Melorheostosis presents a variety of clinical symptoms and imaging findings. Orthopedic surgeons should know the existence of this rare and unique condition
Dr. Keiichi Muramatsu, Department of Orthopedic Surgery, Nagato General Hospital, 85 Higashi-fukawa, Nagato, Yamaguchi 759-4194, Japan. E-mail: kemuramatsu@outlook.jp
Introduction: Melorheostosis was first described in 1922 with a pattern of linear hyperostosis described as a “dripping candle-wax” appearance. It is a rare benign disease with an estimated incidence of 1: 1,000,000. The classic appearance exists only in less than half of the patients, making the atypical presentations confounding and can lead to delayed presentations and misdiagnosis. We here describe two distinct cases of melorheostosis, which represent the classic and atypical melorheostosis presentation.
Case Report: The first case presents as pain and limitation of hand motion, while the other case presents as an insidious pain of the foot. Both are managed surgically and with excellent outcomes.
Conclusions: Although melorheostosis is benign, other atypical types exist, with significant overlap with other conditions, especially malignancy. In some cases, the disease can result in debilitating chronic pain, deformity, and joint contractures leading to severe disability. Holistic and individualized management, including adequate pain control, physiotherapy, and surgical interventions, are required to address specific complaints and improve functional capacity.
Keywords: Melorheostosis, hand, foot, bone tumor, curettage
Melorheostosis is a rare, non-hereditary bony dysplasia of uncertain etiology. The name melorheostosis comes from the Greek words Melos, meaning limb, and rhein, meaning flow. This corresponds to the dripping candle wax appearance in radiographs. There are <400 cases published about melorheostosis, but localization to the hand is limited to around 30. Melorheostosis classically is more common in the younger population. Since it starts asymptomatically for long periods, presentation is delayed and sometimes detected incidentally [1]. Men and women are equally affected, and there is no proven hereditary tendency. The lower limb’s long tubular bones are most commonly affected. We describe a rare melorheostotic lesion of the hand involving multiple bones of the middle and ring finger rays with the classic dripping candle wax appearance and a fifth metatarsal melorheostotic lesion with an osteoma-like appearance. Herein, we examine these two cases of melorheostosis, correlate the distinct presentation and unique clinical and radiologic characteristics, and discuss the etiology, differentials, and treatment approaches with the currently available literature.
Case 1
A 79-year-old right-handed female was seen in the clinic for the gradual onset of pain and bony protuberances of the dorsum of the left hand (Fig. 1). The pain and limitation of motion worsened over time and eventually affected her daily activities. She did not report any numbness in the middle finger and index finger. There was no prior trauma history. She had surgery at another hospital 7 years ago, but the details were unknown.
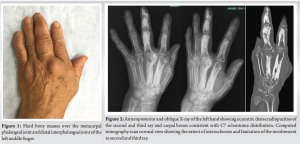
Physical examination revealed tender, hard bony protuberances at the dorsal-radial aspect of the distal interphalangeal (DIP) and the metacarpal phalangeal (MP) joint of the left middle finger. There is also a surgical scar at the dorsum of MP joint. Range of motion (ROM) was limited to 0–30°, while the DIP joint ROM was also restricted to 0–30°. There was no sensory disturbance. Laboratory findings were unremarkable.
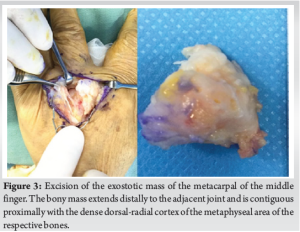
Radiographs revealed extensive hyperostosis at the distal, middle, proximal phalanges, and metacarpal of the middle finger. The middle, proximal phalanges, and metacarpal of the index finger are also involved. There are notable exostotic lesions over the dorso-radial aspect of the metacarpal head, the proximal and the middle phalangeal heads of the middle finger, causing impingement of the adjacent joints. Dense radiopacities are also appreciated at the carpal bones of the trapezoid, capitate, lunate, and scaphoid (Fig. 2). A computed tomography (CT) scan showed similar findings with dense osteosclerosis and hyperostosis of the second and third ray of the left hand. The dense cortical densities are found to extend to the intramedullary canal causing near obliteration of the medullary space. At the same time, the exostotic masses arise at the dorsal-radial aspect of the epi-metaphyseal area encroaching distally around the adjacent joint and superficially irritating the dorsal soft tissues. No joint involvement or soft-tissue masses were seen (Fig. 2).
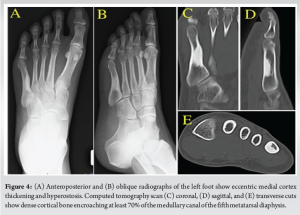
She underwent resection of the bony prominences to relieve the pain and to increase ROM of the MP and DIP joints of the middle finger (Fig. 3). The resection of the bony prominences at the metacarpal and middle phalanx was difficult due to the sclerotic change. Postoperatively, the pain was alleviated, and restricted ROM of the MP and DIP joints were immediately improved after surgery. On her latest follow-up at 6 months postoperatively, she maintained improved ROM with MP joint ROM of 0–70° and DIP joint ROM of 0–50°. The histopathologic examination result was osteochondroma due to the traces of cartilage at the periphery.
Case 2
A 46-year-old female came for pain over her left fifth metatarsal. One month before her initial consultation, she accidentally hit a shelf with the left fifth toe and was diagnosed with contusion by an orthopedic doctor. Radiographs showed an incidental abnormal finding on her left fifth metatarsal. At that time, there was no history of previous pain in the area. Her condition improved after the injury until the pain recurred in her left fifth toe, necessitating a referral to our department for further evaluation and treatment.
On her initial consult, she complained of pain in her left foot, causing her to limp. There were no other complaints, and the patient was otherwise in good health. On inspection, there were no skin changes, gross deformities, masses, swelling, edema, and erythema over the left foot. There was intense tenderness over the dorsal and lateral aspects of the left foot over the fifth metatarsal. The fifth metatarsophalangeal (MTP) joint has no limited ROM.
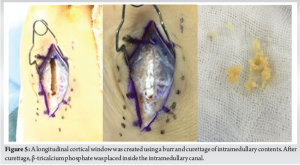
Radiographs revealed dense cortical bone formation along the medial aspect of the meta-diaphyseal area extending to the medullary canal of the fifth metatarsal. Eccentric hyperostosis was also appreciated in the medial cortex. CT scan revealed intraosseous compact bone growth and hyperdense sclerotic lesions along the medial cortex encroaching at least 70% of the intramedullary space with narrowing of the canal of the meta-diaphyseal area of the fifth metatarsal. There was also associated bulging of the medial cortex (Fig. 4). Magnetic resonance imaging (MRI) showed low-signal intensity lesions in the intramedullary cavity in both T1- and T2-weighted MR sequences, suggesting mineralized areas. There was no marrow edema, soft-tissue masses, muscle atrophy, and joint abnormalities.
The patient was initially given a non-steroid anti-inflammatory drug; however, it did not relieve her pain. She then underwent surgery for biopsy and curettage. A cortical window was created utilizing an airtome dorsally, and findings revealed yellow, hard bony tissue inside her medullary canal. It was then curetted off, and the medullary canal was loaded with β-tricalcium phosphate (β-TCP) (Fig. 5).
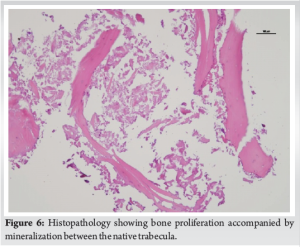
Her pain was relieved immediately after surgery, and she was pain-free 6 months after surgery. A plain X-ray showed that the β-TCP was slowly being resorbed and replaced by new bone. The post-operative histopathological tissue showed bone proliferation accompanied by mineralization between the native trabecula. These pathological findings seemed to be consistent with previous reports (Fig. 6).
Etiology
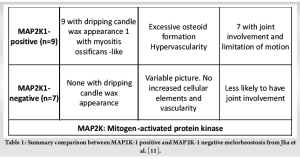
The etiology of melorheostosis remains poorly understood to date. The sclerotome hypothesis suggests that an infection, a vascular or an inflammatory insult to the segmental sclerotome before limb bud formation in the neural crest explains the obscure distribution pattern [1]. The distribution pattern for Case 1 is at the C7 sclerotome, while in Case 2 is at the S1 sclerotome. The mosaicism theory surmised that the sporadic occurrence and variable involvement could be explained by an early post-zygotic mutation of the mesenchyme [2]. Jha and colleagues in 2018 proposed a clonal proliferation theory in which the mutation could have happened during limb bud development and assignment of the anteroposterior (dorsoventral) elements in the limb bud mesenchyme [3]. Some authors describe an association with the LEM domain containing 3 genes (LEMD3) gene mutations found in familial sclerosing dysplasias, including osteopoikilosis and Buschke-Ollendorff syndrome [4]. However, recent molecular analyses have shown that LEMD3 mutations do not result in isolated melorheostosis [5]. Recent molecular analysis has elucidated that classic melorheostosis results from a somatic activating mutation in Mitogen-Activated Protein Kinase Kinase 1 (MAP2K1) [6]. This genetic heterogeneity translates to phenotypic heterogeneity from the histopathologic level and ultimately to the final clinical presentation (Table 1).
Clinical Presentation and radiologic findings
The clinical presentation in Case 1 is primarily pain and stiffness related to the exostotic lesion and juxta-articular extension. In a series of 24 patients studied by Smith et al., the most common complaint is pain (83%), followed by deformity (54%), limitation of movement (45%), numbness, and weakness (25%) [7]. The pain can be nociceptive, neuropathic, or skeletal. The nociceptive pain is related to the soft-tissue inflammation resulting from compressions, as in Case 1. The skeletal pain comes from the extensive hyperostosis that probably resulted from increased intraosseous pressure, as in Case 2.
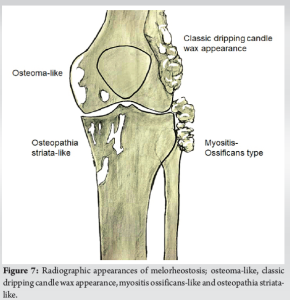
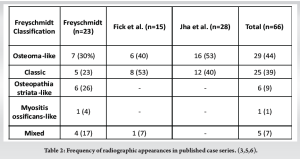
Radiographic findings have been the cornerstone of the diagnosis, but atypical presentations are a source of confusion. [4,8,9]. Freyschmidt suggested five identifiable patterns of radiographic appearances. These are the five types; osteoma-like, classic dripping candle wax appearance, myositis ossificans-like, osteopathia striata-like, and mixed [9] (Fig. 7). According to multiple case series, the radiographic appearance in Case 1, which is the classic type, and the radiographic appearance in Case 2, which is the osteoma-like type, constitute the most common of all the radiographic appearances of melorheostosis (Table 2).
CT scan helps to define the extent of the disease, joint involvement, and presence of soft-tissue ossification. The value of MRI rests in its ability to delineate soft-tissue involvement and bone marrow edema. For Case 1, a CT scan and MRI clarified the relationship between the exostosis’s juxta-articular extension. For Case 2, cross-sectional imaging helped rule out important differential diagnoses like osteoid osteoma and potential malignancies.
Histopathology
The histopathology of melorheostosis is variable, with common histologic patterns such as increased cortical density, woven bone, osteoid deposition, and vascularity. Fick et al. found that it can present with dense cortical bone, woven bone, hypervascularity, and periosteal fibrous thickening [10]. Although these histologic features are not pathognomonic to melorheostosis, a biopsy is still necessary to rule out malignant features.
Differential diagnosis
Classic melorheostosis can be easily identified by its radiographic appearance alone. Diagnosis of melorheostosis in Case 1 was considered due to its classic melting candle wax appearance. Due to the presence of exostosis, osteochondroma is a critical differential. Osteochondroma presents as a hard, palpable mass that can also cause impingement of nearby structures, bursitis, and osteoarthritis. Characteristically, osteochondromatous exostosis usually grows away from the nearby joint, which is not the case in melorheostosis. Although traces of cartilage were appreciated in the histologic examination in Case 1, which can be confused with the cartilage cap in osteochondroma, the juxta-articular nature of the melorheostotic lesion can result in the presence of cartilage. In Case 2, the endosteal sclerosis of the fifth metatarsal was initially considered an osteoid osteoma. The hallmark of osteoid osteoma radiographically is the presence of sclerosis with a central radiolucent nidus zone surrounded by dense bone. However, in small bones, especially in the medullary osteoid osteoma type, it can be difficult to appreciate a nidus, especially in the early stages [11]. CT scan and MRI in Case 2 failed to show a nidus and any periosteal and bone marrow changes. Additionally, histopathology showed no nidus and bone edema consistent with osteoid osteoma.
An enostosis or a bone island radiographically looks similar to osteoma-like melorheostosis in Case 2. Enostosis presents as solitary oval, round, or dense oblong sclerosis consisting of a focus of cortical bone within the cancellous bone with peripheral radiating bony spicules (“rose thorns”). However, it is typically metabolically inactive, nearly always asymptomatic, and does not grow in size. Atypical enostoses presenting with pain, tenderness, or enlargement can occur, but this needs to be differentiated from other entities necessitating bone scan, CT scan, and biopsy [12].
Treatment
Treatment is variable and depends on the symptoms and consequent disability. In a case series by Jha et al., patients with lesions of the hand or foot (in contrast to arm and leg) experience greater functional limitations and more significant occupational disability. Some case reports showed improvement for non-operative treatment after administering zoledronic acid denosumab as second-line treatment [13], but we had no experience. Surgical management is individualized depending on patient complaints and findings. For exostotic lesions, such as in Case 1, excision relieves the pain and improves the ROM. It is essential to highlight that decompression is an effective treatment option for relieving extreme pain brought about by melorheostosis. In both cases, intractable pain was the significant complaint due to increased intraosseous pressure, and dramatic pain relief was achieved through decompression, debulking, or cortical window with intramedullary curettage. Freyschmidt [9] and Lan et al. [14] suggested fenestration of melorheostotic bone to relieve intraosseous pressure. It is also essential that regular follow-ups are employed to monitor the progression of the disease and the recurrence of the symptoms. Even though melorheostosis is a benign condition and degeneration is not a feature, some reports of osteosarcoma concurrent with melorheostotic lesions exist [15].
We here have described two distinct cases of melorheostosis, which represent the classic and atypical melorheostosis presentation. One case had a lesion of the hand involving multiple bones of the middle and ring finger rays with the classic dripping candle wax appearance. Another had a fifth metatarsal melorheostotic lesion with an osteoma-like appearance. Holistic and individualized management, including adequate pain control, physiotherapy, and surgical interventions, are required to address specific complaints and improve functional capacity.
Melorheostosis is a rare benign disease with an estimated incidence of 1: 1,000,000. Melorheostosis was described as a “dripping candle-wax” appearance in radiographs. However, the classic appearance exists only in less than half of the patients, making the atypical presentations confounding and can lead to delayed presentations and misdiagnosis. Orthopedic surgeons should know the existence of this rare and unique condition.
References
- 1.Murray R, McCredie J, Murray RO. Skeletal radiology melorheostosis and the selerotomes: A radiological correlation. Skeletal Radiol 1979;4:57-71. [Google Scholar]
- 2.Fryns JP. Melorheostosis and somatic mosaicism. Am J Med Genet 1995;58:199. [Google Scholar]
- 3.Jha S, Laucis N, Kim L, Malayeri A, Dasgupta A, Papadakis GZ, et al. CT analysis of anatomical distribution of melorheostosis challenges the sclerotome hypothesis. Bone 2018;117:31-6. [Google Scholar]
- 4.Hellemans J, Preobrazhenska O, Willaert A, Debeer P, Verdonk PC, Costa T, et al. Loss-of-function mutations in LEMD3 result in osteopoikilosis, Buschke-Ollendorff syndrome and melorheostosis. Nat Genet 2004;36:1213-8. [Google Scholar]
- 5.Mumm S, Wenkert D, Zhang X, McAlister WH, Mier RJ, Whyte MP. Deactivating germline mutations in LEMD3 cause osteopoikilosis and Buschke-Ollendorff syndrome, but not sporadic melorheostosis. J Bone Miner Res 2007;22:243-50. [Google Scholar]
- 6.Jha S, Fratzl-Zelman N, Roschger P, Papadakis GZ, Cowen EW, Kang H, et al. Distinct clinical and pathological features of melorheostosis associated with somatic MAP2K1 mutations. J Bone Miner Res 2019;34:145-56. [Google Scholar]
- 7.Smith GC, Pingree MJ, Freeman LA, Matsumoto JM, Howe BM, Kannas SN, et al. Melorheostosis: A retrospective clinical analysis of 24 patients at the mayo clinic. PM R 2017;9:283-8. [Google Scholar]
- 8.Rozencwaig R, Wilson MR. Melorheostosis of the skeletally immature hand: A case report and long-term follow-up evaluation. J Hand Surg Am 1996;21:703-6. [Google Scholar]
- 9.Freyschmidt J. Melorheostosis: A review of 23 cases. Eur Radiol 2001;11:474-9. [Google Scholar]
- 10.Fick CN, Fratzl-Zelman N, Roschger P, Klaushofer K, Jha S, Marini JC, et al. Melorheostosis a clinical, pathologic, and radiologic case series. Am J Surg Pathol 2019;43:1554-9. [Google Scholar]
- 11.Hashemi J, Gharahdaghi M, Ansaripour E, Jedi F, Hashemi S. Radiological features of osteoid osteoma: Pictorial review. Iran J Radiol 2011;8:182-9. [Google Scholar]
- 12.Bedard T, Mohammed M, Serinelli S, Damron TA. Atypical enostoses-series of ten cases and literature review. Medicina (Lithuania) 2020;56:1-12. [Google Scholar]
- 13.Sathish M, Girinivasan C, Srinivasacholan C, Gowtham P. Bisphosphonate therapy in the management of symptomatic melorheostosis of Tibia. J Orthop Case Rep 2021;11:103-6. [Google Scholar]
- 14.Lan H, Yin DZ, Xin XT, Chen C, Liu B. Knee melorheostosis treated by drilling fenestration: A case report. Orthop Surg 2012;4:122-4. [Google Scholar]
- 15.Brennan DD, Bruzzi JF, Thakore H, O’Keane JC, Eustace S. Osteosarcoma arising in a femur with melorheostosis and osteopathia striata. Skeletal Radiol 2002;31:471-4. [Google Scholar]











