RIF assay in osteoarticular tuberculosis: A retrospective study. World J Orthop 2022;13:289-96. [Google Scholar | PubMed]
- 15.Grover SB, Jain M, Dumeer S, Sirari N, Bansal M, Badgujar D. Chest wall tuberculosis-a clinical and imaging experience. Indian J Radiol Imaging 2011;21:28-33. [Google Scholar | PubMed]
- 16.Lee YM, Park KH, Kim SM, Park SJ, Lee SO, Choi SH, et al. Risk factors for false-negative results of T-SPOT.TB and tuberculin skin test in extrapulmonary tuberculosis. Infection 2013;41:1089-95. [Google Scholar | PubMed]
- 17.He G, Chen CY, Zhang X, Ding PP, Hu CZ, Huang XF, et al. Clinical performance of quantitative PCR for the molecular identification of skeletal tuberculosis from formalin-fixed paraffin-embedded tissues. BMC Infect Dis 2022;22:651. [Google Scholar | PubMed]
- 18.Cho YS, Chung DR, Lee EJ, Kim BT, Lee KH. 18F-FDG PET/CT in a Case of Multifocal Skeletal Tuberculosis without Pulmonary Disease and Potential Role for Monitoring Treatment Response. Clin Nucl Med 2014;39:980-3. [Google Scholar | PubMed]
- 19.Central TB Divison, Ministry of Health and Family Welfare G of I. Index TB Guidelines. Guidelines for Extrapulomary TB in India; 2016. Available from: https://tbcindia.gov.in/writereaddata/l892s/5585665076index-tb guidelines.pdf. last assessed 10th Jan 2025. [Google Scholar | PubMed]
- 20.Kabiri EH, Alassane EA, Kamdem MK, Bhairis M, Amraoui M, El Oueriachi F, et al. Tuberculous cold abscess of the chest wall: A clinical and surgical experience. Report of 16 cases(Case series). Ann Med Surg (Lond) 2020;51:54-8. [Google Scholar | PubMed]











